Case Report - Volume 2 - Issue 5
Malaria And Typhoid Co – Infection Among Patients Attending Some Selected Healthcare Facilities In Kawo Metropolis, Kaduna State, Nigeria
Eke Samuel Sunday*; Ucheh Bernadette Ifeoma; Owoh – Etete Ukamaka1; Michael Nancy Erika
Biology Unit, Air Force Institute of Technology, Kaduna, Kaduna State – Nigeria
Received Date : Aug 30, 2022
Accepted Date : Oct 09, 2022
Published Date: Oct 25, 2022
Copyright:© Eke Samuel Sunday 2022
*Corresponding Author : Eke Samuel Sunday, Biology Unit, Air Force Institute of Technology, Kaduna, Kaduna State – Nigeria.
Email: ekesamuel2012@gmail.com
DOI: Doi.org/10.55920/2771-019X/1273
Abstract
Malaria and typhoid fever are two leading infections of poverty with serious health and socioeconomic impacts, and due to their geographical overlap, co-infections are very common. Their mimicking symptomatology often present with gross misdiagnosis and mistreatment. This study was carried out to determine the incidence of malaria and typhoid co-infections among adult population attending some selected healthcare facilities in Kawo Metropolis, Kaduna, Kaduna State. A cross-sectional study was conducted on Two hundred and seventy six (276) patients. Venous blood samples were collected for Widal and Malaria tests, respectively. The Widal agglutination test was performed by the rapid slide titration method using commercial antigen suspension while the Malaria diagnosis was carried out using antigen based- Rapid Diagnostic Test (RDT). Out of the 276 blood samples analyzed, 184 (66.67%) were positive for malaria, 143 (51.81%) were positive for Salmonella typhi, while 132 (47.83%) were positive for both typhoid and malaria co – infection. However, the prevalence of malaria parasite was statistically significant in relation to sex (p<0.05), as males had 75 (40.76%) prevalence and females, 109 (59.24%). The highest prevalence of typhoid fever was recorded in males 87 (60.84%) while females had the lowest prevalence of typhoid fever 56 (39.16%). Both malaria and typhoid were prevalent among the studied population with high rate of co-infection. Co-infection was higher in females than males and use of herbal medicine for treatment was common. Efforts should be made to improve on the living conditions of the people of Kawo and also, there should be public enlightenment on the preventive and control measures of the two diseases. Since both diseases have similar symptomatology, treatment should be based on adequate laboratory diagnosis. Also, personal hygiene is hereby encouraged among the populace.
Keywords: Malaria; Typhoid Fever; Salmonella; Kawo and Co – infection.
Introduction
Malaria is a life threatening disease caused by five species of protozoan parasite of the genus Plasmodium (P. falciparum, P. vivax, P. malariae, P. ovale and P. knowlesi) that is transmitted to humans through the bites of an infected 34 female anopheles mosquito [1,2,3]. Nearly all human deaths by malaria are caused by P. falciparum, mainly in sub-Saharan Africa. Globally, an estimated 3.3 billion people in 97 countries and territories are at risk of being infected with malaria and developing disease and 1.2 billion are at high risk [3,4]. It is estimated that 198 million cases of malaria occurred globally in 2013 and the disease led to 584,000 deaths representing a decrease in malaria case incidence and mortality rates of 30% and 47% since 2000, respectively [5,6]. It is considered a disease of poverty and duly recognized as a public health problem with overwhelming medical, social and economic implications. Malaria exacts a heavy burden on the poorest and most vulnerable communities of which the people of Kawo metropolis, Kaduna State is not an exception. Within endemic countries, the poorest and most marginalized communities are the most severely affected, having the highest risks associated with malaria, and the least access to effective services for prevention, diagnosis and treatment [7]. Typhoid fever is a bacterial infection due to Salmonella typhi. Salmonella’s genus is Gram-negative, motile, non-sporing, non-capsulate bacilli which exist in nature primarily as parasites of the intestinal tract of man and other animals [8].
Salmonella typhi and the paratyphoid bacilli are found only in the intestinal tract of man for whom they have a high degree of pathogenicity and in which they frequently cause invasive disease that causes symptoms which may vary from mild to severe and usually begin six to thirty days after exposure with gradual onset of a high fever after several days [9,10]. Weakness, abdominal pain, constipation, and headaches are the commonest symptoms. Some people develop a skin rash with rose colored spots. Without treatment, symptoms may last for weeks or months. Other people may carry the bacterium without symptoms; however, they are still able to spread the disease to others [11,12].
Typhoid and malaria fever are two leading febrile illness affecting humans, especially in sub-Saharan Africa. They remain the diseases of major public health importance and the cause of morbidity and mortality. An association between malaria and typhoid fever was first described in 1862 in North America as an entity called typho-malaria fever [10,13]. It is acquired by the ingestion of food and/or water contaminated with the faeces of an infected person, which contain the bacterium, Salmonella enteric serovar typhi; humans are the only infected [1,14]. Risk factors include poverty as a result of poor sanitation and poor hygiene [15]. In the year 2000 and 2010, an estimated 21.7 million and 13.5 million typhoid fever illnesses were recorded. Between years 2000 and 2013, it resulted in estimated 217,000 and 161,000 deaths respectively [16,17]. Infants, children, and adolescents in south-central and Southeast Asia experience the greatest burden of illness [18,19]. Nonetheless, outbreaks of typhoid fever are frequently reported from sub-Saharan Africa and countries in Southeast Asia [20,21].
Due to the geographical overlap of both infections, co-infections are very common. However, the precise incidence of the concurrent malaria and typhoid fever in most geographical areas is largely uncertain, as both share social circumstances which are imperative to their transmission; individuals in areas endemic for both diseases are at substantial risk of contracting both these diseases, either concurrently or an acute infection superimposed on a chronic one [22]. While high prevalence of malaria is an established fact, it is only within the last decade that an unusually high number of illnesses have been diagnosed as malaria co-existing with typhoid fever [23,24,25]. Malaria and typhoid fever often present with mimicking symptoms especially in the early stages of typhoid fever [23,25]. The situation often presents a diagnostic problem and in some cases could lead to diagnostic confusion. As a result of this, the importance of definitive laboratory-based diagnosis cannot be overstated, before an individual is said to have concurrent malaria and typhoid fever, the presence of Plasmodium species and Salmonella enteric sub-sp enterica serotype typhi must be demonstrated in the patient’s laboratory specimens [26].
Both diseases are common in many countries of the world where poor sanitary habit, poverty and ignorance exist. The first non-specific manifestations include fever, headache, abdominal pain and vomiting. Despite the importance of concurrent malaria and typhoid fever in the tropics, the challenges associated with the diagnosis and the public health implications have not been comprehensively reviewed. Hence, this paper presents a study carried out to determine the prevalence of malaria, typhoid and their confection in Kawo Metropolis, Kaduna, Kaduna State State.
Materials and Methods
Study area
The study was conducted in five (5) different healthcare facilities Kawo Metropolis. Kaduna State is a state of the Federal Republic of Nigeria located in the northwestern geopolitical zone of the country. It takes its name for the capital of Kaduna, hence it is usually referred to as Kaduna State to distinguish the two. It is ranked 4th by land area and 3rd by population in Nigeria. The state capital was the former capital city of the British protectorate of Northern Nigeria region (1923–1966) fter Zungeru (1903–1923) and Lokoja (1897–1903). Other major urban areas include Zaria, Kagoro, Kafanchan, Kachia, Nok, Makarfi, Birnin Gwari and Zonkwa.
Kaduna is one of the largest centers of education in Nigeria. The slogan of the state is Center of Learning because of the presence of many institutions like Ahmadu Bello University (established 1962), Nigeria Defense Academy (NDA), Air Force Institute of Technology (Air Force University) etc. There are many government schools, include primary schools and secondary schools. All secondary schools in Kaduna are owned by the state government, federal government or private organizations. There are many tertiary institutions in the state.
Sampling design
Two hundred and seventy six (276) adults were randomly sampled across the selected healthcare facilities for this study, irrespective of their sex, age and department.
Sample collection
Five millilitres (5ml) of blood sample was collected from each patient into sterilized EDTA tube by trained phlebotomist.
Malaria diagnosis using antigen based- rapid diagnostic test (RDT)
The test kit was detached from its seal and the blood from the EDTA bottle was blotted into sample window (S) present on the test kit, two drops of Malaria parasite test kit buffer was added to the blood sample in the sample window (S) and allowed to flow through the chamber labeled test (T) and control (C) windows. The test was allowed to run for 10mins. The appearance of coloured band line at the control window (C) only, indicates a valid but negative test while coloured band lines appearing at the test window (T) and control window (C) indicates a positive test. If there was no redline appearing at the control window (C), it is thus interpreted as invalid and the test is repeated [27].
Widal test
The agglutination test was performed on all blood samples by the rapid slide titration method using Cal-Test Diagnostic Inc. Chino, U.S.A. Widal commercial antigen suspensions, for the somatic (O) and flagella (H) antigens by adding one drop of the widal antigen suspension to the reaction circles containing the patient’s serum. The content of each circle was uniformly mixed over the entire circle with separate mixing sticks. The slides were gently rocked back and forth, and observed for agglutination for one minute. A positive widal test was considered for any serum sample with antibody titre ≥ 1:160 to the O and H antigens of S. typhi [27].
Ethical Considerations
Prior to the study, ethical approval was obtained from Research and Ethics Committee of the Kaduna State Ministry of Health, while permission was obtained from the community heads. Consent was sought and obtained from participants or their relations and only those who gave their consents were enrolled into this study. Information or results obtained from the study was treated with utmost confidentiality and used for the purpose of the research only.
Statistical analysis
Data were analyzed using statistical package for social sciences (SPSS) version 23.0 (Chicago, USA). Chi-square (χ2) was used to determine if the relationships between the Malaria parasite infection and Salmonella typhi were actually significant.
Results
Blood samples were collected from a total of 276 patients. These blood samples were examined for the presence of malaria parasites, typhoid fever and malaria/typhoid co-infection in relation to Healthcare facility and Gender and the results are presented below.
Prevalence of Malaria Parasite
Of the 276 (100%) patients screened and tested for malaria parasites, 184 (66.67%) were positive to malaria parasite. On the other hand, Females recorded higher prevalence of 109 (59.24%) than Males 75 (40.76%). Healthcare facility C recorded the highest prevalence 49 (26.63%) followed by Healthcare facility B with 44 (23.91%) while Healthcare facility E recorded the least prevalence 20 (10.87%) (Table 1).
Prevalence of Typhoid Fever
A total of 143 (51.81%) patients were positive for typhoid fever; 87 (60.84%) males and 56 (39.16%) females. Healthcare facility B recorded the highest prevalence 34 (23.77%) followed by Healthcare facility D with 33 (23.08%) while Healthcare facility E recorded the least prevalence 22 (15.38%). However, there is no significant difference between the age groups (P > 0.05) (Table 2).
Co-infection of malaria and typhoid fever
Of the 276 (100%) patients tested for malaria parasite and typhoid fever, 132 (47.83%) were recorded as co-infection. Healthcare facility B recorded the highest prevalence 32 (24.24 %) followed by Healthcare facility D with 29 (21.97 %) while Healthcare facility C recorded the least prevalence 21 (15.91%). However, there was a significant difference in the age groups (P < 0.05) (Table 3, Figure 1).
Table 1: Prevalence of malaria parasite in relation to Healthcare facilities and Gender among sampled population in Kawo Metropolis.
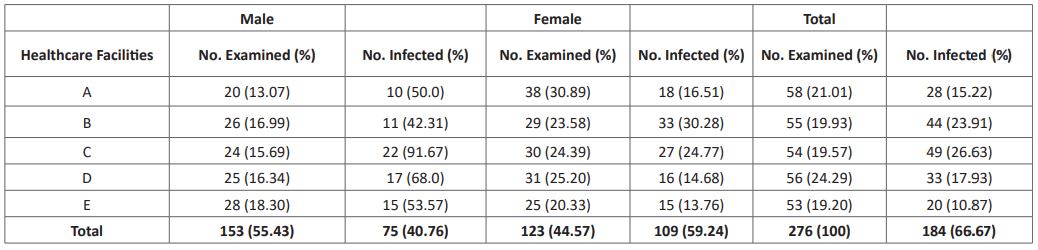
Table 2: Prevalence of Typhoid fever in relation to Healthcare facilities and Gender among sampled population in Kawo Metropolis
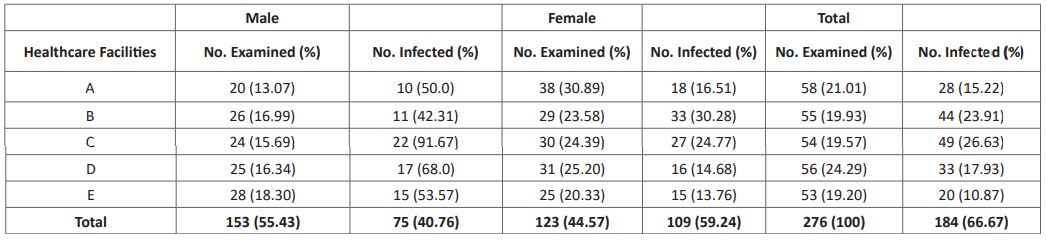
Table 3: Prevalence of Malaria Parasite, Typhoid Fever and their Co – infection in relation to Healthcare facilities in Kawo Metropolis.
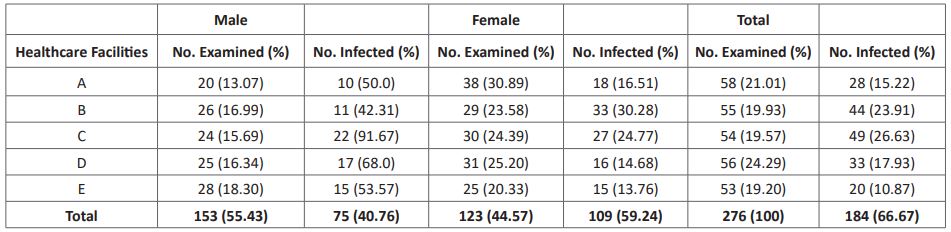
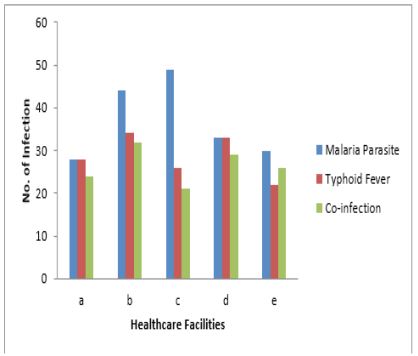
Figure 1: Malaria Parasite, Typhoid Fever and their Co – infection in relation to Healthcare facilities.
Discussion
Malaria and typhoid is still a major public health problem in tropics. The prevalence of malaria and typhoid co-infection is high in this study. Malaria and typhoid fever are tropical diseases where poverty mal-nutrition, poor sanitary status, poor personal hygiene, poor health facilities, poor social service and low level of education are among the factors that make tropical areas disease laden [28]. The findings reveal that a total percentage prevalence of 66.67% for malaria parasite was recorded among the sampled population of selected Healthcare facilities in Kawo Metropolis, Kaduna, Kaduna State. This is quite high. It shows that mosquitoes’ breeding, inoculation and transmission rate is very high, hence the study area is endemic for malaria. This high prevalence of malaria parasitaemia could be attributed to environmental factors such as altitude and rainfall and thick vegetations, which promote the intensity of mosquitoes breeding and transmission in Kawo Metropolis. Also, the case of Kawo metropolis is worsened due to their poor knowledge of methods for prevention/control of mosquitoes bites, hence malaria.
Females recorded higher positive cases of malaria infection (59.24%) more than males (40.76%), which is contrary to the report of [28] in Calabar and Akure respectively. However, this result corroborates the report of and [19] who recorded a higher prevalence among female students (56.9%) than male students (42.9%) in Abakaliki and Wukari, Nigeria. The high prevalence recorded among gender could be as a result of their different habits, level of exposure to mosquito bites and immunity developed against the parasite [29]. Typhoid fever prevalence rate was equally high (51.81%); 87 (60.84%) males and 56 (39.16%) females, but not statistically significant (P > 0.05). This prevalence rate is contrary to the report of[30] in Samaru, Zaria where females had slightly higher prevalence rate of typhoid fever (45.3%) than males (42.2%) but similar to the result obtained by [31] in Pakistan where the males had higher frequency of typhoid (51%) than females (49%). The high prevalence of typhoid fever could be attributed to the source of drinking water (such as water from uncovered well, contaminated sachet water) and indiscriminate defaecation in bushes around water sources which is a common practice among dwellers of Kawo metropolis which could have contributed to the high burden of typhoid fever recorded in this study [13].
The prevalence of malaria and typhoid co-infection (47.83%) in this study is higher than (10.33%) reported by [32] in Sokoto, (15.2%) by (Mbah and Agu, 2014) in Zaria and (28%) by (Orok et al., 2016) in Calabar. However, there was a significant difference between the numbers of individuals co-infected and those not co-infected (P < 0.05). Delay in treatment and treatment option could contribute to persistence and continued transmission of the co-infections.
In view of this significant difference and in order to roll out any case of malaria with mimicking symptoms, or the influence of anamnestic response the practical use of cultural methods for the diagnosis of typhoid fever should be emphasized in our clinical laboratories. This will also improve patient management by cutting down cost of treatment and eliminate other risks associated with misuse of antibiotics.
Conclusion
In view of this study, malaria and typhoid fever were prevalent in Kawo metropolis and still remain diseases of major public health importance. Comparably, both malaria parasitaemia and its co-infection with typhoid were more prevalent in females than in males of Kawo Metropolis. Typhoid fever was found to be more prevalent in males than in females. Since both are diseases of poverty, efforts should be made to improve on the living conditions of the people of Kawo Metropolis. Also, there should be public enlightenment of the preventive and control measures of the diseases. Both diseases have similar symptomatology; therefore, treatment should be based on adequate laboratory diagnosis. Also, personal hygiene is hereby encouraged among the populace.
Conflict of Interest: The authors declare no conflicts of interest of whatsoever.
Author’s Contribution
We declare that the both authors have made substantial contribution to the concept, acquisition and interpretation of data, draft of the article and its critical revision. Both authors approved the submission of the final version
References
- Ukaegbu CO, Nnachi AU, Mawak JD & Igwe CC. Incidence of concurrent malaria and typhoid fever infection in febrile patients in Jos, Plateau State Nigeria. International Journal of Scientific and Technology Research, 2014; 3(4): 157-161.
- Mbah JO, Njoku OO, Nnachi AU, Nnachi IA & Nwinyimagu AJ. Incidence of Antenatal Malaria Parasitaemia and the effect on the Haemoglobin Profile of Pregnant Women in Enugu East Local Government Area, Enugu, Nigeria. American Journal of Epidemiology and Infectious Disease, 2015; 3(5): 88-94.
- Iwuafor AA, Egwuatu CC, Nnachi AU, Akujobi CN, Ita IO, Ogban GI & Egwuatu TO. Malaria-related Febrile Illness and the use of Insecticide-Treated Nets (INTs) for Malaria Control Amongst Under-5 Year Old Children in Calabar, Nigeria. BMC Journal of Infectious Diseases, 2016; 16: 151.
- World Health Organization. World malaria report. Geneva: World Health Organization; 2011.
- World Health Organization. World malaria report, 2013, http://www.who.int/malaria/WMR0143. 2013.
- World Health Organization. World malaria report, 2014, http://www.who.int/malaria/WMR014. 2014.
- World Bank, World Development Indicator: Poverty rate at international poverty lines. Available online at: http//wdi.worldbank.org/table/28. accessed 24 November, 2014.
- WHO. Malaria prevention works, let’s close the gap. World Health Organization, Geneva, Switzerland. 2017.
- Ammah A, Nkuo-Akenji T, Ndip R & Deas JE. An update on concurrent malaria and typhoid fever and in Cameroon. Transactions of the Royal Society of Tropical Medicine and Hygiene, 2013;93: 127-129.
- WHO (2018). World Malaria Report. Federal Republic of Ethiopia Ministry of Health, National Guide Lines, (3rd edition).
- WHO (2016). Malaria prevention works, let’s close the gap. World Health Organization, Geneva, Switzerland.
- Simon-Oke IA. Prevalence of Malaria parasite among asymptomatic and symptomatic students of Federal University of Technology, Akure, Ondo-State. British Journal of Research, 2017; 4: 2-4.
- Mbuh FA, Galadima M & Ogbadu L. Rate of co-infection with malaria parasites and Salmonella typhii Zaria, Kaduna State, Nigeria. Annual African Medical Report, 2013; 2: 64-67.
- Orok DA, Ibor UA, Oyama IO, Edisua ED & Efeffiom EE. Prevalence of malaria and typhoid fever co-infection among febrile patients attending College of Health Technology Medical Centre in Calabar, Cross River State, Nigeria. International Journal of Current Microbiology and Applied Science, 2016; 5: 825-835.
- Wain J, Hendriksen RS, Mikoleit ML, Keddy KH & Ochiai RL. Typhoid Fever. Lancet, 2015; 85(9973): 1136-45.
- Crump JA and Mintz ED. Global trend in typhoid and paratyphoid fever. Clinical infectious. An official publication of the infectious Diseases. Society of America, 2010; 50(2): 241-6.
- Buckle, GC, Walker CL & Black RE. Typhoid fever and paratyphoid: systematic review to estimate global morbidity and mortality for 2010. Journal of Global Health, 2, 1. Article I.D 010401, 2012. 2010.
- Crump JA, Luby SP & Mintz ED. The burden of Typhoid fever. Bulletin of the World Health Organization, 2004; 82(5): 34b-53.
- Muhammad S, Muhammad Z, Riaz A, Muhammad R & Mudassar S. Co-infection of malaria and typhoid in district Dir (Lower) Khyber Pakhtunkhwa, Pakistan. Journal of Entomology and Zoology Studies, 2017; 5: 912-914.
- Muyembe-tamfum JJ, Veyi J, Kaswa M, Lunguya O, Verhaegen J & Boelaert M. An outbreak of peritonitis caused by multi-resistant Salmonella typhi in Kinshasa. Democratic Republic of Congo. Travel Medical Infections Disease, 2009; 7: 40-3.
- Baddam R, Narender K, Kwai-Ln T, Soo-Tein N, Cindy SJ, Kein-pong Y, et al. Genetic fine structure of a Salmonella enteric serovar typhi strain associated with 2005 outbreak of typoid in Kelantan Malaysia. Journal of Bacteriology, 2012; 194(13): 3565-3566.
- Keong BCM and Sulaiman W. Typhoid and malaria co-infection —an interesting finding in the investigation of a tropical fever. Malaysian Journal of Medical Sciences, 2016; 13: 74–5.
- Ammah A, Nkuo-Akenji T & Ndip R. An update on concurrent malaria and typhoid fever and in Cameroon. Transactions of the Royal Society of Tropical Medicine and Hygiene, 1999: 93:127-129.
- Kanjilal SD, Dutta A, Mondal RK & Chakravorti S. Uncomplicated falciparum malaria complicated by Salmonella septicaemia: cause not coincidence. Journal of the Indian Medical Association, 2016; 104: 646–8.
- Ohanu, ME, Mbah AU, Okonkwo PO & Nwagbo FS. Interference by malaria in the diagnosis of typhoid using Widal test alone. West African Journal of Medicine, 2003; 22: 250-252.
- Uneke CJ. Concurrent malaria and typhoid fever in the tropics: the diagnostic challenges and public health implications. Journal of Vector Borne Diseases, 2008; 45: 133–142.
- Ochei JO and Kolhatkar AA. Medical Laboratory Science: Theory and Practice”, Tata McGraw-Hill, New Delhi, India, 2010; 692-693, 962.
- Obimakinde ET and Simon-Oke IA. The prevalence of malaria infection among patients attending the Health Centre of the Federal University of Technology Akure, Nigeria. International Journal of Tropical Disease and Health, 2017; 27: 1-7.
- Morde RM and Borke ME. The prevalence of malaria in Edo State, Nigeria. Nigerian Journal of Parasitology, 2013; 34: 41- 46.
- Mbah CE and Agu B. Prevalence of malaria and typhoid co-infection among patients in some hospitals in Samaru, Zaria. Annals of Bioanthropology, 2014; 2: 43-48.
- Asma WQ, Zaib-Ullah K, Luqman K, Abu M & Rashid M. Prevalence of malaria, typhoid and co-infection in district DIR (Lower) Pakistan. Bioscience Journal, 2019; 35: 317-325.
- Alhassan HM. Co-infection profile of Salmonella typhi and Malaria parasite in Sokoto-Nigeria. Global Journal of Science, Engineering and Technology, 2012; 201: 13-20.

