Case Report - Volume 2 - Issue 5
Uncommon indication for an Octopus technique in a symptomatic infected thoracoabdominal aneurysm after thoracic endoprosthesis
Justine Longchamp; Matthieu Zellweger; Sébastien Déglise*; Céline Deslarzes-Dubuis*
Vascular Surgery Department, Lausanne University Hospital (CHUV), Lausanne, Switzerland.
Received Date : July 30, 2022
Accepted Date : Sep 13, 2022
Published Date: Sep 17, 2022
Copyright:© Céline Deslarzes-Dubuis 2022
*Corresponding Author : Céline Deslarzes-Dubuis, Lausanne University Hospital, Rue du Bugnon 46, CH-1011 Lausanne, Switzerland.
Email:celine.deslarzes@chuv.ch
DOI: Doi.org/10.55920/2771-019X/1246
Abstract
Emergent thoraco-abdominal aneurysms (TAAA) repair remains challenging. Endovascular treatment should be considered in patients unfit for open surgery. Octopus technique is an off-the-shelf solution suitable for selected situations. We describe the successful treatment of a symptomatic and infected TAAA. A 66-year-old man presented to the emergency department with an infected 92mm TAAA with impending rupture due to Type 1b endoleak following previous TEVAR. 18FDG-PET-CT ruled out an endograft infection but diagnosed an aortitis.. Considering the emergent setting and his comorbidities, the patient was treated with the Octopus technique. Both renals were sacrificed and the celiac trunk was previously occluded, leaving the superior mesenteric artery the only target vessel. Treatment was successful and patient went home with a lifelong oral antibiotherapy. The 6-months angio-CT confirmed the absence of endoleak and patent superior mesenteric artery. The Octopus procedure can be used in selected cases for urgent endovascular TAAA repair in patients who are unfit for open repair.
Keywords: Thoracoabdominal aortic aneurysm; endovascular repair; endoleak; octopus technique.
Introduction
The repair of emergent thoraco-abdominal aneurysms (TAAA) remains challenging. Open surgery carries high rates of morbi-mortality [1]. Off-the-shelf branched endovascular devices can be a solution for the repair of TAAA in emergent cases. The Octopus technique [2]. (OT) entails bifurcated grafts in the thoracic segment in TAAA to access visceral arteries with multiples parallel covered stents. This appears to be an option with acceptable target vessels patency varying between 89-100% [3]. We describe the successful treatment of a symptomatic and infected TAAA with the OT.
Case Report
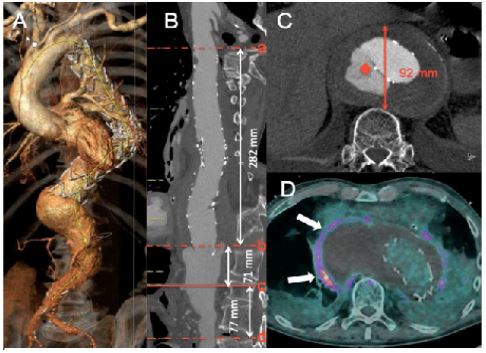
A 66 year-old man was referred to our emergency department for fever, and left back pain. He had a history of TEVAR for ruptured TAAA 2-years prior and was put on hemodialysis with no chance of recovery. Laboratory tests showed elevated white blood count 15.8 G/l (normal 4.0-10.0 G/l) and C-reactive protein (CRP) 483mg/l (normal < 5mg/l). Blood cultures were positive for Staphylococcus. Angio-CT evidenced a bulky 92mm Crawford type III TAAA, caused by a type 1b endoleak (Figure 1). Proximal coeliac trunk (CoT) was occluded following the TEVAR. 18F-FDG Positron emission tomography (PET-CT) ruled out a stentgraft infection but highlighted parietal hypermetabolism of the aneurysmal sac, hinting at an aortitis (Figure 1d). The presence of a type Ib endoleak and the impending rupture justified an urgent treatment. As patient was unfit for open surgery, we decided to sacrifie both renal arteries (RA) and secure superior (SMA) and inferior mesenteric arteries (IMA) using the OT.
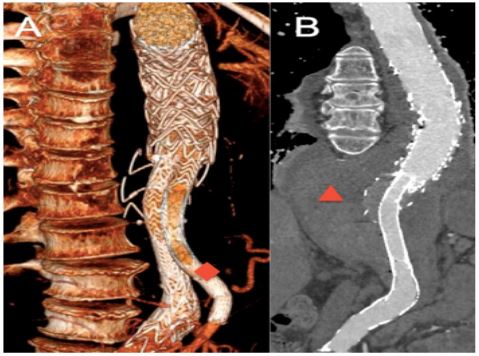
E-vita thoracic stentgraft (Jotec GmbH, Hechingen, Germany) was deployed in the previous graft followed by a Gore Excluder endoprosthesis (W.L Gore & Associates, Flagstaff, Ariz). SMA was catheterized from left axillary access through the ipsilateral leg opened just above it. Sealing was obtained with a Gore Viabahn distally and an Excluder HGB proximally. Stents were reinforced with self-expanding stents. Gore Excluder limbs and a Valiant (Medtronic, Santa Rosa, CA) endograft were used to prolonge the contralateral limb down to the infrarenal aorta above the IMA. The procedure lasted 133 minutes. The patient was discharged at post-operative day 25. Lifelong doxycycline was given. At 6 months follow-up, angio-CT confirmed the absence of endoleak and patent mesenteric arteries (Figure 2).
Figure 1: A: Three-dimensional CT reconstruction using 3mensio©.
B: Centerline analysis. a: endograft’s start, b: endograft’s end, c: CoT, d: IMA
C: CT showed type 1B endoleak (red diamond) and aneurysm (anterio-posterior diameter: 92 millimeters).
D: 18F-FDG Positron emission tomography showing parietal peri-aneurysmal hypermetabolism (white arrows).
Figure 2: A: Three-dimensional CT showing octopus branch in SMA (red diamond) and patent IMA (white arrow). B: Post-operative aneurysm exclusion (red triangle).
Discussion
Mortality rates of vascular graft infection at the thoracic level is up to 64%.. According to the guidelines [4], a bridging treatment was proposed due to the emergent setting. Although removal of the infected tissue and reconstruction in a clean field is recommended as definitive treatment, this was not an option for this high-risk patient.
The best strategy for thoracoabdominal aneurysm endovascular repair is fenestrated and branched endografts. The 2 existing off-the-shelf devices can accommodate a large number of anatomies in an emergent setting [5]. However, we selected an OT because the patient’s CeT was occluded and because both RA could be covered. His aortic anatomy was suitable for this technique, as there was no aortic thrombus, nor thoracic aortic tortuosity. Moreover, the simplicity of that technique offers additional advantages such as a reduced price and shorter intervention time. OT has been used in the US in the absence of FDA-approved branched devices for thoracoabdominal aneurysms. It is a useful technique to learn in Europe, as it could be life-saving for patients in urgent need of care and with no alternative. A series of 21 patients unfit for surgery treated with OT reported a technical success of 90% with a 30-days mortality of 9.5% confirming the good outcomes in critical patients3. With only one target vessel to revascularize, we used the OT in its easiest configuration with a single EVAR piece.
The OT is an attractive tool, providing an endovascular solution in emergency for high-risk surgical patients in selected cases. It should be part of the armentarium of every physician dealing with TAAA treatment.
References
- Coselli JS, LeMaire SA, Preventza O et al. Outcomes of 3309 thoracoabdominal aortic aneurysm repairs. J Thorac Cardiovasc Surg. 2016; 151: 1323–1337.
- Kasirajan K. Branched Grafts for Thoracoabdominal Aneurysms: Off-Label Use of FDA-Approved Devices. J Endovasc therapy. 2011;18: 471–476.
- Anahita Dua, Kedar S. Lavingia, et al. Early Experience with the Octopus Endovascular Strategy in the Management of Thoracoabdominal Aneurysms. Annals of Vascular Surgery. Volume 61, November 2019; 350-355.
- Chakfé N, Diener H, Lejay A, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur J Vasc Endovasc Surg. 2020 Mar; 59(3): 339-384.
- Spanos K, Kölbel T, Theodorakopoulou M, et al. Early Outcomes of the t-Branch Off-the-Shelf Multibranched Stent-Graft in Urgent Thoracoabdominal Aortic Aneurysm Repair. Journal of Endovascular Therapy. 2018; 25(1):3 1-39.