Case Report - Volume 2 - Issue 6
A Case Report of Perimyocarditis as a Rare Complication of Campylobacteriosis
Ahmad Behzadpour 1*; Dave Patel 2; Xolani Mdluli 2; and Arya Khoshniyati 3
1American University of the Caribbean, School of Medicine, Coral Gables, FL, USA.
2Department of Infectious Disease Eisenhower Health, Rancho Mirage, CA, USA.
3Department of Internal Medicine, Eisenhower Health, Rancho Mirage, CA, USA.
Received Date : Sep 06, 2022
Accepted Date : Oct 15, 2022
Published Date: Nov 02, 2022
Copyright:© Ahmad Behzadpour 2022
*Corresponding Author : American University of the Caribbean, School of Medicine, Coral Gables, FL, USA.Tel: 312-532-1098.
Email: djr.min@gmail.com
DOI: Doi.org/10.55920/2771-019X/1281
Abstract
Campylobacter species is one of the most common infections that cause gastroenteritis in developed countries. Although most Campylobacter infections are self-limited, cases can be complicated by extraintestinal presentation, such as myocarditis, pericarditis, or perimyocarditis. We report herein a case of perimyocarditis complicating gastroenteritis in a 24-yearold male. The patient presented with abdominal pain, diarrhea, and dehydration over a couple of days, progressively worsening with substernal chest pain and dyspnea. Troponins were elevated, and ECG showed diffuse concave ST elevation and PR segment depression. Based on the clinical signs and symptoms, the diagnosis of perimyocarditis was made, and he was treated accordingly with a favorable outcome.
Keywords: Campylobacter; Gastroenteritis; Enterocolitis; Diarrhea; Perimyocarditis; Myocarditis; Pericarditis.
Abbreviations: NAGMA: Non-Anion Gap Metabolic Acidosis; ECG: Echocardiography; WBC: White Blood Cells; CRP: C-Reactive protein; ESR: Estimated Sedimentation Rate; CT: Computed Tomography; EF: Ejection Fraction.
Case Report
A 24-year-old male with no significant past medical history presented to the emergency department with four days of diarrhea which progressed to chest pain. The patient started to have loose stool twice a day, progressively worsening to diarrhea that started from yellow color to red, and then green. The patient denied any foul smell but reported generalized abdominal pain localizing to the periumbilical region characterizing it as crampy pain. He also reported a dull non-radiating pleuritic chest pain localized to the substernal area. Upon arrival, he was found to have tachycardia of 141 bpm, normotensive blood pressure of 119/77 mmHg, and a respiration rate of 20 with 95% O2 saturation on room air. He was severely volume depleted with the dry oral mucosa, decreased skin turgor, and capillary refill time. Initial laboratory work-up revealed hypokalemia of 3.4 mmol/L, mild NAGMA, hyponatremia of 131 mmol/L, WBC 14.1 K/uL, CRP 12.6 mg/L, ESR 31 mm/hr, and troponin of 35.8 pg/mL that increased to 1350 pg/mL. The troponin started down-trending later. ECG revealed sinus tachycardia, diffused concave up ST elevation, and PR segment depression associated with acute pericarditis (Figure 1). GI panel revealed campylobacter jejuni, and leukocytes were found in his stool sample. CT scan of the abdomen revealed pancolitis with diffuse colonic wall thickening and edema (Figure 2). The chest CT also illustrated a minimal pericardial effusion (Figure 3), and a transthoracic echocardiogram confirmed the small circumferential pericardial effusion with thickening of the posterior parietal pericardium and EF of 50-55%. The diagnosis of perimyocarditis was made. The treatment was initiated with oral azithromycin 500 mg daily for seven days, ibuprofen 600 mg twice a day, and oral methylprednisolone for one week.

Figure 1. ECG findings revealed concave up ST elevation and PR segment depression that are common in the setting of acute pericarditis.
Follow Up
On follow-up with his primary care physician, he reported an absence of chest pain and diarrhea. The CRP level had normalized.
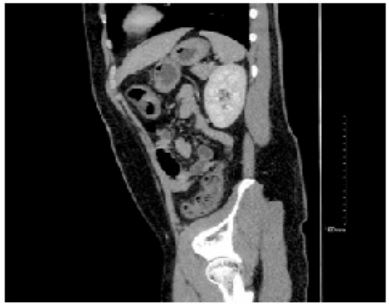
Figure 2: Abdominal CT revealed pancolitis with diffuse colonic wall thickening and edema.
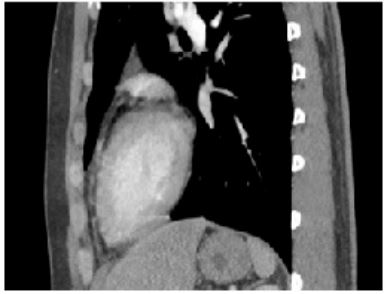
Figure 3: Sagittal view of the CT scan from the thoracic cavity demonstrating minimal pericardial effusion.
Discussion
The most common cause of diarrhea is infectious etiologies. While the most common infection is viral gastroenteritis, bacteria such as Campylobacter, Salmonella, and Shigella are the most common cause of acute diarrhea [1]. One of the leading pathogens that cause gastroenteritis in developed countries is the Campylobacter species. Campylobacteriosis has early and late complications that can be deleterious. For instant, urticaria, erythema nodosum, cholecystitis, peritonitis, and abdominal aortic septic pseudoaneurysm. The late course of the disease presents as reactive arthritis and Guillain-Barré syndrome. Campylobacter infection may progress to bacteremia in immunocompetent and immunocompromised individuals (2). Pericarditis and myocarditis can be associated with a late complication of campylobacter gastroenteritis, as demonstrated in our patient [3]. The development of cardiac manifestations presents most often involves young adults or teenagers. As in most gastroenteritis illnesses, symptoms begin with fevers, abdominal pain, and diarrhea, after which symptoms of concurrent chest pain, discomfort, or tightness ensue within 48-72 hours [5]. Therefore, a reported history of chest discomfort following bouts of diarrhea should prompt physicians to include Campylobacteriosis in their differential [4]. The pathophysiology of perimyocarditis secondary to Campylobacter gastroenteritis is not fully understood. Still, the combination of the number of organisms consumed, the virulence of the infecting strain, and the host immunity are all crucial factors in the patient’s clinical presentation. Several factors are beginning to be just understood, and two proposed models have been reviewed in the literature. One model suggested that the pathogen or toxin-induced may be responsible for the acute presentation of the carditis within 48-72 hours. The alternative model offered that the immunological response such as systemic circulation of immune complexes or cytotoxic T Cell attack presents with the later presentation of the cardiac embodiments [6-9].
Regardless of the proposed pathogenies of the disease, almost all the immunocompetent patients with gastroenteritis secondary due to campylobacter infection in the literature have not been reported to experience bacteremia with the disease. However, this doesn’t exclude the likelihood of the pathogen harboring transient bacteremia as its mechanism of action [10]. Lastly, because most Campylobacter infections are self-limited and have limited efficacy of antimicrobials, antibiotic therapy is only recommended for individuals with severe disease. For instance, patients with bloody stools, a high temperature, an extraintestinal infection such as myocarditis, pericarditis or perimyocarditis, increasing or recurrent symptoms, or symptoms that persist for more than a week are considered to have a severe illness [11].
Conclusion
Gastroenteritis due to Campylobacter infection can be mild, self-limited, and often treated with a supportive case. However, the physicians need to recognize progression to cardiac manifestations of Campylobacteriosis, such as myocarditis and pericarditis, as severe manifestations as treatment varies. Meanwhile, the exact pathogenesis of the disease is still under review, and physicians’ awareness of the progression of the disease will allow a timely, focused treatment.
Conflicts of Interest: None.
Funding Sources: None.
References
- Dryden MS, Gabb RJ, Wright SK. Empirical treatment of severe acute community-acquired gastroenteritis with ciprofloxacin. Clin Infect Dis. 1996 Jun; 22(6): 1019-25. [PMID: 8783703 DOI: 10.1093/clinids/22.6.1019].
- Spapen J, Hermans H, Rosseel M, Buysschaert I. Campylobacter jejuni-related cardiomyopathy: Unknown entity or yet underreported? Int J Cardiol. 2015 Nov 1; 198: 24-5. [PMID: 26149333 DOI: 10.1016/j.ijcard.2015.06.110] [Epub 2015 Jul 3]
- Hannu T, Mattila L, Rautelin H, Siitonen A, Leirisalo-Repo M. Three cases of cardiac complications associated with Campylobacter jejuni infection and review of the literature. Eur J Clin Microbiol Infect Dis. 2005 Sep; 24(9): 619-22. [PMID: 16167138 DOI: 10.1007/s10096-005-0001-2].
- Lai T, Yadav R, Schrale R. Mimicking myocardial infarction: localized ST-segment elevation in Campylobacter jejuni myopericarditis. Intern Med J. 2009 Jun; 39(6): 422-3. [PMID: 19580626 DOI: 10.1111/j.1445-5994.2009.01930.x].
- Hessulf F, Ljungberg J, Johansson PA, Lindgren M, Engdahl J. Campylobacter jejuni-associated perimyocarditis: two case reports and review of the literature. BMC Infect Dis. 2016 Jun 14; 16: 289. [PMID: 27297408; PMCID: PMC4907281 DOI: 10.1186/s12879-016-1635-7].
- Florkowski CM, Ikram RB, Crozier IM, Ikram H, Berry ME. Campylobacter jejuni myocarditis. Clin Cardiol. 1984 Oct; 7(10): 558-9. [PMID: 6488601 DOI: 10.1002/clc.4960071008].
- Uzoigwe C. Campylobacter infections of the pericardium and myocardium. Clin Microbiol Infect. 2005 Apr; 11(4): 253-5. [PMID: 15760422 DOI: 10.1111/j.1469-0691.2004.01028.x].
- Pena LA, Fishbein MC. Fatal myocarditis related to Campylobacter jejuni infection: a case report. Cardiovasc Pathol. 2007 Mar-Apr; 16(2): 119-21. [PMID: 17317547 DOI: 10.1016/j.carpath.2006.09.007].
- Alzand BS, Ilhan M, Heesen WF, Meeder JG. Campylobacter jejuni: enterocolitis and myopericarditis. Int J Cardiol. 2010 Sep 24; 144(1): e14-6. [PMID: 19168238 DOI: 10.1016/j.ijcard.2008.12.101] [Epub 2009 Jan 26].
- Skirrow MB, Jones DM, Sutcliffe E, Benjamin J. Campylobacter bacteraemia in England and Wales, 1981-91. Epidemiol Infect. 1993 Jun; 110(3): 567-73. [PMID: 8519321; PMCID: PMC2272297 DOI: 10.1017/s0950268800050986].
- Ruiz-Palacios GM. The health burden of Campylobacter infection and the impact of antimicrobial resistance: playing chicken. Clin Infect Dis. 2007 Mar 1; 44(5): 701-3. [PMID: 17278063 DOI: 10.1086/509936] [Epub 2007 Jan 25].

