Case Report - Volume 2 - Issue 5
Inflammatory pseudotumor-like follicular dendritic cell sarcoma with first clinical manifestation of thrombocytopenia: a case report
Dong-Li Leng1; Kang-Jie Yu1 and Jing Wang2*
1Pathology department, Nanjing JunXie Hospital, Nanjing, Jiangsu Province 210002, China.
2Translational Medicine Center, Nanjing JunXie Hospital, Nanjing, Jiangsu Province 210002, China
Received Date : July 19, 2022
Accepted Date : Aug 20, 2022
Published Date: Sep 06, 2022
Copyright:© Jing Wang 2022
*Corresponding Author : Jing Wang, Translational Medicine Center,Nanjing JunXie Hospital, 32# Ma-Lu street, Nanjing, Jiangsu Province 210002, China.
Email:wj6373@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1235
Abstract
Inflammatory pseudotumor-like follicular dendritic cell sarcoma (IPT-like FDCS) is often associated with Epsrein-Barr (EB) virus infection. A male patient visited our hospital in September 2020 due to bleeding gums and epistaxis. The initial diagnosis was splenic lymphoma with marked thrombocytopenia. The patient was sent for pathological examination after splenectomy. Microscopic examination showed spindle-shaped or oval cells arranged in loose bundles, a large number of lymphocytes and plasma cells infiltrated in the interstitium, and fibrin-like changes in the blood vessel wall. Immunohistochemical detection of tumor cells was positive for CD21, CD35 and EBER, and we diagnosed IPT-like FDCS. The patient received platelet-raising therapy after operation. No tumor recurrence or metastasis was found during the 17-month follow-up, and the platelets returned to normal.IPT-like FDCS is an uncommon tumor, and the first presentation with marked thrombocytopenia is even rarer. The tumor was clinically and radiographically nonspecific. Its definitive diagnosis needs to rely on histopathological and immunohistochemical staining. IPT-like FDCS is biologically indolent and has a good prognosis.
Keywords: Inflammatory pseudotumor-like follicular dendritic cell sarcoma; Epstein–Barr virus; thrombocytopenia; Case report.
Introduction
Follicular dendritic cell (FDC) sarcomas are often confused with other tumors and even inflammatory processes. Diagnosis requires the use of broad-spectrum FDC markers (eg, CD21, CD23, CD35, clusterin, CXCL13, podoplanin), especially given that tumor antigen loss is common. It can be divided into two types: conventional FDC sarcoma and inflammatory pseudotumor-like follicular dendritic cell (IPT-like FDC) sarcoma. In addition to its unique histopathological and clinical features, IPT-like FDCs also have the characteristic that tumor cells are positive for Epstein-Barr virus, which is necessary for diagnosis [1,2]. IPT-like FDC sarcoma is a very rare solid tumor with a favorable prognosis that usually occurs in the spleen and can involve other anatomical sites, including the liver and pancreas. The tumor tends to develop in young and middle-aged adults and may present with a variety of symptoms, including fever, abdominal pain, sweating, fatigue, and more commonly, a solitary lesion of the spleen. This sarcoma is a neoplastic spindle cell lesion, usually with follicular dendritic cell differentiation. It has been reported in the literature that paraneoplastic pemphegus (PNP), myasthenia gravis (MG) and other diseases can be combined, and more than 90% of the cases are associated with Epstein-Barr virus (EBV) [2,6]. The diagnosis of IPT-like FDC sarcoma is problematic due to the rarity of cases and the lack of specific clinical and imaging features. Therefore, we report a case of IPT-like FDCS with significant thrombocytopenia as clinical symptoms. The patient received platelet-raising therapy after surgical resection of the tumor. No tumor recurrence or metastasis was found during the 17-month follow-up, and the platelets returned to normal.
Case report
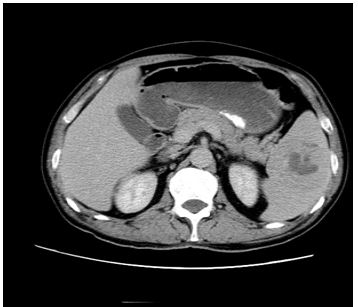
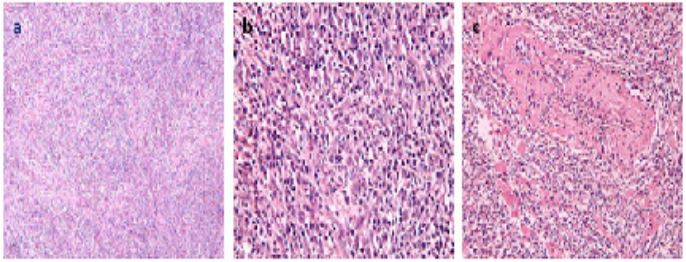
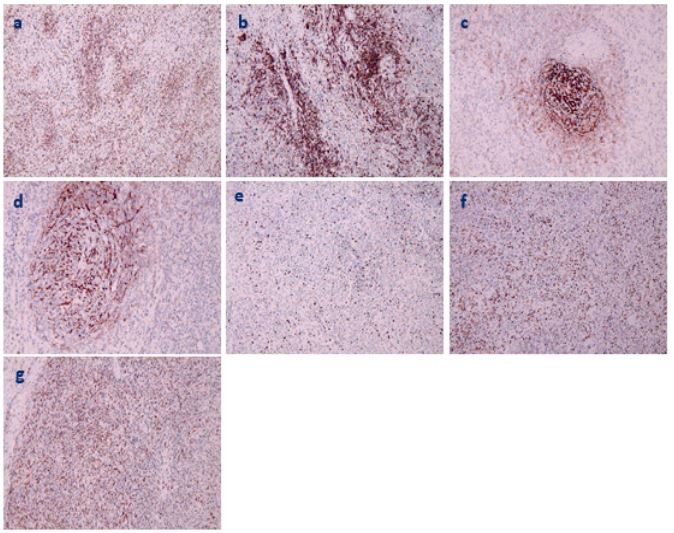
A 59-year-old male patient presented with bleeding gums and epistaxis in January 2020. Visited our hospital in September 2020. Blood routine showed: total white blood cells 9.4×109/L, monocytes 9.8%, hematocrit 0.279, hemoglobin 97g/L, red blood cells 3.05×1012, platelets 12×109/L, and platelet specific volume 0.01. Bone marrow smear showed: bone marrow hyperplasia was significantly active, megakaryocytic hyperplasia was significantly active with maturation disorders. Abdominal and pelvic ultrasound showed: spleen enlargement, solid mass in the spleen: lymphoma to be discharged; CT spleen with slightly low-density mass (6×6.3cm), increased FDG uptake, considering malignant tumor, abdominal enhanced CT: spleen mass, Consider malignancy (Figure 1). The patients were treated with splenectomy and histopathological examination of tumor specimens. Gross observation of pathological specimens: the mass is 9.5×5×3.5cm in size, with clear boundary with surrounding tissues, gray-white solid on the cut surface, medium texture, and focal necrosis. Morphological observation: tumor cells were arranged in loose bundles (Figure 2a), with swirling structures visible locally, with clear cell boundaries, spindle-shaped or oval, abundant cytoplasm, eosinophilic, nuclei mostly long spindle-shaped, and nuclear staining plasma vesicular, with small and clear nucleoli, mitoses are rare. There were many lymphocytes and plasma cells infiltrated between tumor cells (Figure 2b). Fibrin-like changes in the vessel wall (Figure 2c). Hemorrhage and sheet necrosis were seen locally in the tumor. Immunohistochemical results: CKpan-, CD20+, CD3+ (Figure 3a), CD10+(Figure 3b), CD21+ (Figure 3c), CD35+ (Figure 3d), Bcl-2-, Bcl-6-, Ki-67 (+30%) (Figure 3e), Mum-1+ (Figure 3f), CD138++, κ+, λ+, CD43++, IgD-, CD56 were scattered with a little +. Epstein-Barr virus in situ hybridization (EBER) showed a large number of Epstein-Barr virus-infected cells (Figure 3g). PCR: B line gene rearrangement detection: IGH monoclonal band detection (-); IGK monoclonal band detection (-). Pathological diagnosis of IPT-like FDC. Biological behavior is relatively lazy. Platelet-raising therapy was given after splenectomy. After 17 months of follow-up, no tumor recurrence or metastasis was found, and the platelets returned to normal.
Figure 1: CT imaging before surgery. spleen mass and intrahepatic nodule, considering spleen tumor with intrahepatic metastasis.
Figure 2: Routine pathological observation of tumor a. Tumor cells are arranged in bundles. b. Tumor cells are spindle-shaped or oval, with more lymphocytes and plasma cells infiltrated between cells. c. Vascular wall fibrin-like changes.
Figure 3: Immunohistochemical observation of tumor (magnification 100×, brown positive cells). a. CD3+. b. CD10+. c CD21+. d. CD35+. e. Ki-67 about 30%+. f. Mum-1+ .g. EBER+.
Discussion
The clinical manifestations are that the pathogenic mechanism of significant platelet reduction is very complex. Pathological changes in the spleen will lead to excessive platelet retention in the spleen, resulting in peripheral blood thrombocytopenia.
IPT-like FDCS is an extremely rare low-grade malignant tumor. Only 48 cases have been reported so far, with a male-to-female ratio of 1:1.5. Clinical manifestations include abdominal pain, bloating, abdominal mass, weight loss, fever, fatigue, anorexia, etc., but most cases have no obvious symptoms [7]. This case was reported for the first time with thrombocytopenia as the first symptom. The patient had no other symptoms except for bleeding gums and epistaxis.
The pathogenesis of IPT-like FDCS is related to EBV infection. It has also been documented that cases of IPT are associated with surgical or traumatic inflammation, autoimmune diseases, and infections such as Castleman disease and pallidococcus [8-11], although other pathogenic mechanisms remain unclear. This case was positive for EBV, accompanied by significant thrombocytopenia, suggesting that its pathogenesis was related to EBV infection and pathological changes in the spleen. Splenic tumor infiltration leads to splenic PLT retention, resulting in marked peripheral thrombocytopenia.
IPT-like FDCS consisted of neoplastic proliferative spindle cells with a large infiltrate of lymphoplasmacytic cells. The borders between cells are ill-defined and contain oval or elongated nuclei, vesicular or granular fine chromatin, and prominent nucleoli. Vascular fibrinoid changes are seen in this case, and EBV-induced cytokines and monokines are known to contribute to vascular proliferation, inflammation, and vascular injury [10], which may explain the vascular changes seen in our case.
Immunohistochemistry is crucial for the diagnosis of IPT-like FDCS. CD21 and CD35 are the preferred markers, positive support for the diagnosis of IPT-like FDCS. In this case, there are many plasma cells in the interstitium, CD138++, κ and λ light chains are all positive, CD43++, IgD-, and B-lineage gene rearrangement IGH and IGK monoclonal bands are all negative, so B-lineage lymphoma is excluded. About 30% of Ki-67 are positive, indicating that the tumor is low-grade malignant, and regular review and close attention are required.
In terms of treatment, surgical resection is usually the treatment of choice for patients with locally diseased tumors. The biological behavior of IPT-like FDCS is indolent, and patients can still survive for a long time after surgery. Survival for a long time even after relapse [12]. After splenectomy in this routine, platelet-raising therapy was given. After 17 months of follow-up, no tumor recurrence or metastasis was found, and the platelets returned to normal.
Conclusion
IPT-like FDCS is a clinically rare tumor. In this report, the cases of marked thrombocytopenia caused by the pathological changes of the spleen caused by the tumor are even rarer. The clinical and imaging manifestations of this tumor are non-specific, and the definitive diagnosis depends on histopathology and immunohistochemical staining. The biological behavior is indolent, and the prognosis is good after surgery and symptomatic treatment.
References
- Facchetti F, Simbeni M, Lorenzi L. Follicular dendritic cell sarcoma. Pathologica. 2021; 113: 316-329.
- Cheuk W, Chan JK, Shek TW, et al. Inflammatory pseudotumor-like follicular dendritic cell tumor: a distinctive low-grade malignant intra-abdominal neoplasm with consistent Epstein-Barr virus association. Am J Surg Pathol 2001; 25: 721-31.
- Morales-Vargas B, Deeb K, Peker D. Clinicopathologic and Molecular Analysis of Inflammatory Pseudotumor-Like Follicular/Fibroblastic Dendritic Cell Sarcoma: A Case Report and Review of Literature. Turk Patoloji Derg. 2021; 37: 266-272.
- Lifang Wang, Hui Deng, Mei Mao. Paraneoplastic pemphigus and myasthenia gravis, associated with inflammatory pseudotumor-like follicular dendritic cell sarcoma: response to rituximab. Clinical Case Reports 2016; 4(8): 797–799.
- Jia-Yi Zhuang, Fang-Fei Zhang, Qing-Wen Li, et al. Intra-abdominal inflammatory pseudotumor-like follicular dendritic cell sarcoma associated with paraneoplastic pemphigus: A case report and review of the literature. World J Clin Cases 2020 July 26; 8(14): 3097-3107.
- WANG Xiyan, LI Huiyuan, YANG Renchi. Immune Imbalance in Immune Thrombocytopenia. Chinese Journal of Cell Biology 2022; 44(1): 78-86.
- Bi-Xi Zhang, Zhi-Hong Chen, Yu Liu, et al. Inflammatory pseudotumor-like follicular dendritic cell sarcoma: A brief report of two cases. World J Gastrointest Oncol 2019 December 15; 11(12): 1231-1239.
- F Facchetti, P Incardona, S Lonardi, et al., Nodal inflammatory pseudotumor caused by leutic infection. American Journal of Surgical Pathology, 2009; 33( 3): 447–453.
- AC Tregnago, DL Morbeck, FD Costa, AH Campos, FA Soares and J Vassallo. Inflammatory pseudotumor-like follicular dendritic cell tumor: an underdiagnosed neoplasia. Applied Cancer Research, 2017; 37( 1): 45.
- Teruya-Feldstein J, Jaffe ES, Burd PR, et al. The role of Mig, the monokine induced by interferon-gamma, and IP-10, the interferongamma-inducible protein-10, in tissue necrosis and vascular damage associated with Epstein-Barr virus-positive lymphoproliferative disease. Blood 1997; 90: 4099-4105.
- Shuangshuang Deng, Jinli Gao. Inflammatory pseudotumor-like follicular dendritic sarcoma: a rare presentation of a hepatic mass. Int J Clin Exp Pathol 2019; 12(8): 3149-3155.
- Ge R, Liu C, Yin X, et al. Clinicopathologic characteristics of inflammatory pseudotumor-like follicular dendritic cell sarcoma. Int J Clin Exp Pathol 2014; 7: 2421-2429.