Case Report - Volume 2 - Issue 5
A Case of Tracheobronchitis in a Patient with Ulcerative Colitis
Jerlon Chiu1; Roy Wang Qu2; Katharine A Kevill3; Melissa M Mortensen-Welch4*
1Department of Surgery, Division of Otolaryngology-Head and Neck Surgery, Stony Brook Medicine, Stony Brook, New York 11794,USA.
2Department of Otolaryngology, Loma Linda University of Health, Loma Linda, CA 92354, USA.
3Department of Pediatrics, Stony Brook Medicine, Stony Brook, New York 11794, USA.
4Department of Otolaryngology-Head and Neck Surgery, Albany Medical Center, Albany 12208, USA
Received Date : July 21, 2022
Accepted Date : Aug 26, 2022
Published Date: Sep 10, 2022
Copyright:© Melissa M Mortensen 2022
*Corresponding Author : Melissa M Mortensen, 50 New Scotland Avenue, Albany, NY 12208, Department of Otolaryngology-Head and Neck Surgery, Albany Medical Center, Albany 12208, USA.Tel:518-262-5575
Email:mortenm1@amc.edu
DOI: Doi.org/10.55920/2771-019X/1239
Abstract
Background: Common extra-intestinal manifestations of ulcerative colitis (UC) have been previously described such as uveitis, conjunctivitis, seronegative arthritis, and erythema nodosum. Less well known extra-intestinal manifestations are described in the pulmonary organs. We present a case of a chronic cough thought to be habitual in nature that was ultimately diagnosed as a tracheobronchitis related to ulcerative colitis.
Methods: Case report.
Results: Clinic stroboscopy lead to examination under anesthesia with suspension laryngoscopy, biopsy and culture and concurrent bronchoscopy with biopsy and washings which lead to a diagnosis of tracheobronchitis related to ulcerative colitis.
Conclusions: Upper airway and pulmonary manifestations can be seen in UC, even when the colon is not actively inflamed. Thorough examination with laryngoscopy and bronchoscopy should be performed in patients refractory to treatment.
Keywords: Tracheobronchitis; Ulcerative colitis; Inflammatory bowel disease.
Introduction
Many extra-intestinal manifestations of inflammatory bowel disease (IBD) have been well described, including uveitis, conjunctivitis, seronegative arthritis, and erythema nodosum. Clinically overt IBD-related pulmonary disease is rare, despite estimates of subclinical pulmonary disease as high as 40-60% [1]. Reported pulmonary manifestations of IBD, especially ulcerative colitis (UC), include bronchiectasis, bronchitis, tracheobronchitis, bronchiolitis, and interstitial lung disease [1]. In UC, large airway involvement is unrelated to bowel disease activity and may present with or without gastrointestinal symptoms. Here, we present a patient with UC and multiple confounding comorbidities, referred to otolaryngology for chronic cough, dysphonia, and dyspnea, and ultimately diagnosed with tracheobronchitis secondary to his UC.
Case report
A 20-year-old male with a past medical history of gastroesophageal reflux, asthma, seasonal allergies, and well-controlled UC was referred to Otolaryngology clinic with chronic cough, hoarseness, and dyspnea. He had a persistent intermittent cough for three years with interval periods of resolution. The cough was intermittently productive for green sputum and worse during the night. He had several episodes of cough with associated dyspnea prompting visits to the emergency department. Prior to his presentation to Otolaryngology, the cough had been resolved for more than a year, but then began to worsen to the point that he could not talk, laugh, or exercise without coughing. He also began to have difficulty projecting his voice and occasional aphonia, and along with the worsening cough prompted a referral from his Pulmonologist to Otolaryngology for evaluation of vocal fold function, as there was a concern for paradoxical vocal fold dysfunction. His Pulmonologist had diagnosed him with habitual cough several years earlier with flexible bronchoscopy. The patient had also received several courses of low dose oral steroids, inhaled corticosteroids, albuterol, and antibiotics such as azithromycin and levofloxacin from the emergency department and pulmonologist for exacerbation of his cough. He experienced minimal relief of his symptoms with these therapies. His past medical history included UC diagnosed at age 16, overall well-controlled with oral mesalamine and mesalamine enemas without surgical intervention. He had gastroesophageal reflux treated with omeprazole and seasonal allergic rhinitis treated with cetirizine, nasal fluticasone, and nasal saline sprays. Patient is a lifetime nonsmoker. Prior workup for his chronic cough included normal pulmonary function tests, sputum culture growing normal respiratory flora, and several chest X-rays without persistent radiologic findings diagnostic for a specific etiology. A CT chest without contrast showed patchy ground-glass opacities in the left lower lobe with no consolidations, consistent with an atypical infectious or inflammatory process.
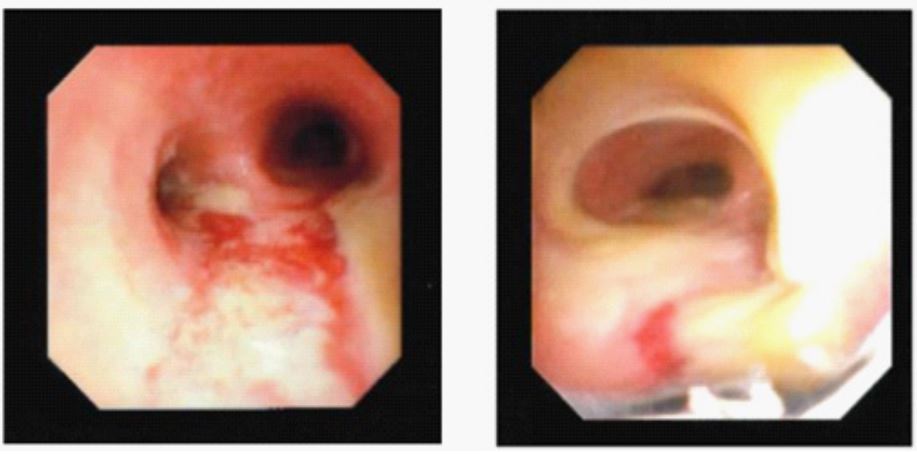
Upon presentation to Otolaryngology clinic, bedside stroboscopy showed generalized laryngeal erythema and thick yellow mucus in the subglottis and trachea (Figure 1). He was diagnosed with tracheitis and laryngitis and tried on a course of levofloxacin. After he failed to improve, he underwent microsuspension direct laryngoscopy with laryngeal biopsy and culture. Concurrent flexible bronchoscopy with bronchoalveolar lavage (BAL) was notable for erythema and white-yellow plaques on the tracheal wall, carina, and bilateral bronchi (Figure 2). Histology of the trachea showed respiratory and squamous mucosa reactive changes and marked chronic inflammation in the lamina propria. This suggested that the tracheobronchitis was an extraintestinal manifestation of ulcerative colitis. The BAL grew Streptococcus mitis, Staphylococcus aureus, Stomatococcus, Gemella sanguinis, and Haemophilus influenzae. He was treated inpatient with high-dose pulse IV steroids (1,000 mg methylprednisolone daily) for three days and ceftriaxone, with immediate, marked improvement of his cough. He was discharged home with a two-week course of Augmentin and one-month oral prednisone taper.
Repeat flexible bronchoscopy one month after his first procedure showed resolution of erythema and plaques. Patient developed recurrent cough two months after the prednisone taper, which was improved by a one-week course of prednisone 60 mg daily. Notably, he was able to tolerate a strenuous two-week hiking trip. Repeat stroboscopy at a four-month follow-up with Otolaryngology showed some minimal white mucus in the subglottis with no laryngeal erythema.
Figure 1: Laryngeal stroboscopy with generalized erythema and mucus in the subglottis.
Figure 2: Initial bronchoscopy with plaques at the carina (left) and trachea (right).
Discussion
Tracheobronchitis as an extraintestinal manifestation of UC is rare and may be difficult to diagnose. Patients typically present with non-specific airway symptoms such as chronic cough, dyspnea, and wheezing, and can be misdiagnosed with asthma. Furthermore, the presence of superimposed infections may further obscure the diagnosis and delay treatment. A thorough investigation for pulmonary pathology, particularly large airway involvement, is crucial to diagnosis. Other diseases to consider include infection, systemic vasculitis, relapsing polychondritis, amyloidosis, and malignancy. Large airway involvement may present at any time before or after the initial diagnosis and even after distant colectomy [3]. This phenomenon supports the hypothesis of Kinnear and Higenbottam that the gastrointestinal inflammation may shift to the airways, indicating an intact colon is not a prerequisite for pulmonary disease [2]. If allowed to progress, the natural history of tracheobronchitis leads to airway stenosis and respiratory failure [4]. In this case, early evaluation with in-office flexible laryngoscopy for visualization of the upper airway was key. Subsequent laryngoscopy, bronchoscopy, and biopsy led to a rapid diagnosis and administration of high dose steroids that altered the disease course for this patient. Mainstay therapy to UC related tracheobronchitis includes inhaled and oral high-dose steroids, though use of other immunosuppressants and immunomodulators such as azathioprine and infliximab have been reported for refractory cases [2,4].
Conclusion
Tracheobronchitis is a rare pulmonary manifestation of UC that may be difficult to diagnose, especially in the setting of multiple comorbidities such as allergies, gastroesophageal reflux, and asthma. Bedside flexible laryngoscopy by an Otolaryngologist should be considered in patients with IBD that present with airway symptoms refractory to treatment.
Institutional Review Board Approval: Exempt.
Meeting information: 2020 Combined Otolaryngology Spring Meetings Virtual Poster Session, Triological Society, 5/15/2020 – 6/15/2020
Funding and Conflicts of Interest: None.
References
- Majewski S, Piotrowski W. Pulmonary manifestations of inflammatory bowel disease. Arch Med Sci 2015; 11: 1179-1188.
- Kar S, Thomas SG. A case of tracheobronchitis in ulcerative colitis: a review of literature. Clin Respir J 2009; 3: 51-54.
- Vasishta S, Wood JB, McGinty F. Ulcerative tracheobronchitis years after colectomy for ulcerative colitis. Chest 1994; 106: 1279-1281.
- Kuzniar T, Sleiman C, Brugiere Oet al. Severe tracheobronchial stenosis in a patient with Crohn's disease. Eur Respir J 2000; 15: 209-212.