Review Article - Volume 2 - Issue 6
Chronicling Subtle Nuances of Childhood Apraxia of Speech (CAS) through Exclusive Non- standardized tool
Nayana Narayanan* ; Fida Jasmine; Nasla TK
Assistant Professor, Department of Audiology and Speech Language Pathology, AWH Special College, Kerala University of Health Sciences, India.
Received Date : Sep 28, 2022
Accepted Date : Oct 22, 2022
Published Date: Nov 08, 2022
Copyright:© Nayana Narayanan 2022
*Corresponding Author : Nayana Narayanan, Assistant Professor, Department of Audiology and Speech Language Pathology, AWH Special College, Kerala University of Health Sciences, India.
Email: nayananarayanan2989@gmail.com
DOI: Doi.org/10.55920/2771-019X/1287
Abstract
Childhood Apraxia of Speech is one of the most interesting motor speech disorders. Child with CAS will not be able to produce speech voluntarily. Due to its subtle nature CAS is either under-diagnosed or over-diagnosed in general. Another challenge faced in practice is the barrier of language as most of the standardized test uses English language based questionnaire format. Henceforth, we developed a tool to qualitatively assess various aspects of CAS.
Introduction
Childhood Apraxia of Speech (CAS) is a very intriguing yet complicated motor speech disorder. It is a disorder that stems from neurological insult to the developing brain due to causes ranging from pre, peri and post natal complications. The salient features of CAS include inability to voluntarily produce speech in the absence of any evident weakness, sensory deficits or lack of language skills. Based on a number of studies, it is clear that the fundamental problem with CAS is a lack in planning and programming, which prevents the affected child from speaking at will [1,2,3,4,5]. At core, in CAS, the voluntary speech differs significantly from involuntary speech [6,7]. Speech in CAS follows a definite pattern. The child will have deficits predominantly in articulation and prosody. ASHA reports three major diagnostic markers in the speech of children with CAS. These include (a) inconsistent errors on consonants and vowels in repeated productions of syllables or words, (b) lengthened and disrupted coarticulatory transitions between sounds and syllables, and (c) inappropriate prosody, especially in the realization of lexical or phrasal stress [emphasis added]”.The articulatory errors detected are highly inconsistent in nature [3,7,8]. Evidently, there exists a visible difference in articulation during voluntary and involuntary speech [3,9]. According to the survey by Shakibayi et.al the predominant articulatory errors reported in CAS other than their hallmark inconsistencies include oromotor difficulties, groping, polysyllabic word errors, sequencing problem and general unintelligibility. Prosody is another aspect of speech that also showed evident abnormalities. The prosodic errors reported in CAS ranges from increased duration in between speech segments and decreased variations in fundamental frequency in different intonation patterns. There are also reports of reduced or erroneous lexical stress placement [10,11] and disrupted rhythms as evidenced by the timing errors [12].
The features of CAS are intriguing yet confusing due to its subtle nature. The chief reason for this is being the negative description of the disorder. i.e, most of the definitions of CAS are given in terms of what should not be present as opposed to what to look for. Another reason is that CAS is categorized under many umbrella disorders. For instance, on one hand ASHA classifies CAS under speech sound disorder whereas on other hand DSM classifies it under development coordination disorder. Yet another school of thought considers CAS as a sensory processing disorder [13]. The definitions are also given accordingly. These controversies make it difficult to define the features of CAS. The lack of crispness in description of CAS leads to many challenges in clinical practice. Due to it’s the concealed nature, in many instances CAS is either under diagnosed or over diagnosed. Further, CAS co-occurs with other disorders with overlapping features. For instance, clinically a child with CAS shares many feature akin to general speech language disorders like speech sound disorders, Autism and even to some extent cerebral palsy. So when these disorders co-exist it becomes practically impossible to differentially diagnose CAS from other co-existing conditions. Yet another challenge faced by diagnostician is the language barrier. All the standardized tests and checklist developed use English language as medium. Hence, it is ineffective for a non-english speaker.
Need for the study
Assessing CAS is a cumbersome process as due to all of the above mentioned factors. A qualification of the features of CAS makes in more confusing rather than resolving the issues. Therefore, to bring clarity for diagnosis we put forth the idea of a qualitative tool. This tool uses descriptive data to record the features of CAS.
Method
About the tool
The tool possesses checklist like format with eleven subsets and a provision for differential diagnosis. The eleven subsets include (i) History, (ii) Motor functions, (iii) Sensory evaluation, (iv) Psycho social evaluation, (v) Speech analysis, (vi) Speech analysis, (v) Language evaluation, (vi) Prosodic aspects (vii) Other Speech subsystem evaluation, (ix) Inconsistency and variability, (x) other observation, (xi) Testing for non-verbal apraxia and finally (xii) differential diagnosis. The subsets were isolated after in depth research. We reviewed nearly fifty articles published regarding CAS from the last decade through open access platforms including Google scholar, Academia, Pubmed, Sciencedirect, Core and Base. Additionally, Information was gathered from professionals working in the field of speech-language pathology using Delphi method and Interview. The efficacy of these materials were discussed and debated in a focus group comprised of four academics, ten undergraduate, and five postgraduate students in the field of Speech Language Pathology. The conclusive points from this focus group discussion were given to three speech language pathologist with minimum ten year of experience working in the area of CAS to fact check. Each subset had numerous questions under them that have to be answered in a descriptive format. No discrete scoring was carried out. The tool is attached in appendix 1.
Administration of the tool
The tool was administered in five children suspected of CAS. The results were tabulated in detail. As it was in a descriptive format no statistical analysis was carried out.
Results
(Table 1) describes the results of administration of the checklist in suspected CAS cases. The results of each case in described separately across each section. The table provides a comprehensive data regarding the cases.
Table 1:Description of CAS features from the developed tool for the five suspected CAS cases.
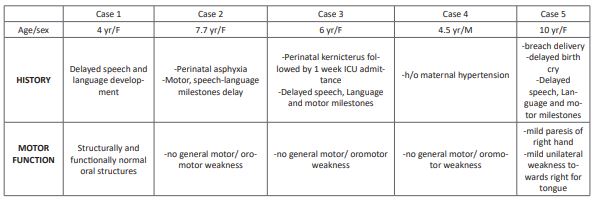
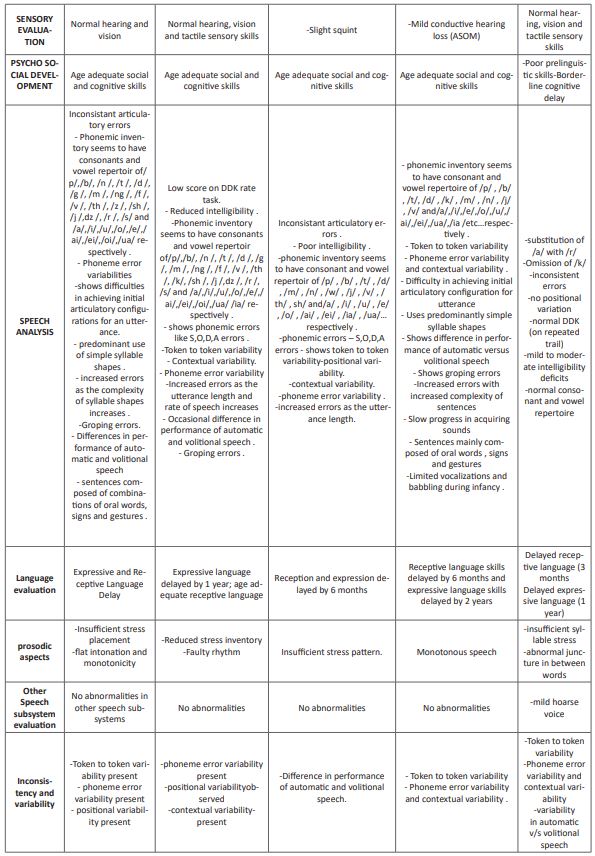
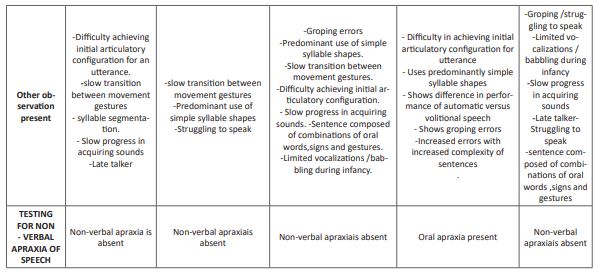
Note:
The table represents the Results of Administration of CAS Tool in five suspected CAS cases. Column 1 represents the sections of tool. Each row records a separate case. Each individual cell describes the features recorded in that particular case across the respective section. yr-years; F-Female; M-Male.
Discussion
(Table 1) gives a clear account of the results of administering the tool in suspected CAS cases. Each subsection is dedicated to outline the various aspects that point the diagnostician towards CAS. The first section documents any potential neural involvement, while the second, third and fourth sections aid in understanding the child's overall motor, sensory and psychosocial development The results we were able to gather in the five suspected CAS cases clearly indicate the presence of neuronal injury.All cases had normal motor and psychosocial abilities, with the exception of case 5, in which there was comorbid dysarthria.
Results of speech evaluation concluded that except in case 5, rest all cases the children exclusively showed deficits in articulation and prosody. There were also noteworthy variability and inconsistencies in the errors thus strongly suggesting the presence of CAS. These results strongly support the presence of CAS in the selected cases.
Furthermore, the tool was also successful in isolating CAS from other disorders sharing similar aspects. For instance, in all of the five cases mentioned in the table there was definite language delay. However, the tool was able to differentiate language related disabilities from the apraxic component through series of well-formed questions. The provision for differential diagnosis enabled the diagnostician to charter the features of each concomitant disorder separately. The separate section delineating the consistency and variability of errors enabled the diagnostician to confirm the probability of CAS based of its exact nature i.e. unpredictable error pattern. Finally, the diagnostician might record the existence of any non-verbal apraxias that might co-occur with CAS in the last section. Only case 4 in our subjects exhibited mild oral apraxia.
The major limitation of our tool is that, it doesn’t give a quantitative data. But practical experience from professional reported that quantitate value lacked personalization. For instance, the scoring in itself will not allow us to understand the finer deficits in the child. Instead our checklist allows us to record the subtle features and characteristics to the data which enables the interventionist to move with it. However, more information can be added to the tool to increase its sensitivity.
Summary and conclusion
To put comprehensively, the tool is a very good mean to outline the subtle aspects of CAS as it compiles many areas exclusive to CAS and bypasses the hurdle of using language as a mean to evaluate the child.As unorthodox our method us, we can strongly argue that the focus of making such a tool is not for the purpose of diagnosing CAS but rather to work as a basis for intervention. Our tool provides information on the core deficits of these children. When put together these kernels can light strong fire that can aid the process of intervention in such children, thereby fanning the rate of prognosis in them.
Ethical Consideration
The study followed the ethical rules and regulation of Kerala University of Health Sciences and was accepted by ethical committee of AWH Special College, Kozhikode. The client was informed and consent was obtained. The study was conducted by maintain proper respect and anonymity towards the client.
Acknowledgement
We wish to thank our Principal Dr P K Abdul Kader and our Head of the Department Mrs. Girija P C for allowing us to conduct this study. We also appreciate the support of staff and students of AWH Special College that helped us to achieve the completion of this study.
Conflict of Interest: There is no conflict of interest between the authors and the authors as well the client.
References
- Shriberg LD, Aram DM & Kwiatkowski J. Developmental apraxia of speech: I. Descriptive and theoretical perspectives. Journal of Speech, Language, Hearing Research. 1997; 40(2): 273-285.
- Davis BL, Jakielski KJ & Marquardt TP. Developmental apraxia of speech: Determiners of differential diagnosis. Clinical linguistics & phonetics. 1998; 12(1): 25-45.
- American Speech-Language-Hearing Association. Childhood apraxia of speech. 2007.
- Terband H, Maassen B, Guenther FH & Brumberg J. Computational neural modeling of speech motor control in childhood apraxia of speech (CAS). 2009.
- Namasivayam AK, Pukonen M, Goshulak D, Hard J, Rudzicz F, et al. Treatment intensity and childhood apraxia of speech. International journal of language & communication disorders. 2015; 50(4): 529-546.
- Malmenholt A, Lohmander A & McAllister A. Childhood apraxia of speech: A survey of praxis and typical speech characteristics. Logopedics Phoniatrics Vocology. 2017; 42(2): 84-92.
- Shakibayi MI, Zarifian T & Zanjari N. Speech characteristics of childhood apraxia of speech: A survey research. International Journal of Pediatric Otorhinolaryngology. 2019; 126: 109609.
- Zuk J, Iuzzini-Seigel J, Cabbage K, Green JR & Hogan TP. Poor speech perception is not a core deficit of childhood apraxia of speech: Preliminary findings. Journal of Speech, Language, and Hearing Research. 2018; 61(3): 583-592.
- Iuzzini J. Inconsistency of speech in children with childhood apraxia of speech, phonological disorders, and typical speech (Doctoral dissertation, Indiana University). 2012.
- Shriberg, Lawrence D. "A neurodevelopmental framework for research in childhood apraxia of speech." Speech motor control: New developments in basic and applied research. 2010; 259-270.
- Kopera HC & Grigos MI. Lexical stress in childhood apraxia of speech: Acoustic and kinematic findings. International Journal of Speech-Language Pathology. 2020; 22(1): 12-23.
- Peter B & Stoel-Gammon C. Subsyllabic component durations in three children with suspected childhood apraxia of speech, two children with typical development, one child with phonologic delay, and one adult. In Child Phonology Conference Chicago: Vancouver, and American Speech, Language, and Hearing Association Convention. 2003; 1-4.
- Newmeyer AJ, Aylward C, Akers R, Ishikawa K, Grether S, Degrauw T & White J. Results of the sensory profile in children with suspected childhood apraxia of speech. Physical & Occupational Therapy in Pediatrics. 2009; 29(2): 203-218.
- Forrest K. Diagnostic criteria of developmental apraxia of speech used by clinical speech-language pathologists. 2003.

