Case Report - Volume 2 - Issue 5
Focal Infarction of the Falciform Ligament: Case Series
Daniella Boros; Abdul Khan; Hina Arif*
Department of Medical Imaging, University of Arizona, Tucson, AZ, USA.
Received Date : July 28, 2022
Accepted Date : Aug 31, 2022
Published Date: Sep 14, 2022
Copyright:© Hina Arif 2022
*Corresponding Author : Hina Arif, Division Chief, Abdominal Radiology,University of Arizona. 1501 N. Campbell Ave, Room 1343, Tucson, AZ85724-5058, USA.Tel: (520) 626-1957
Email:hinarif@radiology.arizona.edu
DOI: Doi.org/10.55920/2771-019X/1242
Abstract
Background: The purpose of this article is to review the clinical presentation and imaging findings of a case of focal infarction of the falciform ligament.
Methods: Patient’s history and diagnostic imaging were retrospectively reviewed. These findings were compared with cases of falciform ligament torsion and/or infraction reported in the literature.
Results: To our knowledge, there are less than twenty cases of falciform ligament torsion and/or infraction reported in the literature [2,4]. Our patient’s presentation of right upper quadrant/epigastric pain was consistent with reported symptoms. While imaging findings using ultrasound have been reported, our case did not reveal any abnormalities on ultrasound. CT findings in our case were similar to findings in the literature and revealed significant fat stranding and inflammatory changes along the falciform ligament. Our diagnosis was also supported using MRI which revealed hyperintensitysurrounding the falciform ligament on T1 and T2/SPAIR as well as rim enhancement on T1 weighted post gadolinium imaging. MRI findings have only been described in one other case in the literature [3].
Conclusion: Imaging findings of falciform ligament torsion and/or infarction have been described in the literature using ultrasound, CT and MRI [3]. In our case, the diagnosis of focal infarction of the falciform ligament was supported by CT and MRI. It is important for radiologists to be aware of this diagnosis as there are few reported cases in the literature and the clinical presentation is often non-specific.
Keywords: Falciform Ligament Infarction
Background
The falciform ligament is a peritoneal fold that contains the ligamentum teres, obliterated umbilical vein, and extraperitoneal fat [1]. Pathology of the falciform ligament is rare but can include focal infarction and necrosis. Torsion of the fatty appendages of the falciform ligament results in ischemia [1,2]. Clinically, focal infarction of the falciform ligament can present with acute abdominal pain which may mimic other hepatobiliary, gastroduodenal, and pancreatic diseases [3]. The diagnosis can be identified on imaging. In this case report of falciform ligament focal infraction, we describe the clinical presentation, CT and MRI findings, and management.
Clinical Case
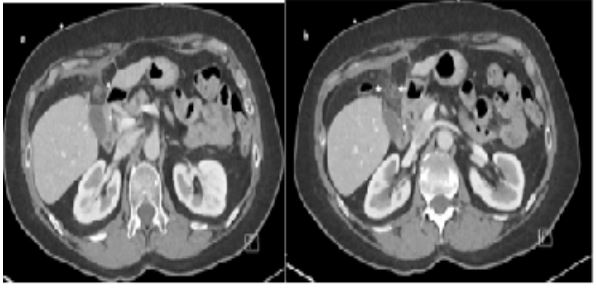
A 65-year-old female with past medical history of multiple sclerosis, hepatic adenoma, and gastritis presented to the Emergency Department with three days of right upper quadrant and epigastric pain. The patient described the pain as burning, with waxing and waning severity, worse with ambulation. The patient denied nausea, vomiting, or associated symptoms with eating or drinking. On presentation, the patient was hemodynamically stable. Physical examination revealed right upper quadrant tenderness to palpation without rebound or guarding. Laboratory evaluation revealed normal white count, electrolytes, and liver function. Ultrasound and a contrast enhanced CT abdomen and pelvis showed a left hepatic lobe adenoma consistent with the patient’s history. The CT also revealed significant fat stranding and inflammatory changes along the falciform ligament involving the adjacent portion of the paraumbilical vein. These findings were suggestive of acute infarction of the falciform ligament likely contributing to patient’s presentation with right upper quadrant pain [Figure 1]. The remainder of the exam including evaluation of the solid organs and other etiology of right upper quadrant pain was normal. The patient was discharged with recommendation for conservative management with nonsteroidal anti inflammatory medication and MRI follow up for the hepatic adenoma
Figure 1a-b: (a) Axial contrast computed tomography shows “swirling” of the umbilical vein (arrow). (b) Fat stranding along the falciform ligament. Note the appearance of normal appearing gallbladder (arrowhead).
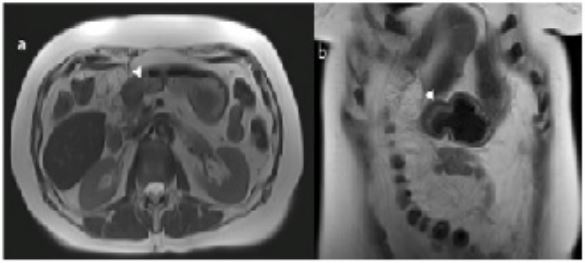
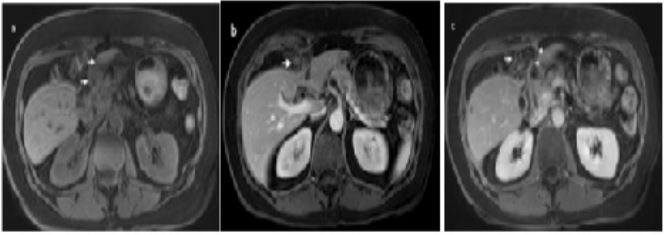
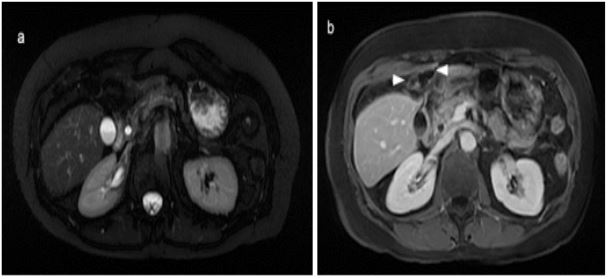
MRI surveillance was performed ten days later with on a contrast enhancement MR abdomen on a 1.5 T magnet (Magnetom Aera). The scan revealed inflammatory changes with necrosis along the falciform ligament in the form of hyperintensity surrounding the falciform ligament on single shot T2 weighted images (ssT2WI) with and without fat saturation. Pre and post contrast fat saturated gradient recoiled echo (GRE) T1 weighted images (WI) in venous phase showed decreased edema, progressive involution, and early encapsulation with surrounding rim enhancement [Figure 2-4]. The hepatic adenoma also appeared unchanged on MR imaging. On follow up visit with provider, approximately two weeks after the initial onset of symptoms, the patient reported improvement of abdominal pain following conservative management. An additional MRI scan was performed five months later which showed continued involution of necrosis along the falciform ligament with resolution of inflammatory changes [Figure 5].
Figure 2 a-b: Axial (a) and Coronal (b) ssT2WI images demonstrate encapsulation (arrows) of the fat necrosis about the falciform ligament.
Figure 3: Axial fat saturated ssT2WI image shows inflammation of the falciform ligament with surrounding encapsulation (arrows).
Figure 4a-c: (a) Axial fat saturated gradient echo T1 weighted image pre gadolinium administration shows increased signal about the falciform ligament fat (arrow) indicative of inflammation and edema. (b) Axial fat saturated gradient echo T1 weighted image post gadolinium administration shows heterogenous fat with enhancement (arrow) suggestive of inflammation. (c) Axial fat saturated gradient echo T1 weighted image post gadolinium administration shows fat necrosis (arrow) with surrounding rim enhancement (arrowheads) in keeping with involution and early encapsulation.
Figure 5a-b: (a) Axial fat saturated ssT2WI image shows resolution of the falciform ligament. (b) Axial fat saturated gradient echo T1 weighted image post gadolinium administration shows continued involution and encapsulation (arrowhead).
Angiography was performed using a right transfemoral arterial approach with study of the abdominal aorta, selective catheterization of the left renal artery, and super selective intraparenchymal branches of the middle and upper renal pole using a microcatheter under anesthesia care. The examination revealed the presence of two spreads of constraint of the renal parenchyma compatible with pseudoaneurysms in correspondence of the superior and mesorenal renal pole, both less than 2 centimeters (Figure 4). Finally, embolization of the arterial branches afferent to the lesions was performed by positioning metal coils with controlled release (3 at the upper pole: 2 x 70 mm and 1 x 70 mm; 2 at the mesorenal level of 3 x 70 mm) (Figure 5,6). In the days following the embolization there was a rise in hemoglobin, the complete disappearance of hematuria and a normalization of the indexes of phlogosis
Discussion
The falciform ligament is a double layer peritoneum derived from ventral mesentery that connects the anterior portion of the liver to the inferior diaphragm and ventral abdominal wall [2]. It contains the ligamentum teres, obliterated umbilical veins, and variable amount of extraperitoneal fat which can form fatty appendages [1,4]. The falciform ligament is supplied arterially by the left inferior phrenic and middle hepatic arteries. Venous drainage is via the left inferior phrenic vein [4,5]. Pathology of the falciform ligament is uncommon, but can include internal herniation, cystic lesions, secondary infections [1,2], and recanalization secondary to portal hypertension [6].
In rare cases, focal infraction and necrosis of the falciform ligament can occur, similar to the index case. This can be associated with torsion of the falciform ligament fatty appendages, which was first described by Beasley in 1959. The diagnosis was made histologically following laparotomy for a suspected perforated peptic ulcer [7]. In 2001, Coulier et al. described a similar case and the first CT and ultrasound findings associated with falciform ligament fatty appendage torsion and necrosis [1]. The falciform ligament is considered a rare location for intraperitoneal focal fat infarction which is more commonly described in epiploic appendages and omentum [1,2,8].
To our knowledge, there are less than twenty cases of falciform ligament torsion and/or focal infraction reported in the literature [2,4]. As in our case, inflammation/infarction of falciform ligament fat often presents with epigastric and/or right upper quadrant pain, with or without constitutional symptoms. The pain is thought to be caused by ischemia resulting from vascular torsion and venous thrombosis. Intermittent symptoms may be attributed to spontaneous untwisting of the appendage, relieving the ischemia [3]. Clinically, the presentation can mimic other diseases such as cholecystitis, perforated peptic ulcer, pancreatitis and gastroesophageal reflux [2,3].In some cases, it presents as an acute abdomen, prompting surgical intervention. Despite the reported severity of symptoms, laboratory findings are often unremarkable [3,4].
Imaging findings of falciform ligament torsion and/or infraction have been described using ultrasound, CT, and MRI [3]. Although ultrasound did not focus on perihepatic fat in our case, several sonographic findings have been described in the literature. Coulier and Lloyd et al. described a heterogenous nodule that did not move with underlying structures during respiration [1,9]. Others have described ill-defined echogenicity with associated inflammatory changes [2]. CT findings are most frequently described and often include a well circumscribed heterogenous mass with increased fatty density and inflammatory changes [2,8]. Chieng et al described an ovoid fat density with attenuated peripheral rim surrounded by inflammatory changes near the falciform ligament [4]. In the index case, fat stranding compatible inflammatory changes around the falciform ligament were seen. The difference from the provided literature may be attributable to the active inflammation resulting in a heterogenous appearance of the fat. In our case,the diagnosis was also supported by MRI which showed progressive involution of the fat necrosis along the falciform ligament and anterior perihepatic space with early encapsulation, similar to the ovoid fat density described by Chieng et al on CT.
To our knowledge, our case is only the second case to characterize focal infarction of the falciform ligament using MRI. Justaniah et al reported the use of MRI in their case series and described findings of an ovoid hypointensity on T1 and T2 weighted MR images with rim enhancement on T1-weight post gadolinium [3]. These findings are similar to our findings as we also visualized post gadolinium rim enhancement, although hyperintensity about the area of fat necrosis on T2/ SPAIR imaging suggested ongoing inflammation and edema. MR imaging confirmed the findings initially seen on CT scan. Conservative management of falciform ligament fat infarction includes nonsteroidal anti-inflammatory medication and is often effective with resolution of symptoms within several weeks [2,4]. Surgical intervention has been reported in cases for increasingly severe abdominal pain [2], diagnostic uncertainty [3,4], or lack of awareness for alternative management [2,9]. While focal infarction of the falciform ligament is rare,its presentation is non-specific mimicking a wide differential of hepatobiliary, gastroduodenal, and pancreatic diseases [3]. Imaging can be diagnostic and therefore it is important for radiologists to recognize this pathology to avoid unnecessary surgical intervention
Declarations
Ethics approval and consent to participate: The study was approved by University of Arizona Institutional Review Board and was HIPAA-compliant. Volume 2 | Issue 5 | 2022 3 jcmimagescasereports.org
Consent for publication: The patient provided consent for publication.
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding: None.
Competing Interests: The authors report no competing interests.
Authors’ contribution
All authors noted above had access to data used in the research study and participated in writing the manuscript being submitted. All authors have read and approved the manuscript for submission. Hina Arif, MD
Acknowledgements: None.
References
- Coulier B, Cloots V, & Ramboux A. US and CT diagnosis of a twisted lipomatous appendage of the falciform ligament. European Radiology, 2001; 11(2): 213-215. [DOI:10.1007/s003300000570].
- Indiran V, Dixit R, & Maduraimuthu P. Unusual Cause of Epigastric Pain: Intra-Abdominal Focal Fat Infarction Involving Appendage of Falciform Ligament - Case Report and Review of Literature. GE - Portuguese Journal of Gastroenterology, 2017; 25(4): 179-183. [DOI:10.1159/000484528].
- Justaniah A, Scholz F, Katz D, & Scheirey C. Perigastric appendagitis: CT and clinical features in eight patients. Clinical Radiology, 2014; 69(12). [DOI:10.1016/j.crad.2014.08.020].
- Chieng J, Leow K, & Lim T. Clinics in diagnostic imaging (203). Singapore Medical Journal, 2020; 61(1): 15-18. [DOI:10.11622/smedj.2020006].
- Li XP, Xu DC, Tan HY & Li CL. Anatomical study on the morphology and blood supply of the falciform ligament and its clinical significance. Surgical and Radiologic Anatomy, 2014;26(2): 106-109. [DOI:10.1007/s00276-003-0184-0].
- Ozkececı ZT, Ozsoy M, Celep B, Bal A & Polat C. A Rare Cause of Acute Abdomen: An Isolated Falciform Ligament Necrosis. Case Reports in Emergency Medicine, 2014; 1-3. [DOI:10.1155/2014/570751].
- Beasley AW. Torsion of fatty tag in falciform ligament simulating perforated peptic ulcer. British Journal of Surgery, 1959;46(198): 423-423. [DOI:10.1002/bjs.18004619829].
- Vanderschueren L, & Coulier B. Focal Fat Infarction of theFalciform Ligament. Journal of the Belgian Society of Radiology, 2019; 103(1). [DOI:10.5334/jbsr.1793].
- Lloyd T. Primary torsion of the falciform ligament: Computed tomography and ultrasound findings. Australasian Radiology, 2006; 50(3): 252-254. [DOI:10.1111/j.1440-1673.2006.01573.x].