Case Report - Volume 2 - Issue 4
Unsuspected Low Grade Endometrial Stromal Sarcoma-Clues to Improve Preoperative Diagnosis
Mamta Mishra*; Neema Sharma; Shreeja Jha; Nitin Dumeer; Shoma
Department of Obstetrics and Gynecology, Fortis hospital, India
Received Date : June 13, 2022
Accepted Date : July 06, 2022
Published Date: Aug 01, 2022
Copyright:© Mamta Mishra 2022
*Corresponding Author : Mamta Mishra, Department of Obstetrics and Gynecology, Fortis hospital, India.
Email: drmmishra12@gmail.com
DOI: Doi.org/10.55920/2771-019X/1204
Abstract
Endometrial stromal tumours are extremely rare, having an incidence of one to two from a million of women Preoperative diagnosis is difficult and most often diagnosis is established after surgery. We report a case where low-grade endometrial sarcoma was diagnosed after hysterectomy in a young woman. Retrospectively we analysed to look for clues which could help to improve preoperative diagnosis.
Introduction
Low grade endometrial stromal sarcoma (LG-ESS) is a rare malignant neoplasm of the uterus. Incidence is one to two from a million of women [1]. Endometrial stromal tumours have been classified by WHO as benign stromal nodule and endometrial stromal sarcoma (ESS). It is further classified based on mitotic count and cell morphology into low grade ESS and high-grade ESS [2]. It commonly presents as abnormal uterine bleeding and pelvic pain. However, it can present as uterine mass and metastases to the adnexa, lymph nodes and lungs. It’s a slow growing tumour and recurrences either local and distant can occur even after 20 years Pre-operative diagnosis is extremely difficult. Ultrasound can easily misdiagnose it as fibroid, adenomyosis or polyp.
Case
A 32-year-old P2 woman presented with secondary dysmenorrhea since last 6 month. She also had recently developed prolonged and intermenstrual bleeding. Due to covid she delayed medical consultation initially. However, her pain gradually worsened each cycle. She used to take injectables diclofenac sodium for pain relief for 6-7 days each cycle. On examination – her vitals were stable However, she looked pale. Abdominal examination revealed a 14-week-pregnancy-sized, non-tender, firm mass with regular margins and arising from the pelvis. Per vaginum examination confirmed that uterus was enlarged, of 14 weeks size and mobile. USG done revealed 5 x3.5 x4.8 cm submucosal fibroid. MRI was done which also confirmed submucosal fibroid. Her hemoglobin was 10.0gm/dl. CA 125 and LDH were45IU/dl and 250 respectively. Pain was disproportionate to clinical and ultrasound finding. Strategies to conserve uterus was discussed. However, as the pain was severe and small chance of recurrence of fibroid was there, she insisted for hysterectomy. Total Laparoscopic hysterectomy with conservation of tubes and ovaries was done on16.12.20.
Histopathology, showed a tumor with infiltrating margins into the myometrium characterized by tongue like extensions. Mitotic activity was low (<5/10hpf). No necrosis was seen. It was suggestive of low-grade endometrial sarcoma. Immunohistochemistry was done. Vimentin was diffuse and strong positive in tumors cells.CD10 and proliferative marker KI67 was also positive whereas desmin and H Cal Desmon were negative. A multidisciplinary meeting was done and it was decided to do bilateral salpingoohrectomy. Laparoscopic bilateral salpingoohrectomy was done on 05.01.2021. Histopathology of tubes and ovaries were unremarkable. One year after surgery patient is absolutely fine.
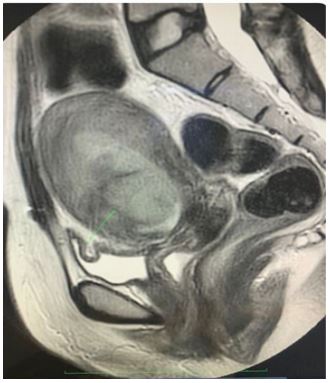
Saggital T2 image showing a hyperintense mass
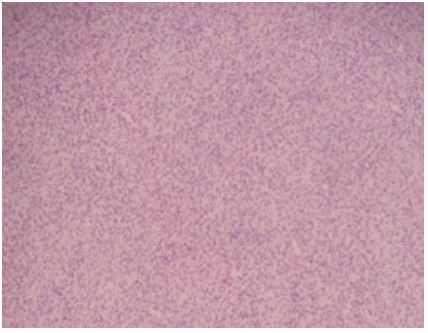
H&E 10X Tumor showing tumor cells with ovoid nuclei and minimal mitotic activity.
Entrapped spiral arterioles seen.
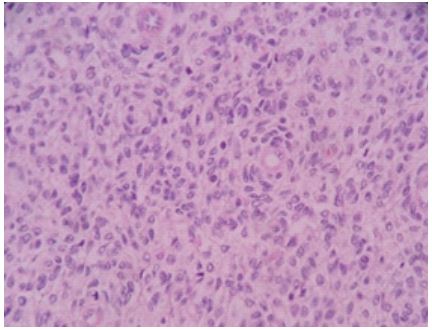
H&E 20X
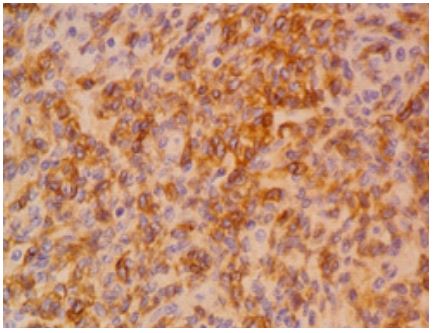
IHC CD-10 Diffuse uniform strong positive in tumor cells.
Discussion
The prevalence of unsuspected sarcoma to be 1 in 352 women and the risk of leiomyosarcoma to be 1 in 498 in women with presumed fibroids [3]. It is not uncommon to misdiagnose low grade stromal tumor as leiomyoma preoperatively. This can lead to opt for conservative approach such as delaying treatment, opting medical management or myomectomy and morcellation rather than hysterectomy. So, is there a possibility to improve diagnosis preoperatively.
Clinical findings
Abnormal vaginal bleeding and pelvic pain are nonspecific symptoms which are commonly present in both fibroids and uterine cancer. In our case Pain was very severe, of short duration and was worsening each cycle. In fact, decision to do hysterectomy was taken mainly because of severe pain.
Serum Markers
Only a small number of studies are currently available that evaluate the use of serum markers in predicting uterine cancer, and none have been reliable. Mostly, studies are done to correlate CA125 and LDH with leiomyosarcomas not endometrial stromal sarcoma [4]. In our case CA125 and LDH were mildly raised. Although, nonspecific but does appear significant when analyzed retrospectively.
Imaging
Ultrasound is not a good modality to distinguish between leiomyoma and endometrial stromal sarcoma. MRI findings were evaluated again so as to improve the preoperative diagnosis.
MRI
Magnetic resonance imaging can be useful for a preoperative diagnosis [5]. It can alert us to leiomyoma variants and possibly endometrial stromal sarcoma. In our case it revealed polypoidal circumscribed mass arising from anterior myometrium projecting into the endometrial cavity, it has well defined margin appears isointense on t1 sequence, hyperintense on T2 weighted images with restricted diffusion. Contrast images show moderate homogenous enhancement within the mass and the presence of a thin enhancing capsule. The important feature in MRI is the presence of bands of low-signal intensity within the area of myometrial invasion. This is due to the worm-like permeation of tumour cells into the myometrium. Leiomyoma on the other hand shows low t2 signal similar to myometrium often with inner whorled and nodular structure. However, leiomyoma can have variable appearance on MRI depending on cellularity and presence of degeneration, necrosis and calcification. Decision to do hysterectomy was difficult and was taken in view of severe pain. Later on it turned out to be a wiser move.
Conclusion
Low grade endometrial stromal sarcoma is a rare pathology more so in young woman. However, awareness about it is essential for the clinician for proper counselling and management. High degree of suspicion along with subtle signs may help to diagnose it preoperatively.
References
- Puliyath G, Nair MK. Endometrial stromal sarcoma: A review of the literature. Indian J Med Paediatr Oncol. 2012; 33(1): 1-6.
- Jain R, Batra S, Ahmad A, Elahi AA,et al. Low grade endometrial stromal sarcoma: a case report. Iran J Med Sci. 2015; 40(1): 81-84.
- 3 Pritts EA, Vanness DJ, Berek JS, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015; 12(3): 165-177.
- Babacan A, Kizilaslan C, Gun I, et al CA 125 and other tumor markers in uterine leiomyomas and their association with lesion characteristics. Int J Clin Exp Med. 2014; 7(4): 1078-1083.
- Himoto Y, Kido A, Sakata A,et al. Differentiation of uterine low-grade endometrial stromal sarcoma from rare leiomyoma variants by magnetic resonance imaging. Sci Rep. 2021 Sep 27; 11(1).

