Case Report - Volume 2 - Issue 5
Combined Endoscopic and Open Surgical Management of Subacute Orbital Lesions associated with Granulomatosis with Polyangiitis: A Case Report
Jillian O Shaughnessy1, Jerlon Chiu2; Stacy Scofield-Kaplan3; Sonya Marcus2*
1Renaissance School of Medicine, Stony Brook University, Stony Brook, New York 11794, USA.
2Department of Surgery, Division of Otolaryngology-Head and Neck Surgery, Stony Brook Medicine, Stony Brook, New York 11794,USA.
3Department of Ophthalmology, Stony Brook Medicine, Stony Brook, New York 11794, USA
Received Date : July 21, 2022
Accepted Date : Aug 26, 2022
Published Date: Sep 09, 2022
Copyright:© Sonya Marcus 2022
*Corresponding Author : Sonya Marcus, HSC T19-068 Division of Otolaryngology-Head and Neck Surgery, Stony Brook Medicine, Stony Brook 11794-8191 Tel: 631-444-766
Email: sonya.marcus@stonybrookmedicine.edu
DOI: Doi.org/10.55920/2771-019X/1238
Abstract
Background: Granulomatosis with polyangiitis (GPA) can manifest with a range of rhinologic and ocular symptoms. Orbital involvement, occurring in 45% to 65% of patients, is typically responsive to immunosuppressive therapy. Surgery for subacute orbital lesions refractory to medical management has not been described in the literature. We present a case of an orbital lesion causing diplopia and gaze restrictions over time despite medical management, which underwent surgical decompression.
Methods: Case report
Results: A combined endoscopic and open decompression of the orbit was performed with partial excision of the mass, resulting in near complete resolution of the patient’s diplopia and gaze restriction.
Conclusions: Surgical decompression is a safe and effective option in the management of symptomatic subacute orbital masses associated with GPA that have been refractory to medical treatment.
Keywords: Orbital lesions; Granulomatosis with polyangiitis; Wegener’s granulomatosis; Endoscopic sinus surgery; Orbital manifestations.
Introduction
Granulomatosis with polyangiitis (GPA), commonly known as Wegener’s Granulomatosis, is an autoimmune granulomatous inflammatory disease of unclear etiology affecting small and medium sized blood vessels [1-4]. Presenting rhinologic symptoms commonly associated with GPA include rhinorrhea, ulcerations of the nasal mucosa, and chronic rhinosinusitis [1, 5]. Although the nasal cavity and paranasal sinuses are the most common zones of GPA involvement in the head and neck, 45% to 60% of patients experience involvement of the soft tissues of the orbit [1, 6]. Orbital manifestations of GPA can be either primary or due to extension of disease from the paranasal sinuses [2, 7]. Inflammation of orbital structures can cause ocular pain, injection, epiphora, vision loss, diplopia, and/or proptosis [7]. The mainstay of treatment includes glucocorticoids and immunosuppressive drugs such as cyclophosphamide, azathioprine, and methotrexate. In cases of severe pain, proptosis, or optic neuropathy, surgical decompression may be indicated [7].
Here, we present a case of a 37-year-old male with orbital manifestations of GPA refractory to medical treatment who underwent combined otolaryngologic and ophthalmologic surgery with improvement of his symptoms.
Case report
A 37-year-old male with a past medical history of well controlled GPA was referred to Otolaryngology clinic with 2 years of progressive diplopia requiring chronic head-turn, left sided medial gaze restriction, and worsening proptosis. He denied any orbital pain, decline in visual acuity, or sinonasal complaints. He had no improvement in double vision following a 2-week course of oral steroids (1mg/kg). On examination, he had 2mm of left-sided proptosis and 75% restriction of left sided medial gaze, but no evidence of optic neuropathy. Rigid nasal endoscopy was notable for a common cavity with minimal sinonasal landmarks present; otherwise, the nasal mucosa was healthy and no purulence was noted.
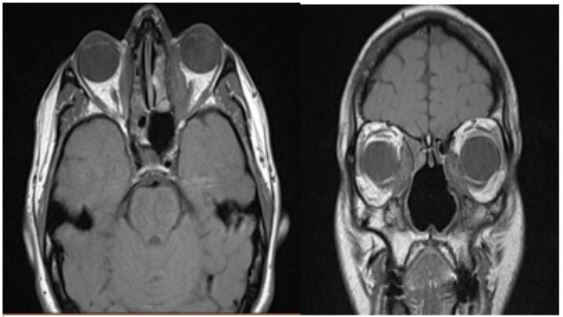
His past medical history included GPA diagnosed at age 25, of which chronic rhinosinusitis, pulmonary nodules, and tracheal stenosis were his predominant manifestations. He was treated with glucocorticoids and immunosuppressive agents with good response and was in remission for 5 years prior to presentation to Otolaryngology. He had been noted to have bilateral medial orbital masses, left larger than right, which were stable on serial imaging for many years. A MRI of orbits without contrast showed a stable left medial extraconal mass measuring 2.8 x 1.0 x 3.7 cm and a right medial extraconal mass measuring 2.4 x 0.9 x 2.6 cm (Figure 1). A left anterior orbitotomy with biopsy was previously performed, which revealed benign dense fibrous tissue with a small foci of chronic inflammation, negative for malignancy.
Given there was no improvement with high dose oral steroids, surgical management was discussed and recommended. Through a combined approach with Otolaryngology and Ophthalmology, the patient underwent an image-guided left sphenoidotomy, left endoscopic orbital decompression, and left anterior orbitotomy with excision of the mass without complication. The left lamina papyracea and bone overlying the orbital apex were drilled and removed, and portions of the orbital mass were resected both endoscopically and through the orbit. Alloderm was placed to create a barrier between the medial rectus muscle and the sinuses. Final surgical pathology showed dense paucicellular fibrous tissue and fibrovascular/granulation tissue with severe acute and chronic inflammation. One year following surgical repair, the patient continues to report marked improvement in his diplopia. His exam was notable for a 1-2mm improvement in proptosis and only mild (<25%) limitation in movement of the left eye medially.
Figure 1: MRI of orbits without contrast, T1-weighted sequences, axial (left) and coronal (right) cuts demonstrating bilateral medial orbit masses.
Discussion
Medical management of the underlying disease is typically sufficient for managing orbital manifestations of GPA [7-9]. Treatment typically includes a glucocorticoid with or without an immunosuppressive medication such as rituximab, azathioprine, methotrexate, or cyclophosphamide [10]. Of note, ocular manifestations are usually refractory to glucocorticoid treatment alone [7]. In cases of acute vision loss refractory to medical treatment, urgent surgical decompression as a sight-saving, emergency procedure has been described, albeit with mixed success [11-14]. Other treatment options to consider are intraocular glucocorticoid injections or slow-release implantation devices, though they have the potential to cause cataracts and open-angle glaucoma [7].
In contrast, the role of surgical decompression in subacute ocular disease due to GPA is poorly described in the literature, and as such the indication for surgical decompression is less clear. Patients with orbital manifestations of GPA may develop diplopia over the course of the disease, either due to inflammation of the vessels supplying the extraocular muscles or due to mass effect [7]. Herein, we present a patient with well controlled GPA with subacute ocular symptoms refractory to medical management who had a significant improvement in double vision and proptosis through a combined endoscopic and open orbital decompression.
Conclusion
Combined ENT-ophthalmologic surgery is a safe and effective option for patients with subacute orbital manifestations of GPA refractory to medical treatment.
Institutional Review Board Approval: Exempt.
Funding and Conflicts of Interest: None.
References
- Greco A, et al. Clinic manifestations in granulomatosis with polyangiitis. Int J Immunopathol Pharmacol, 2016; 29(2): 151-9.
- Vischio JA and CT McCrary. Orbital Wegener's granulomatosis: a case report and review of the literature. Clin Rheumatol, 2008; 27(10): 1333-6.
- Wolff SM, et al. Wegener's granulomatosis. Ann Intern Med, 1974; 81(4): 513-25.
- Ntatsaki E, RA Watts, and DG Scott. Epidemiology of ANCA-associated vasculitis. Rheum Dis Clin North Am, 2010; 36(3): 447-61.
- Gubbels SP, A Barkhuizen, and PH Hwang. Head and neck manifestations of Wegener's granulomatosis. Otolaryngologic Clinics of North America, 2003; 36(4): 685-705.
- Muller K and JH Lin. Orbital Granulomatosis With Polyangiitis (Wegener Granulomatosis): Clinical and Pathologic Findings. Archives of Pathology & Laboratory Medicine, 2014; 138(8): 1110-1114.
- Pakrou N, D Selva, and I Leibovitch. Wegener’s Granulomatosis: Ophthalmic Manifestations and Management. Seminars in Arthritis and Rheumatism, 2006; 35(5): 284-292.
- Babu K and B Dharmanand. Worsening of posterior scleritis and orbital pseudotumor in a patient with granulomatosis polyangiitis with rituximab-A case report. Indian journal of ophthalmology, 2020; 68(9): 1986-1988.
- Isse N, et al. Granulomatosis with polyangiitis presenting as an orbital inflammatory pseudotumor: a case report. Journal of medical case reports, 2013; 7(1): 110-110.
- Andrada-Elena M, et al. Wegener's granulomatosis with orbital involvement: case report and literature review. Rom J Ophthalmol, 2021; 65(1): 93-97.
- Fishman JM, A Slovick, and CA East. Wegener's granulomatosis of the orbit: two cases requiring endoscopic surgical decompression. The Journal of Laryngology & Otology, 2008; 122(11): 1257-1259.
- Murai Y, et al. Granulomatosis with Polyangiitis Presenting with Bilateral Orbital Apex Syndrome. Case Reports in Ophthalmology, 2021; 12(1): 32-40.
- Santiago YM and A Fay. Wegener's Granulomatosis of the Orbit: A Review of Clinical Features and Updates in Diagnosis and Treatment. Seminars in ophthalmology, 2011; 26(4-5): 349-355.
- Thorne JE and DA Jabs. OCULAR MANIFESTATIONS OF VASCULITIS. Rheumatic Disease Clinics of North America, 2001; 27(4): 761-779.