Case Report - Volume 2 - Issue 5
Atypical Presentation of Infective Endocarditis in a Young Man without Risk Factors: A Case Report
Jorge Luiz de Carvalho Mello1,*; Eliton Edimilson do Couto2; Alyne Couto Carvalho da Fonseca Machado2;Gustavo Henrique Reis Mariano2; Sebastião Jupiaçara Guimarães3
1Associate Professor, Department of Medical Clinic, University of Vale do Sapucaí, Pouso Alegre, Minas Gerais, Brazil.
2Medical Student, University of Vale do Sapucaí, Pouso Alegre, Minas Gerais, Brazil.
3Head of the Department of Clinical Medicine, University of Vale do Sapucaí, Pouso Alegre, Minas Gerais, Brazil.
Received Date : Sep 01, 2022
Accepted Date : Oct 11, 2022
Published Date: Oct 29, 2022
Copyright:© Jorge Luiz de Carvalho
Mello 2022
*Corresponding Author : Jorge Luiz de Carvalho Mello, Department of Applied Health Sciences, UNIVAS Av. Prefeito Tuany Toledo, 470. CEP 37554-210 Pouso Alegre, MG, Brazil. Tel: 55-35-34499231.
Email: jorgeluis_melo@yahoo.com.br
DOI: Doi.org/10.55920/2771-019X/1277
Abstract
Infective endocarditis is a disease caused by the adherence of infectious agents to the endocardial surface, resulting in inflammation and damage, especially to the heart valves. Endocarditis may be diagnosed in up to 5% of patients with prolonged febrile syndrome. The incidence of endocarditis affecting the right heart chambers ranges from 5% to 10% with predominant involvement of the tricuspid valve. Pulmonary valve involvement is rare and usually associated with immunosuppressive conditions or structurally abnormal hearts. Pulmonary valve endocarditis may present atypically with recurrent respiratory symptoms, so that echocardiography should be considered to assess the presence of right heart lesions, which may be a challenge for suspicion and diagnosis, especially in patients without risk factors. In this study, the authors report a case of isolated infective endocarditis in the pulmonary valve due to Staphylococcus aureus in a young man with recurrent pneumonia episodes and without traditional risk factors. Although technological advances contribute to the diagnosis of complex cases, the clinical approach was the best way to determine the appropriate tests and examinations, and for choosing or developing interventions. Despite the availability of resources and diagnostic tools, many diseases associated with high morbidity and mortality may be misdiagnosed and mistreated, including infective endocarditis. A comprehensive patient assessment is essential for the correct diagnosis, as many signs and symptoms are common to different diseases.
Keywords: Endocarditis; Heart valves; Pulmonary valve.
Introduction
Infective endocarditis is caused by the adherence of infectious agents to the endocardial surface, resulting in inflammation and damage, especially to the heart valves. Acute infective endocarditis is usually characterized by the presence of a virulent pathogen, such as Staphylococcus aureus, with involvement of a normal heart valve, commonly resulting in a typical clinical presentation and early complications, with signs and symptoms usually reported in less than two weeks of onset. Subacute infective endocarditis is frequently characterized by the presence of a less virulent pathogen, such as Streptococcus viridans or Staphylococcus epidermidis, with the involvement of an abnormal heart valve and symptoms reported after two weeks from the onset [1].
Infective endocarditis often produces vegetation, identified by echocardiography as a mass of echogenic material adhered to the endocardial surface, showing different mobility from those of the surface. Vegetations tend to grow in the heart valve leaflets and on the ring of mechanical prostheses in the direction of the regurgitant jet [1].The mitral and aortic valves are affected in about 40% and 34% of cases, respectively [2]. The involvement of the tricuspid and pulmonary valves in endocarditis is more frequently observed among intravenous drug users and patients with central venous access catheters. Pulmonary valve involvement is rare, affecting less than 2% of patients with infective endocarditis [2]. The authors report a case of pulmonary valve endocarditis in a young man without traditional risk factors.
Case report
An 18-year-old man reported having intermittent fever and chills in the last 50 days, with axillary temperature ranging from 39°C to 41°C, especially during the afternoon and night periods, which could be reduced with antipyretic drugs. The patient complained of asthenia and cough productive of yellowish sputum, and reported three episodes of pneumonia during the 50-day period. He claimed to be afebrile both during the last in-hospital treatment and 10 days following discharge, after which he experienced fever recurrence. Then, he sought treatment at the Samuel Libânio General Hospital (Brazil), where he was hospitalized for investigation.
The medical history revealed that the patient had undergone septoplasty for deviated septum and tonsillectomy as a child, which required blood transfusion, but without other complication. The patient was a former smoker, who had smoked for six months, and denied the use of any illicit injectable drug. He had no history of upper respiratory tract infection, dental procedures, respiratory-related pain, or changes in the gastrointestinal or urinary tracts.
The patient was slightly dehydrated, but in good general condition at hospital admission. His axillary temperature was 38ºC, but without other changes; no palpable lymph nodes or signs of meningeal irritation were detected; the abdomen and respiratory, cardiovascular, and locomotor systems showed no relevant changes. Laboratory tests were requested and the results were as follows: hemoglobin, 12.1 g/dl; total leukocytes, 39,300/mm3 with 20% rods; C-reactive protein (CRP), 73 mg/dl; a negative HIV-test, and smear-negative for acid-alcohol-fast-bacilli (AAFB). Blood culture tested positive for methicillin‐sensitive Staphylococcus aureus. On the fifth day after admission, the patient presented diastolic murmur in pulmonary focus detected by changes in cardiac auscultation. Thus, the patient was assessed for infective endocarditis by transthoracic Doppler echocardiography. The echocardiogram revealed evidences of vegetation on the pulmonary valve and signs of valve insufficiency (Figure 1), leading to the hypothesis of infective endocarditis, which was confirmed by the modified Duke criteria [3]. The patient met two major and one minor criteria of this instrument, thus confirming the diagnosis of infective endocarditis in the pulmonary valve due to Staphylococcus aureus.
Computed tomography of the chest was also performed and showed small peripheral consolidations with bronchiectasis, and sparse bilateral areas containing frosted glass opacification in the right lower lobe. The patient was then treated with oxacillin, 2 g every 4 hours, given intravenously for 4 weeks, resulting in satisfactory progress, then discharged from hospital, and followed-up at the outpatient clinic of the same hospital.
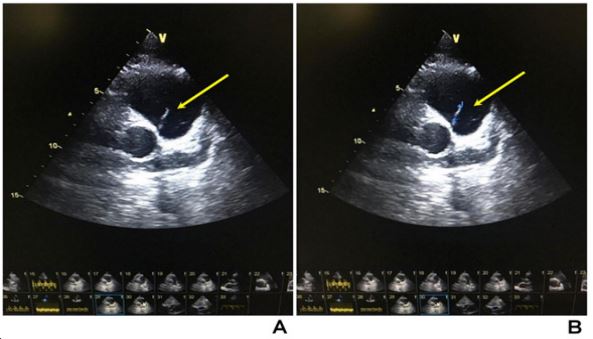
Figure 1: Echocardiograms showing (A) the presence of a 1.1 cm mass attached to the ventricular surface of the pulmonary valve associated with mild reflux; and (B) an image suggestive of pulmonary valve vegetation, which is marked in blue. Other cardiac structures were normal.
Discussion
Endocarditis may be diagnosed in up to 5% of patients with prolonged febrile syndrome [2]. The incidence of endocarditis in the right heart chambers ranges from 5% to 10%, with predominant involvement of the tricuspid valve. Involvement of the pulmonary valve is rare, possibly due to low oxygen content of the venous blood, and low-pressure gradients or differences in endothelial coverage and vascularization of the right heart.
Staphylococcus spp. is the most common responsible pathogen for infective endocarditis. The main risk factors include underlying valvular or congenital heart disease, intravenous drug use, alcohol consumption, dialysis treatment, liver cirrhosis, and use of pacemakers [3-5]. Prior studies have found that right-sided endocarditis is caused by Streptococcus viridans in about 55% to 65% of cases among non-drug users, whereas Staphylococcus aureus is prevalent among drug users. Isolated pulmonary valve endocarditis in patients with neither pulmonary lesions nor traditional risk factors is difficult to diagnose, [2] with echocardiography playing an important role in the propaedeutic investigation [6-8]. In this case, the presence of vegetation on the pulmonary valve was detected on echocardiogram. The diagnosis was confirmed using the modified Duke criteria, which is an instrument widely used for the diagnosis of infective endocarditis [3].
According to this instrument, diagnosis of definitive infective endocarditis requires two major criteria, or one major and three minor criteria, whereas the diagnosis of probable infective endocarditis requires one major and one minor criterion, or three minor criteria (Chart 1) [3]. A comprehensive patient assessment, combining clinical history, physical examination, laboratory tests and imaging studies is essential to reach the correct diagnosis, as many signs and symptoms are common to different diseases [9]. Pulmonary valve endocarditis may present atypically with recurrent respiratory symptoms [10]. Our findings indicated that the pneumonia episodes reported by the patient were probably caused by septic embolism to the lung and pulmonary infections, which delayed diagnosis of infective endocarditis.
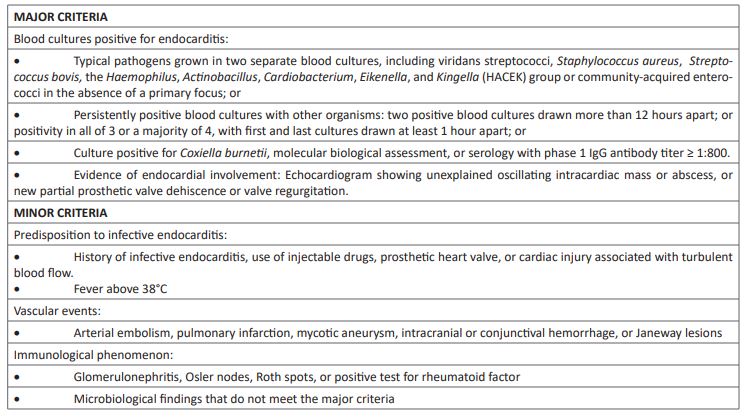
Chart 1: Modified Duke criteria for the diagnosis of infective endocarditis.
Conclusion
This study reported a case of right heart endocarditis with pulmonary valve involvement with atypical recurrent pneumonia episodes. Echocardiography was fundamental for the detection of right heart lesions, which may be a challenge to suspicion and diagnosis. Recurrent pneumonia episodes should be included in the list of differential diagnoses for right heart endocarditis.
Learning Points
- Right heart endocarditis is rare, especially with involvement of the pulmonary valve.
- Pulmonary valve endocarditis may present atypically with recurrent respiratory symptoms.
- Echocardiography should be considered for the assessment of right heart lesions, which may be a challenge to suspicion and diagnosis.
- Recurrent pneumonia should be included in the list of differential diagnoses for right heart endocarditis.
Declarations of interest: none
Role of the funding source: No outside funding was received.
Ethics: The patient signed the informed consent for the procedures and for the use of clinical data and photographic records for scientific purposes and publication. Patient anonymity was assured. This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki of the World Medical Association, and its subsequent amendments.
References
- Alves Rezende LG, Geleilete TJ, Carvalho MT, Rezende TV, Castro NA, Barcelos BC, et al. Infectious tricuspid valve endocarditis with septic pulmonary emboli: case report. Arch Health Invest. 2014; 3(2): 16-20.
- Grativvol KM, Grativvol PS, Gama JD, Rosa FA, Grativvol RS. Pulmonary valve endocarditis in subjects without classical risk factors for involvement of right heart. Rev Bras Ecocardiogr Imagem Cardiovasc 2012; 25: 116-8.
- Salgado AA, Lamas CC, Buoy MN. Infective endocarditis: what has changed in the last decade? Rev HUPE 2013; 12: 100-9. https://doi.org/10.12957/rhupe.2013.7088.
- Della Giustina R, Marchi MF, Fiamoncini MM, Mazon EZ, Bussoletto MP, Fiamoncini A. Trivalvular endocarditis: a rare multivalvular condition. Arq Bras Cardiol: Imagem Cardiovasc 2019; 32: 79-81. https://doi.org/10.5935/2318-8219.20190016.
- Ranjith MP, Rajesh KF, Rajesh G, Haridasan V, Bastian C, Sajeev CG, et al. Isolated pulmonary valve endocarditis: A case report and review of literature. J Cardiol Cases 2013; 8: 161-3. https://doi.org/10.1016/j.jccase.2013.07.007.
- Nascimento BR, Coelho TO, Costa Filho LR, Pinto Filho MM, Cota VE, Bicalho RC, et al. Right-side infective endocarditis: discrepancy between clinical and echocardiographic evolution: case report. Rev Soc Bras Med Trop. 2009; 42: 587-90. https://doi.org/10.1590/s0037-86822009000500020.
- Leme Neto AC, Adam EP, Carvalho G. Infective endocarditis: definition diagnosis and treatment by echocardiography. Rev Bras Ecocardiogr Imagem Cardiovasc 2013; 26: 50-1.
- Barbosa MM. [Infective endocarditis: evolving clinical profile]. Arq Bras Cardiol 2004; 83: 189-90.
- Machado FCA, Ferreira MAF. Infective endocarditis profile in a reference hospital from 2003 to 2009. Rev Bras Odontol 2013; 70: 8-11.
- Moreira D, Correia E, Rodrigues B, Santos L, Capelo J, Abreu L, et al. Isolated pulmonary valve endocarditis in a normal heart. Rev Port Cardiol 2012; 31: 615-7. https://doi.org/10.1016/j.repc.2012.01.019.

