Case Report - Volume 2 - Issue 5
Cerebral Fat Embolism in the Absence of Intracardiac Shunting
Katerina Vraka1*; Vivian Tang2; Dipak Ram1
1Paediatric Neurology Department, Royal Manchester Children’s Hospital, Manchester, UK.
2Paediatric Radiology Department, Royal Manchester Children’s Hospital, Manchester, UK.
Received Date : Aug 22, 2022
Accepted Date : Sep 22, 2022
Published Date: Sep 30, 2022
Copyright:© Katerina Vraka 2022
*Corresponding Author : Katerina Vraka, Paediatric Neurology Department, Royal Manchester Children’s Hospital, Manchester, UK.
Email:Katerina.Vraka@mft.nhs.uk
DOI: Doi.org/10.55920/2771-019X/1255
Introduction
Cerebral fat embolism (CFE) is a rare phenomenon in paediatric settings and is usually seen post-trauma in patients with pre-existing intracardiac shunting. We present a rare case of CFE in the absence of cardiac anomaly.
Case
A sixteen-year-old, previously fit and well, boy sustained open fractures of the right lower limb, following a fall from a motorcycle, without reported head injury. His GCS was 15 at presentation. He underwent internal and external fixation of his multiple fractures. Post-operatively, he developed altered sensorium and abnormal posturing without respiratory compromise and did not require oxygen at any stage. He consequently had an urgent replacement of the external fixation with an MRI compatible intramedullary nail to facilitate imaging. MRI brain showed bilateral diffuse T2/FLAIR white and deep grey matter hyperintensities with diffusion restriction. These appearances were highly suggestive of cerebral fat embolism (CFE) (see Figures 1 to 4). Paradoxical embolism was excluded following a normal cardiac echocardiogram. Despite the extensive changes noted on brain imaging, he had an excellent recovery over a few weeks. On discharge, he was independently mobile with no neurological deficits and had no speech, swallowing or other significant difficulties.
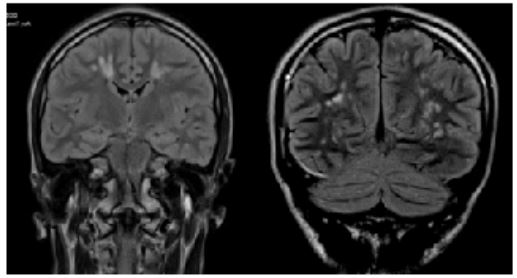
Figure 1: 1a and 1b Coronal FLAIR.
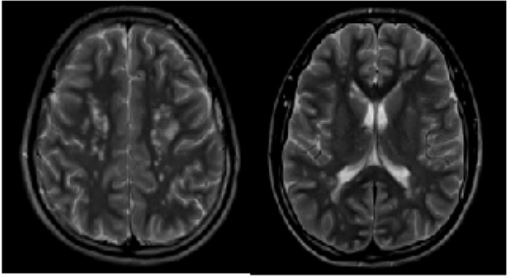
Figure: 2a and 2b Axial T2
FLAIR and T2 images demonstrated high signal foci abnormalities scattered bilaterally in deep and subcortical white matter, corpus callosum, basal ganglia and thalami.
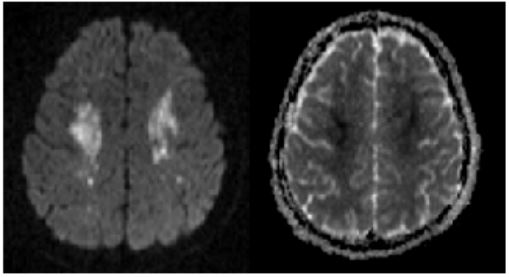
Figure: 3a DWI Fig 3b ADC
Centrum semi-ovale white matter diffusion restriction demonstrated on DWI and ADC map.
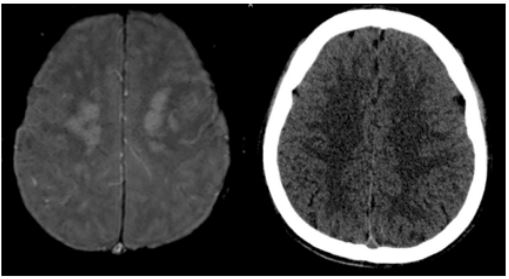
Figure: 4a SWI Fig 4b CT
No haemorrhage on SWI sequence.
Normal CT head.
Discussion
This case supports a rare, previously described [1] mechanism, where fat microglobules may sometimes be numerous (100 particles per mm2), too small (7-10μm) and malleable to cause pulmonary injury and can be filtered through the lung capillaries into the arterial circulation. Larger particles (>20μm) would get blocked by the pulmonary filter and cause respiratory symptomatology. When those fat microglobules reach the brain, they cause local ischaemia by mechanical obstruction of small vessels, release of inflammatory mediators and endothelial factors, along with platelet aggregation [2]. The symptoms onset is usually within the first 72 hours from the trigger. The neurological findings of CFE can vary from mild confusion to coma, headache, seizures, aggressive behaviour, hallucinations, memory problems, cortical visual impairment, and focal deficits (such as hemiplegia, dysphasia etc). Paroxysmal sympathetic activity with tachycardia, sweating, hypertension and hyperthermia has also been described [3]. The CT brain was normal and only MRI brain revealed diffuse abnormalities in our case, which underlines that MRI brain is the gold standard neuroimaging in order to diagnose CFE, something which is proposed by Lee et al. with the modified Gurd’s criteria [4]. In the acute phase, the most common finding has been described as “the starfield pattern”, with multiple, small scattered, hyperintense lesions in both the white and deep gray matter associated with innumerable scattered punctate foci of restricted diffusion on diffusion-weighed imaging and petechial haemorrhage on susceptibility-weighted imaging [2]. Our case supports this theory as the patient had no evidence of hypoxia at any stage and only had cerebral complications of fat embolism from a long bone fracture.
Conclusion
CFE is a condition with increased associated mortality and morbidity and should be considered in all patients with long bone or pelvic fractures who develop sudden onset neurological symptoms. Our case highlights that CFE can occur in the absence of intracardiac shunting or pulmonary symptoms.
Conflicts of Interest Disclosure: Nothing to declare.
References
- Eriksson EA, Schultz SE, Cohle SD, Post KW. Cerebral fat embolism without intracardiac shunt: A novel presentation. J Emerg Trauma Shock. 2011; 4(2): 309-312.
- Scarpino M, Lanzo G, Lolli F, Grippo A. From the diagnosis to the therapeutic management: cerebral fat embolism, a clinical challenge. Int J Gen Med. 2019; 12: 9-48.
- Mittal MK, Burrus TM, Campeau NG, Eckel LJ, Rabinstein AA, Wijdicks EF. Pearls & oy-sters: good recovery following cerebral fat embolization with paroxysmal hyperactivity syndrome. Neurology. 2013; 81(14): e107-109.
- Lee SC, Yoon JY, Nam CH, Kim TK, Jung KA, Lee DW. Cerebral fat embolism syndrome after simultaneous bilateral total knee arthroplasty: a case series. J Arthroplasty. 2012; 27(3): 409-414.