Case Report - Volume 2 - Issue 5
Phlegmasia cerulea dolens and covid 19: a case report and review of the literature
B Dahmani*; EM Choukri; Z Moudafia; S Omari Tadlaoui; FZ Oufquir ; S Alaoui Rachidi
Radiology Department, CHU Tanger Tétouan Al Hoceima, Faculty of Medicine and Pharmacy of Tanger, Abdelmalek Essaadi University, Tanger, Morocco.
Received Date : Aug 26, 2022
Accepted Date : Oct 07, 2022
Published Date: Oct 22, 2022
Copyright:© B Dahmani 2022
*Corresponding Author : B Dahmani, Radiology Department, CHU Tanger Tétouan Al Hoceima, Faculty of Medicine and Pharmacy of Tanger, Abdelmalek Essaadi University, Tanger, Morocco.
Email: dahmani199302@outlook.fr
DOI: Doi.org/10.55920/2771-019X/1271
Abstract
Phlegmasia cerulea dolens is a manifestation of peripheral venous thrombosis leading to arterial is chaemia.
It is a rare and serious complication that can be life-threatening and functionally challenging. It has a suggestive clinical presentation and is diagnosed by vascular ultrasound. We report a case of blue phlebitis in a 28 year old covid positive woman.
Keywords: Covid 19 ; peripheral venous thrombosis; arterial ischaemia.
Introduction
Phlegmasia cerulea dolens (blue phlebitis) is a rare condition caused by complete venous occlusion resulting in impaired arterial flow. It most often develops in a medically fragile patients.
Observation
This is a 28 year old female patient followed for polycystic ovarian syndrome under oral contraception, who has been presenting for a week with asthenia and cough motivating her consultation, and given the pandemic context a PCR was requested which came back positive for sars cov2 pneumopathy, the symptomatology worsened 6 days after the onset of symptoms with the sudden appearance of a hot and painful red swelling of the left lower limb which became tense and bluish 3 hours later, prompting her consultation in the covid care unit, On physical examination, the patient was apyretic at 35°C, tachycardic at 145 beats per minute, polypneic at 35cpm and normotensive at 115/90 Mhg, with a left lower limb that was very painful on palpation, with diffuse non-pitting edema, with a blue colouration and a weak pulse. (Figure 1)
On Doppler ultrasound: Deep venous thrombosis from the left primitive iliac vein extending to the entire deep venous network of the homolateral lower limb, with extension to the superficial network, the common femoral vein is very increased in calibre surrounded by a significant perivascular infiltration and compressing the adjacent artery. (Figure 2).
Phleboscan: showed massive deep vein thrombosis of the left lower limb extending from the left iliac vein compressing the arterial network (Figure 3)
Thoracic angioscan showed an enhancement defect of a sub-segmental branch of the right inferior lobar artery, with a few bilateral, basal predominant, peripheral ground glass lung foci (Figure 4).

Figure 1: Left lower limb with diffuse tense edema with bluish discolouration.

Figure 2: Venous Doppler of the left lower limb showing (a):thrombus of the superficial femoral vein extending to the long saphenous vein(b) thrombus of the popliteal vein(c).
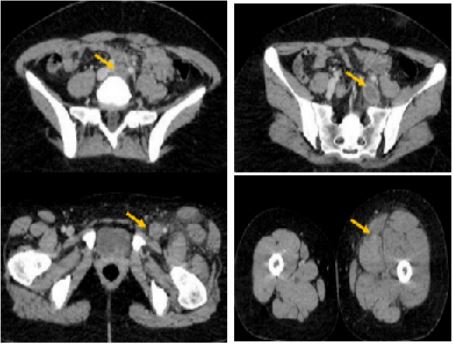
Figure 3: Phleboscan showing massive deep vein thrombosis of the left lower limb extending from the left primitive iliac vein compressing the arterial network of the left lower limb subinguinal (arrows). network of the left lower limb subinguinal (arrows).
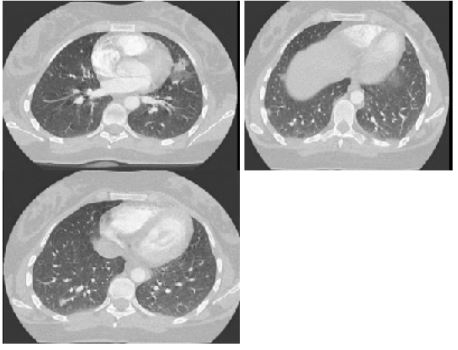
Figure 4: Axial CT parenchymal window slices showing a bilateral peripheral and basal ground glass lung foci.
Discussion
Phlegmasia cerulea dolens (PCD) is a manifestation of peripheral venous thrombosis associated with signs of arterial ischaemia [2]. Increased interstitial pressure and hypovolaemia lead to arterial collapse, distal tissue ischaemia and venous gangrene [3]. Although phlegmasia cerulea dolens can be treated at an early stage, the accompanying complications have a detrimental effect on the patient's quality of life [2].
Phlegmasia cerulea dolens continues to have mortality and amputation rates of 25% to 40% and 20% to 50% respectively [5-6], so multiple factors can induce it, including heart disease, malignancy, hypercoagulability and central venous catheter implantation [7]. The clinical presentation of PCD includes the following triad: oedema, cyanosis and pain in the affected extremity.
The diagnosis is essentially clinical and based on the three cardinal signs, confirmed by imaging. Duplex ultrasound has become the preferred imaging modality for the diagnosis of DVT due to its availability and non-invasive nature. Phleboscan and phlebo-MRI are rarely used but can help determine the proximal and distal extent of the thrombus. Therapeutic anticoagulation with urgent thrombolytic therapy or mechanical thrombectomy can help save the limb [8-9], reperfusion injury and post-thrombotic syndrome can develop even in successfully treated patients.
Our patient was hospitalized in a covid unit with urgent curative anticoagulation, The subsequent evolution was marked by a clinical improvement made of a disappearance of the coldness of the lower limb with a well perceived distal pulse.
Conclusion
Phlegmasia cerulea dolens is a serious complication if not treated quickly and effectively Doppler ultrasonography is the imaging method to be indicated first thanks to its rapidity, availability and sensitivity in making a positive diagnosis, Management consists of two main therapeutic components: anticoagulation and mechanical recanalisation or thrombolysis.
References
- Perkins JMT, Magee TR, Galland RB. Phlegmasia caerulea dolens and venous gangrene. Br J Surg. 1996; 83: 19-23
- Case Report Phlegmasia Cerulea Dolens in the Upper Extremity: A Case Report and Literature Review
- Burihan E, Figueiredo LFPD, Francisco Júnior J, et al. Upper-extremity deep venous thrombosis: analysis of 52 cases. Cardiovasc Surg 1993; 1: 19–22.
- Tung CS, Soliman PT, Wallace MJ, Wolf JK, Bodurka DC. Successful catheter-directed venous thrombolysis in phlegmasia cerulea dolens. Gynecol Oncol 2007; 104: 140-2.
- Perkins JMT, Magee TR, Galland RB. Phlegmasia caerulea dolens and venous gangrene. Br J Surg. 1996; 83: 19-23.
- Bhatt S, Wehbe C, Dogra VS. Phlegmasia cerulea dolens. J Clin Ultrasound. 2007; 35(7): 401-404.
- Case Report Phlegmasia Cerulea Dolens in the Upper Extremity: A Case Report and Literature Review Jie Zhang, Yanyang Wang, Yali Du, and Liang Zhao Hood DB, Weaver FA, Modrall JG, et al. Advances in the treatment of phlegmasia cerulea dolens. Am J Surg 1993; 166: 206–10.
- Weaver FA, Meacham PW, Adkins RB, et al. Phlegmasia cerulea dolens: therapeutic considerations. South Med J 1988; 81: 306–12.
- Abhishek Maiti,1 Avash Das,2 Daniel T Smith3, Phlegmasia cerulea dolens

