Case Report - Volume 2 - Issue 5
Endoscopic Variceal Therapy (EVT) may Increase the Risk of Portal Vein Thrombosis in Cirrhosis: A Clinical Case Report and Literature Review
Xin Yao; Hua Ni; Na Peng; Qi Qi; Lan-Jing Wang; Jian-Ping Qin*
Department of Gastroenterology, General Hospital of Western Theater Command, Chengdu 610083, Sichuan Province, China
Received Date : Aug 26, 2022
Accepted Date : Oct 05, 2022
Published Date: Oct 18, 2022
Copyright:© Jian-Ping Qin 2022
*Corresponding Author : Jian-Ping Qin, Department of Gastroenterology, General Hospital of Western Theater Command, No. 270 Rongdu Road, Chengdu 610083, Sichuan Province, China.
Email: jpqqing@163.com
DOI: Doi.org/10.55920/2771-019X/1267
Abstract
Background: Oesophagogastric varices (EGV) are a common complication occurring secondary to cirrhotic portal hypertension. Endoscopic methods are often used for primary prevention and treatment in such patients. However, it has been found in clinical practice that patients undergoing repeated endoscopic variceal therapy (EVT) may develop portal vein thrombosis (PVT). Herein, we reported the case of a patient with cirrhosis who developed PVT after repeated EVT and further progressed to cavernous transformation of the portal vein (CTPV) after anticoagulant therapy to learn from the clinical treatment of this patient. Written informed consent was obtained from the patient to publish this case report, including the attached imaging data.
Case Summary: We reported the case of a patient with cirrhosis who developed PVT after repeated EVT and further progressed to cavernous transformation of the portal vein (CTPV) after anticoagulant therapy to learn from the clinical treatment of this patient. Written informed consent was obtained from the patient to publish this case report, including the attached imaging data.
Conclusion: EVT may increase the risk of PVT in patients with cirrhosis, which may be related to the changes in portal venous hemodynamics and hemorheology.
Keywords: Endoscopic Variceal Therapy; Portal Vein; Thrombosis; Cirrhosis.
Core Tip: Oesophagogastric varices (EGV) are a common complication occurring secondary to cirrhotic portal hypertension. Endoscopic methods are often used for primary prevention and treatment in such patients. However, it has been found in clinical practice that patients undergoing repeated endoscopic variceal therapy (EVT) may develop portal vein thrombosis (PVT). Herein, we reported the case of a patient with cirrhosis who developed PVT after repeated EVT and further progressed to cavernous transformation of the portal vein (CTPV) after anticoagulant therapy to learn from the clinical treatment of this patient.
Introduction
Oesophagogastric varices (EGV) are a common complication of cirrhotic portal hypertension, for which endoscopic variceal therapy (EVT) is always used as the means of primary prevention and treatment. However, repeated EVT may lead to portal vein thrombosis (PVT). A meta-analysis [1] involving 833 patients from 13 studies showed that the overall incidence of PVT after EVT was 10.4% (95% CI, 4.9–17.7%), with a statistically significant difference (I2 = 83.3%, P < 0.0001). Currently, there is no prospective study confirming the correlation between ETV and PVT or exploring the effect of PVT secondary to EVT on the prognosis of patients with cirrhosis. Herein, we reported the case of a patient with cirrhosis who developed PVT after repeated EVT and further progressed to cavernous transformation of the portal vein (CTPV) and reviewed the literature, aiming to deeply explore the correlation between ETV and PVT.
Case presentation
Chief complaints: A 46-year-old male patient was admitted to the hospital because of recurrent haematemesis and melena.
History of present illness: The patient had a history of hepatitis B for 20 years, had been receiving antiviral therapy with entecavir dispersible tablets since 2016, and underwent regular hepatitis B virus quantification, which was continuously negative.
History of past illness: The patient had hepatitis B liver cirrhosis and acute variceal bleeding accompanied.
Personal and family history: The patient had no special personal history or family history.
Physical examination: Soft abdomen; severe splenomegaly with palpable edges of the spleen at the umbilical level, no tenderness, rebound tenderness or muscle tension and not reaching the subcostal liver; and positive shifting dullness.
Laboratory examinations: The results of laboratory examinations were Child-Pugh grade A liver function and a Model for End-stage Liver Disease (MELD) score of 12.
Imaging examinations: Enhanced abdominal computed tomography (CT) revealed portal hypertension and collateral circulation with cirrhosis.
Final Diagnosis
After admission, the patient was diagnosed with hepatitis B cirrhosis, acute variceal bleeding.
Treatment
The patient underwent endoscopic variceal ligation for oesophageal varices six times in our hospital in July 2016, May 2017, June 2017, 14 January 2019, 5 March 2019 and 15 April 2019, respectively. On 23 July 2019, the patient underwent endoscopic sclerotherapy and intravenous injection of tissue glue to the gastric fundus for segmental oesophageal varices.
Outcome and Follow-Up
He fibrinogen concentration (g/L) increased to 2.05 g compared with 1.45 g in July 2016, and the platelet count (10^9/L) increased to 40 compared with 25 in July 2016. During this period, propranolol hydrochloride tablets were orally administered, 10 mg/dose, 3 times/day and the heart rate was controlled at 55–60 beats/min. On 16 October 2019, abdominal enhanced CT suggested embolus formation in the right portal vein (RPV) and main portal vein (MPV) (Figure 1–2). In addition, fibrinogen concentration was 1.85 g/L, and platelet count was 45*109/L. A transjugular intrahepatic portosystemic shunt (TIPS) combined with oral warfarin sodium tablets, 2.5 mg/dose, 1 time/day was recommended for the patient. After that, the INR was controlled at approximately 2.0. On 27 December 2021, abdominal enhanced CT suggested strip filling defects in the RPV, MPV and proximal superior mesenteric vein (SMV), which were considered as embolus formation and aggravated compared with that on 16 October 2019(Figure 3–4). The fibrinogen concentration was 1.95 g/L, and the platelet count was 55*109/L. TIPS was further recommended for the patient, but he refused (In China, most patients prefer endoscopic treatment due to its low single cost and high reimbursement rate). On 22 March 2022, CT angiography of the portal vein displayed strip filling defects in the RPV, MPV and proximal SMV, and the emboli in the MPV increased compared with those on 28 December 2021(Figure5–6)., accompanied by cavernous transformation. The fibrinogen concentration was 1.87 g/L, and the platelet count was 60*109/L.
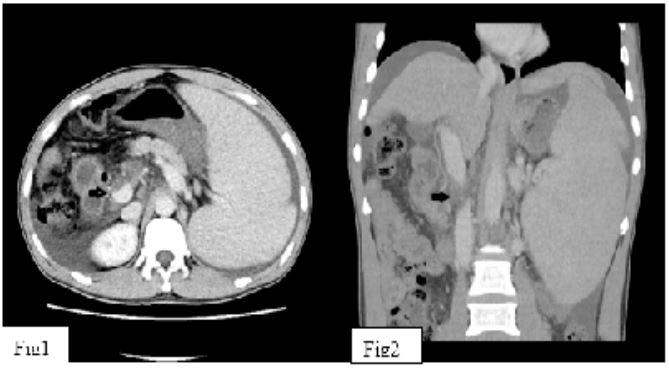
Figure 1–2: On 16 October 2019, abdominal enhanced CT suggested embolus formation in the RPV and MPV.

Figure 3–4: On 27 December 2021, abdominal enhanced CT suggested strip filling defects in the RPV, MPV and proximal SMV, which were considered as embolus formation and aggravated compared with that on 16 October 2019.
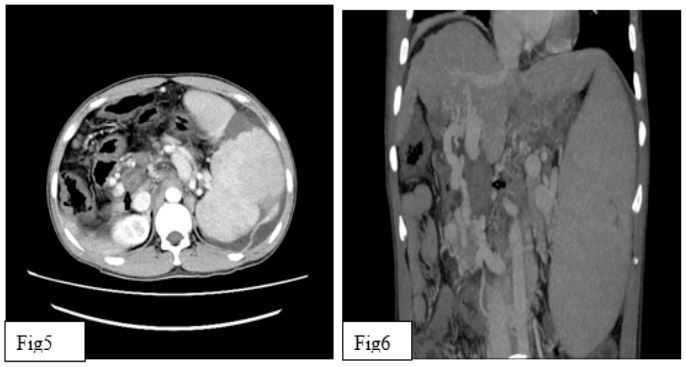
Figure 5–6: On 22 March 2022, CT angiography of the portal vein displayed strip filling defects in the RPV, MPV and proximal SMV, and emboli in the MPV increased compared with those on 28 December 2021, accompanied by cavernous transformation.
Discussion
According to a previous US study [2], cirrhosis causes portal hypertension due to hepatic sinusoidal obstruction syndrome, perisinusoidal fibrosis and blocked portal circulation, thereby resulting in reduced and slow blood flow in the liver. At present, it has been confirmed that [3-5] PVT involves multiple factors, including hypercoagulable state, endothelial injury and slow portal vein blood flow. In this case, EVT might lead to mechanical injury of local vascular endothelium and activation of endogenous coagulation [6], in particular, endoscopic intravenous tissue glue injection into the stomach could cause histological changes in the portal vein [7], which might be one of the causes for subsequent thrombosis. In addition, ETV changed the hemodynamics of the portal vein. At present, studies [8-9] have shown that portal vein blood flow increases after ETV, accompanied by turbulence and pooling and portal vein pressure increases, which may increase the probability of portal vein thrombus formation and development. Both the 2019 Chinese Operation Guidelines for TIPS [10] and the 2021 North American Operation Guidelines for TIPS [11] pointed out that PVT was one of the surgical indications of TIPS. Nevertheless, the patient refused TIPS after PVT. Although anticoagulant therapy was given when portal vein pressure could not be effectively controlled, thrombosis was still progressively aggravated, resulting in CTPV. It can be predicted that PVT will aggravate portal hypertension, increase the risk of oesophagogastric variceal bleeding (EGVB), reduce intrahepatic portal perfusion and damage the compensatory function of the liver. If thrombosis involves the SMV and splenic vein, it may cause severe complications such as intestinal infarction and splenic infarction [10], which increases the risk of death in patients with cirrhosis [12] and the technical difficulty in liver transplantation [13]. Therefore, we will follow up and pay attention to the prognosis of this patient.
Factors including widening of portal vein diameter, deterioration of liver function and large blood flow in the portal collateral circulation have been considered risk factors of PVT [14-17]. Although the risk factors of PVT have been studied, some hemorheological indexes have been ignored. As an important organ of hemorheology, the liver synthesises plasma proteins, lipids and coagulation factors. Additionally, the liver also plays an important and decisive role in hemorheology [18]. Due to the low concentration of fibrinogen, albumin and other large proteins in the body, plasma viscosity is low [19]. Jang Bohyun et al. [20] reported that fibrinogen increased with the increase in the inflammatory response and other macromolecular proteins. Chaudhary A et al. [21] found that ETV could lead to fibrosis of the splenic vein, and local inflammation may increase the blood viscosity of the portal vein system. Harding DJ et al. [22] believed that after splenectomy, local vascular intima of the portal vein system was damaged, and an inflammatory reaction and platelet adhesion and aggregation occurred, which was likely to cause PVT or mesenteric thrombosis. In this case, fibrinogen and platelet counts after ETV were higher than those before surgery. We speculate that because patients with cirrhosis have adapted to low blood viscosity for a long time, local vascular intimal damage and inflammatory reaction will also occur in the portal vein system after ETV, accompanied by platelet adhesion and aggregation and increased blood viscosity, resulting in the formation and progression of the portal vein or mesenteric thrombus. This patient was treated with anticoagulant therapy after the detection of PVT, but the progression of thrombosis could not be avoided. We believe that blood viscosity is affected by the haematocrit, fibrinogen, albumin, erythrocyte deformation and aggregation and plasma viscosity. Moreover, in patients with cirrhosis whose portal hypertension cannot be effectively controlled and hemodynamics of the portal vein system cannot be changed, whether anticoagulant therapy alone can prevent the progression of PVT is worthy of further exploration.
In conclusion, based on clinical practice, it is common for cirrhotic patients to develop PVT after EVT. Therefore, further prospective studies are needed to confirm their correlation and to explore the effect of PVT after EVT on the prognosis of patients with cirrhosis.
Conclusions
EVT may increase the risk of PVT in patients with cirrhosis, which may be related to the changes in portal venous hemodynamics and hemorheology.
Author contributions: Yao X performed the operation and wrote the paper; Ni H, Peng N collected the data; Qi Q , Wang LJ collected the data; Qin JP participated in and guided the operation, conceptualized the idea, and finalized the manuscript
References
- Wang L, Guo X, Xu X, Philips CA, Primignani M, Mendez-Sanchez N, Li Q, Zheng K, Qi X. Association of portal venous system thrombosis with endoscopic variceal treatment: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2021 Feb 1; 32(2): 125-131. [PMID: 32501878 DOI: 10.1097/MEG.0000000000001774].
- Ljubicić N, Duvnjak M, Rotkvić I, Kopjar B. Influence of the degree of liver failure on portal blood flow in patients with liver cirrhosis. Scand J Gastroenterol. 1990 Apr; 25(4): 395-400. [PMID: 2186474 DOI: 10.3109/00365529009095505].
- Stine JG, Northup PG. Management of non-tumoral portal vein thrombosis in patients with cirrhosis. Dig Dis Sci 2019; 64: 619–626. [PMID: 30560339 DOI: 10.1007/s10620-018-5427-3].
- Qi X, Li H, Liu X, Yao H, Han G, Hu F, et al. Novel insights into the development of portal vein thrombosis in cirrhosis patients. Expert Rev Gastroenterol Hepatol 2015; 9: 1421–1432. [PMID: 26325361 DOI:10.1586/17474124.2015.1083856].
- Stine JG, Wang J, Shah PM, Argo CK, Intagliata N, Uflacker A, et al. Decreased portal vein velocity is predictive of the development of portal vein thrombosis: a matched case-control study. Liver Int 2018; 38:94-101. [PMID: 28632958 DOI: 10.1111/liv.13500].
- Bosch J, Berzigotti A. Letter: nonselective beta-blockers, endoscopic therapy and portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther 2019; 49: 1370–1371. [PMID: 31016776 DOI: 10.1111/apt.15236].
- Hunter GC, Steinkirchner T, Burbige EJ, Guernsey JM, Putnam CW. Venous complications of sclerotherapy for esophageal varices. Am J Surg 1988; 156: 497–501. [PMID: 3264465 DOI: 10.1016/s0002-9610(88)80538-5].
- Ohnishi K, Nakata H, Terabayashi H, Tanaka H, Tsunoda T, Iida S, Nomura F. The effects of endoscopic sclerotherapy combined with transhepatic variceal obliteration on portal hemodynamics. Am J Gastroenterol 1987; 82: 1138–1142. PMID: 3673992.
- Sugimoto K, Shiraki K, Murata K, Ito T, Ohmori S, Sakai T, et al. The effect of endoscopic injection sclerotherapy on portal blood flow and liver function. Hepatogastroenterology 2002; 49: 1587–1590. PMID: 12397742.
- Chinese College of Interventionalists. [CCI clinical practice guidelines: management of TIPS for portal hypertension (2019 edition)]. Zhonghua Gan Zang Bing Za Zhi 2019; 27: 582-593 [PMID: 31594075 DOI: 10.3760/cma.j.issn.1007-3418.2019.08.002]
- Boike JR, Thornburg BG, Asrani SK, Fallon MB, Fortune BE, Izzy MJ, et al. Advancing Liver Therapeutic Approaches (ALTA) Consortium. North American Practice-Based Recommendations for Transjugular Intrahepatic Portosystemic Shunts in Portal Hypertension. Clin Gastroenterol Hepatol. 2021 Jul 15: S1542-3565(21)00749-7. [PMID: 34274511 DOI: 10.1016/j.cgh.2021.07.018].
- Stine JG, Shah PM, Cornella SL, Rudnick SR, Ghabril MS, Stukenborg GJ, Northup PG. Portal vein thrombosis, mortality and hepatic decompensation in patients with cirrhosis: a meta-analysis. World J Hepatol 2015; 7: 2774–2780. [PMID: 26644821 DOI: 10.4254/wjh.v7.i27.2774].
- Talwar Abhinav, Varghese Jeffrey, Knight Gabriel M, Katariya Nitin, Caicedo Juan-Carlos, Dietch Zach, Borja-Cacho Daniel, Ladner Daniella, Christopher Derrick, Baker Talia, Abecassis Michael, Mouli Samdeep, Desai Kush, Riaz Ahsun, Thornburg Bart, Salem Riad. Preoperative portal vein recanalization-transjugular intrahepatic portosystemic shunt for chronic obliterative portal vein thrombosis: Outcomes following liver transplantation. Hepatol Commun, undefined(undefined), undefined. 2002. [DOI:10.1002/hep4.1914 PMID: 35220693].
- Kuroki T, Kitasato A, Tokunaga T, et al. Predictors of portal and splenic vein thrombosis after laparoscopic splenectomy: A retrospective analysis of a single-center experience. Surg Today. 2018; 48(8): 804-9. [PMID: 29569060 DOI: 10.1007/s00595-018-1655-6].
- Qi X, Li H, Liu X, et al. Novel insights into the development of portal vein thrombosis in cirrhosis patients. Expert Rev Gastroenterol Hepatol. 2015; 9(11): 1421-32. [PMID: 26325361 DOI: 10.1586/17474124.2015.1083856].
- Dai J, Qi X, Peng Y, et al. Association between D-dimer level and portal venous system thrombosis in liver cirrhosis: A retrospective observational study. Int J Clin Exp Med. 2015; 8(9): 15296-301 PMID: 26629017.
- Zhang X, Wang Y, Yu M, et al. effective prevention for portal venous system thrombosis after splenectomy: A meta-analysis. J Laparoendosc Adv Surg Tech A. 2017; 27(3): 247-52. [PMID: 28296630 DOI: 10.1089/lap.2016.0511].
- Liu TT, Wong WJ, Hou MC, et al. Hemorheology in patients with liver cirrhosis: Special emphasis on its relation to severity of esophageal variceal bleeding. J Gastroenterol Hepatol. 2006; 21(5): 908-13. [PMID: 16704544 DOI: 10.1111/j.1440-1746.2006.04266.x].
- Robertson DA, Simpson FG, Losowsky MS. Blood viscosity after splenectomy. Br Med J (Clin Res Ed). 1981; 283(6291): 573-75. [PMID: 6790084 DOI: 10.1136/bmj.283.6291.573].
- Jang Bohyun, Han Ji Won, Sung Pil Soo, Jang Jeong Won, Bae Si Hyun, Choi Jong Young, Cho Young I, Yoon Seung Kew. Hemorheological Alteration in Patients Clinically Diagnosed with Chronic Liver Diseases. J Korean Med Sci, 2016; 31(12): 1943-1948. [PMID: 27822933 DOI:10.3346/jkms.2016.31.12.1943].
- Chaudhary A, Tatke M, Aranya RC. Endoscopic sclerotherapy: the far and near effects. Br J Surg 1990; 77: 963. [PMID: 2207585 DOI: 10.1002/bjs.1800770904].
- Harding DJ, Perera MT, Chen F, et al. Portal vein thrombosis in cirrhosis: Controversies and latest developments. World J Gastroenterol. 2015; 21(22): 6769-84. [PMID: 26078553 DOI: 10.3748/wjg.v21.i22.6769]

