Review Article - Volume 2 - Issue 4
Telepharmacy in sub-Saharan Africa: A Narrative Review
Nwaodu Mercy Adamma1; Ogbonna Brian Onyebuchi1,2*; Anetoh Maureen Ugonwa1; Ejieh Loveth1; Okpalanma Nneoma3; Maduekwe Hilda3; Okeke Anthony4; Okoye Ifunanya3; Omuta Michael Chukwuemeka4;Egere Eustace Chijioke4; Osuafor Nkeiruka Grace4; Maduka Anthony4; Ovwighose Samuel4; Nnamani Monica4; Ajagu nenna5; Ofor Amala5
1Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University,Awka, Nigeria.
2Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, King David University of Medical Sciences, Uburu,Nigeria.
3Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Chukwuemeka OdimegwuOjukwu University Igboariam Nigeria.
4Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Madona University, Elele Nigeria.
5Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Enugu State University of Sience and Technology, ESUT- Enugu.
Received Date : June 14, 2022
Accepted Date : July 11, 2022
Published Date: July 31, 2022
Copyright:© Ogbonna Brian 2022
*Corresponding Author : Ogbonna Brian O, Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences,Nnamdi Azikiwe University, Awka, Nigeria.
Email: bo.ogbonna@unizik.edu.ng
DOI: Doi.org/10.55920/2771-019X/1203
Abstract
Introducion: In light of the COVID-19 pandemic, there have been developments to ensure patient care even with distance as a barrier. In line with this, Telepharmacy has been receiving much focus, however, there is sparse information on its practice in Sub-Saharan Africa, thus, necessitating the study. This study described the trends and dynamics of Telepharmacy in SubSaharan Africa.
Methods: The study utilized narrative review to explain the state of Telepharmacy in Sub-Saharan Africa. Literature were retrieved from computerized databases using related search terms. Data obtained was entered into Microsoft Excel Work sheet and summarized using descriptive statistics in frequency and percentages.
Results: A total of 6 publications from a total of 140 was selected (0.043% selection rate). All selected articles fell after the year 2000, indicating the field is still novel. Most of the selected studies were also commentaries as opposed to observational studies.
Conclusion: There is a dearth of studies relating to Telepharmacy in Sub-Saharan Africa, thus, it is a minefield which researchers can explore for further studies.
Keywords: Telepharmacy; Pharmacy Practice; Pharmaceutical Care; Sub- Saharan Africa.
Introduction
Over the years, technology has impacted many spheres of life with the major aim of creating a positive transformational effect. The 20th century was met with an expansion in the use of information and communication technologies, which strongly influenced healthcare delivery not just in developed countries, but also in developing countries. Technology in healthcare has attempted to address the issues of equity, quality, access, cost-effectiveness and other problems associated with health care in countries around the globe [1]. However, with the ever-increasing population explosion, fueled by rural-urban migration and a constant dwindling healthcare workforce, Telepharmacy has been an enabling tool in health technology that bridges the gap between Pharmacists and patients. To address the shortage of health workers’ crisis, an acute situation faced mostly in Sub-Saharan Africa, the World Health Assembly (WHA), in 2005 passed a resolution urging countries to adopt the use of eHealth to strengthen their health system. In 2006, the WHA encouraged WHO member states to use ICT in addressing global shortage of workers [2].
Telehealth is an encompassing term that considers the application of technology on all aspects of health, i.e., providing healthcare through a virtual interface. These include, but is not limited to: Teleradiology, Telenursing, Telepharmacy, Telepsychiatry, Teledermatoogy, Telemedicine etc. However, in some works of literature, Telemedicine is used interchangeably with Telehealth [3]. The National Association of Boards of Pharmacy defines Telepharmacy as “the provision of pharmacist care by registered pharmacists and pharmacies through the use of telecommunications and information technologies to patients located at a distance” [4, 5]. Telepharmacy harnesses technology to provide services like patient assessment, Medication refill, Patient education and counselling, Drug information services, Therapeutic drug monitoring etc. [6]. In spite of numerous advantages of Telepharmacy such as decreased hospital visits, reduced traveling expenses, improved pharmacist-patient relationship, improved drug therapeutic monitoring, and a decrease in actual and potential drug therapy problem [7], the major constraint remains the issue of confidentiality, privacy, and security threats of health information. Thus, regulations and laws ensuring such must be put in place to curb these. Patients’ information can also be encrypted and consent should be received from them before proceeding with the voice or video call [6]. This study described the trends and dynamics of Telepharmacy in Sub-Saharan Africa.
Methods
Study Area
The study covered prior works related to Telepharmacy in Sub-Saharan Africa with no specified date limit.
Review Question
What are the trends and dynamics of Telepharmacy in Sub-Saharan Africa?
Study Population and Type of Study Included
Studies that passed the eligibility criteria and were found in databases such as Google Scholar and PubMed were included in the study.
Eligibility Criteria
- Studies published in English Language
- Studies related to Telepharmacy carried out in Sub-Sahara Africa
- Studies with clearly defined protocol and study design
- Studies with no conflict of interest stated
Ineligibility Criteria
- Studies not published in English Language
- Studies outside the scope of the study
- Studies with methodological flaws
- Studies with conflict of interest stated
Study Design
Study was a narrative overview of studies pertaining to Telepharmacy in Sub-Saharan Africa.
Information Source
Literature search was conducted using Google Scholar and PubMed.
Articles Search Process
This research reviewed relevant journals and articles on Telepharmacy that have considered the body of Sub-Saharan African countries as an entity or as a whole. The search terms included key words, set of synonyms and variation in combination of keywords relating to Telepharmacy in Sub-Saharan Africa. The whole research, for reviewed literature, was finalized after two months and two main databases were considered, namely: Google Scholar and PubMed; abstracts and full-text articles were obtained. A total of 6 articles were obtained relating to Telepharmacy in Sub-Sahara Africa, from Google scholar and PubMed (Figure 1). These articles were then assessed for eligibility. These databases were selected for based on convenience and ease of access.
Study Period and Duration
The study lasted from December 2021 to February 2022.
Ethical Approval
No Ethical Approval was obtained for the study.
Study Articles Selection Process
A total of 140 articles were obtained relating to Telepharmacy: 78 from Google scholar, and 62 from PubMed. These were assessed based on the eligibility criteria. Duplicate articles were removed and on further screening, a total of 6 articles were used for the review.
Data Analysis
For the bibliographic analysis, data extracted from the selected articles were entered into a spreadsheet for statistical analysis (Microsoft Office Excel, Windows 10 version). The variables registered for each article were: Reference, Title, Year of publication, Geographical zone, Study design and Sample size. Descriptive analyses of the relevant study variables were undertaken and the results were summarized in tables and figures.
Flow Chart of Study Process
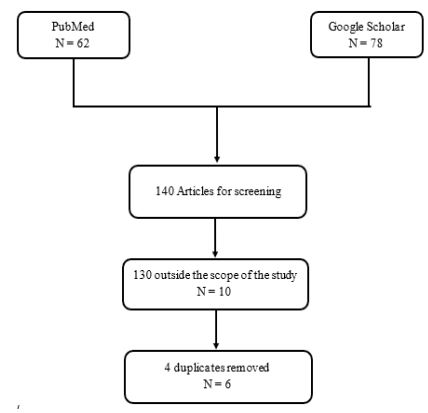
Figure 1: Flow Chart of the study articles selection process.
Results
Table 1: Characteristic distribution of selected study.
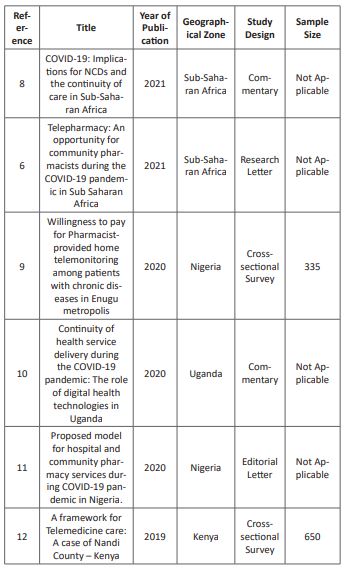
Table 2: Periodic distribution of the articles
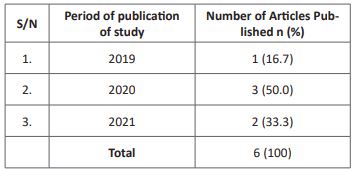
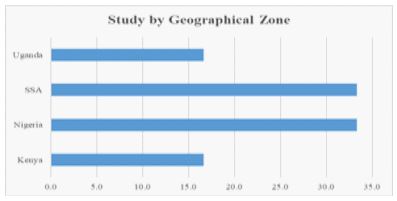
Figure 2: Geographical spread of study
Discussion
Trends and Dynamics of Telepharmacy in Sub-Saharan Africa
The distribution of the study revealed a high incidence of non-experimental studies as the study design was predominantly editorial letters or commentaries. One can thus infer that the practical application of this model of pharmacy has not been fully integrated into the healthcare system in most Sub-Saharan African countries which is similar to most developing countries. As seen, however, from the date of publication of these articles, it can be inferred that the COVID-19 pandemic brought unprecedented transformation to the healthcare system, as this model of pharmacy began to receive much focus, as it is also a means of bridging the gap between Pharmacists and patients, even while ensuring ‘social-distancing’, thus reducing infection rate whilst receiving proper pharmaceutical care. The recent date of these published work is quite understandable because the concept of Telepharmacy, although conceptualized as far back as 1942 in Australia, did not receive appropriate recognition until 2001 when the first attempt to regulate it was made by the Board of Pharmacy, North Dakota in the United States of America. Ethical considerations, high startup cost, as well as a host of other factors, have delayed its applications in developing countries [6, 13].
Currently, there is no regulatory framework for the implementation of Telepharmacy, leading to reliance on regular licenses. 92% of countries in Africa indicated the absence of laws governing online Pharmacy practice even those offering a form of Telepharmacy services [14]. In Nigeria, the National Information Technology Development Agency (NITDA), the Ministry of Health and the Ministry of Communications have begun working with Entrepreneurs interested in health technology to develop a policy document [15]. In addition, the registrar of the Pharmacists Council of Nigeria, Elijah Mohammed, charged the council to do a thorough work regarding regulations of online pharmacies, also stating that every certified online pharmacy should have a Telepharmacy component [16]. This will go a long way in ensuring its integration more into the healthcare system.
Extent and Nature of Work Done in Sub-Saharan Africa
Findings obtained indicate that majority of the studies were a call to action and not actual applications of this model of Pharmacy in healthcare, hence, the need for practical approaches, to be able to compare outcomes between Telepharmacy model and Traditional Pharmacy model. Focus of study bordered on Telemedicine, as a general term to address other forms of telehealth with minor specificity to Telepharmacy. This may not necessarily be because Telepharmacy is not practiced but could be as a result of lack of documentation, hence, dearth of published works. From Table 1, it is seen that majority of the study were commentaries or review/editorial letters. The surveys recorded however addressed different study populations. According to findings by Anosike et al [9] less than half of the population (patients) were willing to pay for a pharmacist-provided home telemonitoring services as majority cited the inability to pay for this service as the reason for their unwillingness as poor income level is a major factor plaguing most developing countries. To manage this issue, it was suggested that the government include charges for this service as tax or in health insurance schemes to ensure patients benefit from this service [9]. The study carried out in Nandi County, Kenya by Amdany et al. revealed that 54.5% of the healthcare workers perceived Telepharmacy as a critical emergency healthcare need, as such, necessary in the health facilities. This also goes to show that Telepharmacy is not just a retail pharmacy concept but is also applicable in a hospital setting [12].
There has been a disruption in care since the COVID pandemic begun as Clinics focused on COVID cases and paid lesser attention to patients coming in with other complaints. This has led to an increase in the prevalence of Non-Communicable Diseases in Sub-Saharan Africa, as such, Telepharmacy was one of the solutions proffered to support e-prescribing thus ensuring continuity of care [8]. In Uganda, medicine delivery services to preferred locations were also incorporated with positive feedback from patients [10]. Hedima & Okoro saw the pandemic era as an opportunity for telehealth improvement in Sub-Saharan African countries, although not without its challenges. Some challenges to Telepharmacy highlighted includes, but not limited to confidentiality and security threat to patients’ data which can be curtailed with appropriate rules and regulations put in place by the government [6].
Currently, the focus is majorly on Online Pharmacy which concentrates on sales and delivery of drugs. However, some online platforms are gradually delving into an aspect of Telepharmacy by providing patients with the option of speaking directly with a Pharmacist (Consultation) from the comfort of their homes. David and Adebisi proposed complementing Telepharmacy with home delivery of medication as well as collaboration with other healthcare professionals [11]. This is a welcome development, although, regulations need to be set in place to ensure only licensed pharmacists with the ability of providing proper drug information are allowed to practice, as the danger of misinformation may be more critical than the current health challenge the patient is facing. One such example of such development is One- Health, amongst many others which are currently increasing on a daily basis. These services are offered on a subscription basis and with the aid of a health analytic dashboard, users can also monitor their health status and progress. Though this platform is not without its challenges, it is seeking for ways to partner with existing Health Maintenance Organizations (HMOs), where its services could be offered to patients with chronic ailments [17].
Conclusion
With more people delving into technology, regardless of their previous discipline, people are becoming more inspired to provide means to make life better using technological means, the pharmaceutical industry is not an exception. As no discovery is without challenges, there is however hope that in the nearest future, Telepharmacy will be implemented at a larger scale, not just in developed, but also in developing countries, with the primary goal of ensuring health for all.
Limitation of study
As most of the search was related to telemedicine, some relevant articles which could have contained details pertaining to Telepharmacy in Sub-Saharan Africa may have been omitted. Omissions may have also been made due to search and search terms limitations.
Funding: No funding was received for this study.
Conflict of interest: The author declares no competing interests
References
- Igharo V. Improving Access to Medicines through Integrated Technologies. Pharmaceutical Sector Paper. 2013 August; 2: 1-8.
- Asamoah-Odei E, De Backer H, Dologuele N, Embola I, Groth S, Horsch A, et al. eHealth for Africa Opportunities for enhancing the contribution of ICT to improve health services. Eur J Med Res. 2007; 12 (1): 1-38.
- Kerna NA, Carsrud NDV, Pruitt KD, Kadivi K, Gutierrez YP, Jones, D et al. Telehealth and Telemedicine: A Practical review (Including applications for COVID-19). EC Clinical and Medical Case Reports. 2021; 4(5): 07-14. [DOI:10.31080/eccmc.2021.04.00389].
- Win AZ. Telepharmacy: time to pick up the line. Res Social Adm Pharm. 2017; 13: 882–883.
- Casey MM, Sorensen TD, Elias W, Knudson A and Gregg W. Current practices and State regulations regarding telepharmacy in rural hospitals. Am J Health Syst Pharm. 2010; 67(13): 1085.
- Hedima EW and Okoro RN. Telepharmacy: An opportunity for community pharmacists during the COVID-19 pandemic in Sub Saharan Africa. Health Policy Technol. 2021; 10(1): 23-24. [DOI: 10.1016/j.hlpt.2020.10.013].
- Nittari G, Khuman R, Baldoni S, Pallotta G, Battineni G, Sirignano A, Amenta F and Ricci G. Telemedicine practice: Review of the current ethical and legal challenges. Telemed J E Health. 2020; 26(12): 1427-1437. [DOI:10.1089/tmj.2019.0158].
- Owopetu O, Fasehun L and Abakporo U. COVID-19: Implications for NCDs and the continuity of care in Sub-Saharan Africa. Global Health Promotions. 2021; 28(2): 8-86. [DOI:10.1177/1757975921992693].
- Anosike C, Adibe MO, Isah A and Ukoha-Kalu OB. Willingness to pay for Pharamacist-provided home telemonitoring among patients with chronic diseases in Enugu metropolis. Health Informatics Journal. 2020; 26(2): 829-840. [DOI: 10.1177/1460458219852534].
- Kamulegeya LH, Bwanika JM, Musinguzi D and Bakibinga P. Continuity of health service delivery during the COVID-19 pandemic: The role of digital health technologies in Uganda. Pan Africa Medical Journal. 2020; 35(2):43. [DOI: 10.11604/pamj.supp.2020.35.2.23115].
- David KB and Adebisi Y A. Proposed model for hospital and community pharmacy services during COVID-19 pandemic in Nigeria. Int J Pharm Pract. 2020; 22: 544-545. [DOI: 10.1111/ijpp.12652].
- Amdany S, Olouch JO and Abila JO. A framework for Telemedicine care: A case of Nandi County – Kenya. International Journal of Innovative Science and Research Technology. 2019; 4(11): 269-267.
- Margolis SA and Ypinazar VA. Telepharmacy in remote medical practice: The Royal Flying Doctor Service Medical Chest Program. Rural Remote Health. 2008; 8: 937.
- International Pharmaceutical Federation. Online pharmacy operations and distributions of medicines. The Hague, The Netherlands: International Pharmaceutical Federation. 2021.
- Agbakoba-Onyejianya B and Aka-Bashorun O. Health Tech in Nigeria: A Legal Perspective; 2019.
- Uche H. Online Pharmacy Regulations: ‘Do a thorough work’; 2021.
- Okwumbu-Imafidon, R. How One Health is taking pharmacare digital in Nigeria – Deola Alli, CEO. 2021.

