Case Report - Volume 2 - Issue 5
The Integrated Management of Cervical hyperostosis in Patients with Dyspnea and Dysphagia to Reduce Risk of Airway Compromise: A Case Series
J Preece1; James Metkus2; V Shah3*; M Mortensen1
1Department of Otolaryngology and Head and Neck Surgery, Albany Medical Center, Albany NY, USA.
2Division of Otolaryngology-Head and Neck Surgery, Department of Surgery, Stony Brook Medicine, Stony Brook NY, USA.
3Albany Medical College, Albany NY USA
Received Date : July 21, 2022
Accepted Date : Aug 29, 2022
Published Date: Sep 12, 2022
Copyright:© V Shah 2022
*Corresponding Author : V Shah, Albany Medical College, Albany NY,704-770-6896, 344 Quail Street, Albany, New York 12208 USA.
Email:shahv1@amc.edu
DOI: Doi.org/10.55920/2771-019X/1240
Abstract
Objectives: Diffuse idiopathic skeletal hyperostosis (DISH) is a non-inflammatory condition diagnosed by the presence of flowing vertebral ossifications along the anterior longitudinal ligament. Limited literature on cervical spine DISH, or cervical hyperostosis (CH), demonstrates that this sub-type of DISH may present with severe oropharyngeal symptoms. Two common manifestations of CH are dysphagia and dyspnea. The purpose of this case series was to provide more insight into detection and management of CH to potentially reduce the risk of impending airway compromise.
Methods: Three patients with CH were selected from two institutions. Each patient presented with similar symptoms of dysphagia and dyspnea. The presentation, diagnosis, and management plan for each patient is described.
Results: Patients ranged from 53 to 76 years of age. All patients presented with dyspnea and dysphagia at the initial appointment, and all patients had co-existing GERD. Patient 1 and Patient 3 patients had vocal cord paralysis and pharyngeal wall fullness due to CH. Patient 2 had vocal cord paralysis and posterior glottic edema due to CH. Patient 1 and Patient 2 underwent anterior resection of their cervical osteophytes and tracheostomy. Dysphagia in both patients resolved after surgery, but their dyspnea persisted. Patient 1 required a transverse cordectomy for bilateral vocal cord paralysis, which treated his dyspnea. Patient 2 had normal vocal fold mobility post-operatively. Patient 3 had a similar pathophysiology and presentation to Patient 1, but she was lost to follow-up.
Conclusion: Existing literature demonstrates that several factors contribute to dyspnea in CH, including vocal fold paralysis and glottic edema. This series demonstrated that not only was surgery successful for partial resolution of symptoms, but also treatment with cordectomy, speech/swallow therapy, and acid-reducers was also beneficial.
Keywords: Skeletal hyperostosis; tracheostomy; dyspnea; dysphagia; cervical osteophytes.
Introduction
Diffuse idiopathic skeletal hyperostosis (DISH) is a non-inflammatory condition characterized by osteophytic growth along the anterior longitudinal ligament. The disease process was first described after Forestier discovered radiographic changes in elderly males with spinal stiffness [1]. The prevalence of DISH increases with age, affecting 25-27% of men over 50-years-old and 12-15% of women over 50-years-old [2-4]. DISH is diagnosed by the presence of flowing vertebral ossifications at four contiguous vertebrae, preserved intervertebral disc height, absent ankylosis at the facet-joints, and absent sacroiliac joint changes [5]. DISH is considered mainly asymptomatic and is debated on whether it manifests with clinical symptoms [6]. Cervical spine DISH, or cervical hyperostosis (CH), is a less common manifestation of DISH and is associated with more severe symptoms, including dysphagia and dyspnea [5-6]. Dysphagia and respiratory compromise are the most common complaints that lead patients to seek surgical treatment. The objective of this case series was to present three patients complaining of dyspnea due to CH at two institutions and their subsequent treatment. Additionally, a comprehensive review of the literature for patients with airway obstruction and CH was performed.
Case Series Presentation
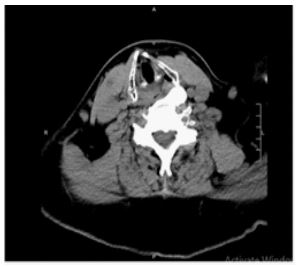
The following are summaries of three patients with CH and their subsequent treatment. (Table 1) shows a summary of patient findings
Table 1: Patient Findings.
Case 1
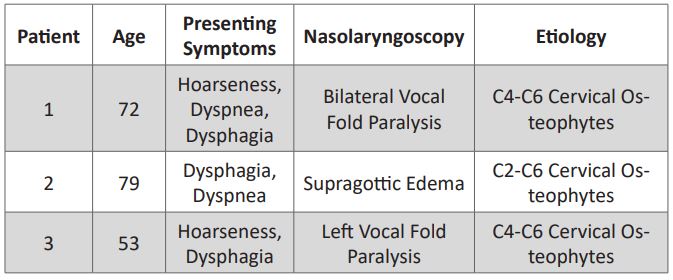
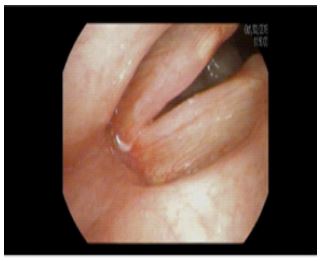
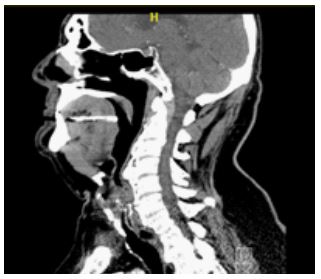
71-year-old male presented to clinic for evaluation of dysphagia, dyspnea, and hoarseness. Two years prior to presentation, the patient was treated for respiratory distress with intubation and was subsequently decannulated. Past medical history included long-term SOB and GERD treated with a PPI. On exam, stroboscopy revealed bilateral vocal fold paralysis and posterior pharyngeal wall fullness concerning for CH (Figure 1). CT imaging showed severe osteophytes at C4-C5 and C5-C6 (Figures 2 and 3). Neurosurgery and otolaryngology collaborated to resect cervical osteophytes via an anterior neck approach. Postoperatively, the patient was admitted and given a thick diet. On postoperative day two, he was discharged without complications. Vocal fold paralysis and dyspnea were persistent after surgery, and the patient was surgically treated with left vocal fold transverse cordectomy and left medial arytenoidectomy. He received speech/swallow therapy and was eventually cleared for a regular diet. Although he continued to have vocal fold immobility, his dyspnea resolved after the cordectomy.
Figure 1: Patient 1 Stroboscopy on full abduction demonstrating vocal fold paralysis.
Figure 2: Patient 1 Sagittal view of CT Neck preoperative view demonstrating cervical osteophytes.
Figure 3: Patient 1 Axial view of CT Neck preoperative view demonstrating cervical osteophytes.
Case 2
76-year-old male presented to clinic for evaluation of worsening dysphagia and dyspnea. Past medical history included spine surgery for severe cord compression, tracheostomy for dyspnea with failed decannulation due to laryngeal edema, and GERD treated with a PPI. Nasolaryngoscopy showed bilateral vocal fold paresis and posterior glottic edema. On diagnostic laryngoscopy, he had a biopsy which was negative for carcinoma and was diagnosed with posterior glottic stenosis. Edema and a large bony protuberance overlying the cricopharyngeal muscle were also noted intraoperatively. CT imaging showed severe osteophytes at C4-C5 and C5-C6 compressing the larynx and upper esophageal sphincter. He underwent excision of tracheal granulation tissue and tracheostomy decannulation by otolaryngology. Later, he was treated by neurosurgery with anterior resection of cervical osteophytes. On postoperative day one, he was discharged without issue. The patient was seen by speech/swallow therapy and cleared for regular diet. Postoperatively, he had continued dysphagia but no longer reported dyspnea. Nasolaryngoscopy showed resolution of the protuberance with normal vocal fold mobility bilaterally.
Case 3
53-year-old woman presented to clinic for evaluation of hoarseness and dyspnea six months after treatment in the ICU for a drug overdose. While in the ICU, the patient was intubated three separate times. She was hoarse immediately after intubation and slowly improved but was still not near her normal voice. Relevant history included a current ½ pack per day smoking history, cervical neuropathy, TBI, post-polio syndrome, and HIV for which she took several medications. Nasolaryngoscopy showed left vocal cord paralysis with moderate reflux change, and stroboscopy showed vocal cord edema with left posterior pharynx fullness. The patient was prescribed a PPI and advised to quit smoking. Three months later, her swallow study showed mild dysphagia without aspiration, but the patient refused speech therapy and continued to smoke. CT imaging showed prominent anterior osteophytosis at C4-C6 levels causing mass effect on the left hypopharynx. Since being informed of these findings, the patient has not returned to the office.
Discussion
CH can cause various clinical manifestations involving the pharynx, larynx, and esophagus. In our series, two of our patients had complaints of dyspnea from CH requiring tracheostomy and surgery. Our third patient had symptoms consistent with CH but was not amenable to conservative treatment and has been lost to follow-up. Previous studies have shown CH leading to respiratory compromise and requiring intubation or tracheostomy [7-8]. In fact, existing literature points that dysphagia and respiratory compromise were the most common complaints, affecting 93% and 31% of patients with CH, respectively [9]. Reported explanations for dyspnea due to CH include compression, glottic edema, and vocal fold immobility [7-8]. In our series, dyspnea likely resulted from vocal fold immobility due to CH in Patients 1 and 3 and from vocal fold immobility and edema in Patient 2.
While CH treatment involves conservative strategies to reduce aspiration and GERD with reflux control and speech/swallow therapy, surgery has also been proven successful [8]. Current literature demonstrates that most patients with CH are treated operatively with an anterolateral approach, achieving a high success rate [10]. While two patients were treated with anterior resection of the cervical osteophytes in this series, they did not have immediate resolution of their symptoms. For Patient 1, the vocal fold paralysis, and thus dyspnea, persisted after resection and only resolved after cordectomy. For Patient 2, resection resulted in treatment of the edema and vocal fold paralysis, although the patient continued to have dysphagia. In contrast to the existing literature, in which most studies found resolution of dysphagia post-operatively, our study observed resolution of dyspnea by treating the underlying cause. Overall, in patients with cervical DISH and dysphagia, early treatment may prevent disease progression to airway compromise.
Conclusion
While DISH is traditionally believed to be asymptomatic, CH should be considered for complaints of dyspnea among older patients that present with dysphagia. Early treatment of CH in elderly patients with dysphagia should be considered to potentially prevent airway compromise.
Acknowledgements
Dr. Jaclyn Carey: planning of manuscript, data gathering and review, manuscript preparation, critical review of manuscript.
Dr. James Metkus: concept, planning of manuscript, data gathering and review, manuscript preparation, critical review of manuscript.
Virali Shah: manuscript preparation and critical review of manuscript.
Dr. Melissa Mortensen: concept, manuscript preparation and critical review of manuscript.
Conflicts of Interest and Source of Funding: There is no conflict of interest or source of funding to disclose from any of the authors.
References
- Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950; 9(4): 321-330.
- Weinfeld RM, Olson PN, Maki DD, Griffiths HJ. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997; 26(4): 222-225.
- Kiss C, O'Neill TW, Mituszova M, Szilagyi M, Poor G. The prevalence of diffuse idiopathic skeletal hyperostosis in a population-based study in Hungary. Scand J Rheumatol. 2002; 31(4): 226-229.
- Westerveld LA, van Ufford HM, Verlaan JJ, Oner FC. The prevalence of diffuse idiopathic skeletal hyperostosis in an outpatient population in The Netherlands. J Rheumatol. 2008; 35(8): 1635-1638.
- Kuperus JS, Mohamed Hoesein FAA, de Jong PA, Verlaan JJ. Diffuse idiopathic skeletal hyperostosis: Etiology and clinical relevance. Best Pract Res Clin Rheumatol. 2020; 34(3): 101527.
- Cassim B, Mody GM, Rubin DL. The prevalence of diffuse idiopathic skeletal hyperostosis in African blacks. Br J Rheumatol. 1990; 29(2): 131-132.
- Verlaan JJ, Boswijk PF, de Ru JA, Dhert WJ, Oner FC. Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction. Spine J. 2011; 11(11): 1058-1067.
- Sebaaly A, Boubez G, Sunna T, et al. Diffuse Idiopathic Hyperostosis Manifesting as Dysphagia and Bilateral Cord Paralysis: A Case Report and Literature Review. World Neurosurg. 2018; 111: 79-85.
- Zarei M, Golbakhsh M, Rostami M, Moosavi M. Dysphonia, Stridor, and Dysphagia Caused By Diffuse Idiopathic Skeletal Hyperostosis: Case Report and Review of Literature. Adv Biomed Res. 2020 Sep 30; 9: 47.
- Souza S, Raggio B, Bareiss A, Friedlander P. Diffuse Idiopathic Skeletal Hyperostosis of the Cervical Spine: A Risk for Acute Airway Obstruction. Ear Nose Throat J. 2020 May 29: 145561320931212.