Case Report - Volume 2 - Issue 6
Unusual presentation of giant perinephric abscess with lower limb involvement
Ziv Savin1* ; Ibrahim Fahoum2; Nicola J Mabjeesh3; Boaz Sagie4
1Departments of Urology, Tel Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv, Israel.
2Department Pathology, Tel Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv, Israel.
3Department of Urology, Soroka University Medical Center, Ben-Gurion University of the Negev, Beer Sheva, Israel.
4General surgery, Tel Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv, Israel.
Received Date : Sep 15, 2022
Accepted Date : Oct 24, 2022
Published Date: Nov 14, 2022
Copyright:© Ziv Savin 2022
*Corresponding Author : Ziv Savin, Department of urology, Sourasky Medical Center, 6423906, Tel Aviv, Israel.
Email: zivsavin23@gmail.com
DOI: Doi.org/10.55920/2771-019X/1293
Abstract
Perinephric abscess is a complication of urinary tract infection. It has the potential to extend beyond the Gerota’s fascia and cause serious illness. We report for the first time on an unusual presentation of a perinephric abscess crossing anatomical sections and extending through the inguinal canal to the ipsilateral lower limb. Treatment was immediate and involved multi-disciplinary operations.
Keywords: Perinephric abscess; Gerota’s fascia; Lower limb; Nephrectomy.
Introduction
A perinephric abscess is a collection of pus in the perinephric space, and represents an unusual complication of urinary tract infection, mainly caused by gram negative organisms and anaerobes [1]. The clinical presentation is usually fever and flank pain, and diagnosis is often established by computed tomography (CT) imaging [2] together with positive urine cultures [3]. Treatment is often based on antimicrobial coverage, drainage of collections, and correction of any treatable underlying predisposing cause [4]. We report, for what we believe to be the first time, an unusual presentation of a perinephric abscess extending through the inguinal canal to the ipsilateral lower limb.
Case presentation
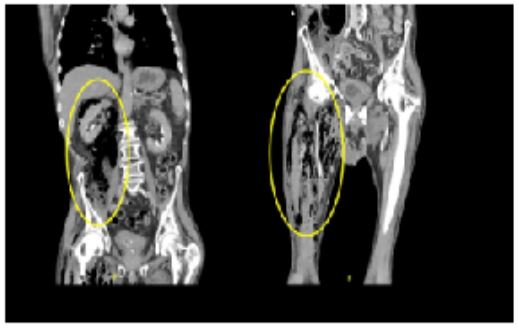
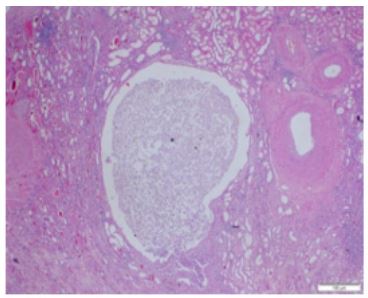
A 78-year-old male arrived to the emergency room in a poor clinical state and complaining of right lower limb pain. His medical history included peripheral vascular disease and recurrent urinary tract infections due to benign prostate hyperplasia. His vital signs were within normal limits. The physical examination was notable for altered mental status and stupor, right costovertebral angle tenderness, and a warm, red right thigh with subcutaneous emphysema. The blood workup revealed leukocytosis and elevated C-reactive protein. He was referred to a CT scan based on a clinical impression of deep soft tissues gas gangrene. CT revealed a giant right perinephric abscess spreading into the psoas and continuing caudally to the right lower limb (Figure 1). An urgent multidisciplinary meeting was held, concluding that immediate surgery was essential for the patient's survival despite the high risk of perioperative mortality. Broad spectrum intravenous antibiotics were initiated, and an exploratory laparotomy was performed. A large right retroperitoneal abscess involving the kidney and the psoas was identified and drained, and a right total nephrectomy was performed to an ill-appearing kidney. Extensive debridement of thigh muscles and a fasciotomy were carried out as well. The pathology specimens were consistent with necrotizing inflammation and abscess formation of the kidney (Figure 2) and the muscles. Blood and pus cultures were positive for extended spectrum beta-lactamases gram negative Klebsiella pneumoniae. The intraoperative and microbial findings confirmed the diagnosis. Despite all supportive efforts in the intensive care unit, the patient developed multi-organ failure and died on the second postoperative day.
Figure 1: Computed tomography images of the perinephric abscess extending to the ipsilateral lower limb.
Figure 2: Necrotizing pyelonephritis with abscess formation.
Discussion
Perinephric abscess is uncommon and often misdiagnosed due to its insidious nature. Renal calculi, diabetes mellitus, urologic manipulation and immunosuppression are the main risk factors [3]. Management of a perinephric abscess is generally conservative or minimally invasive [5]. It usually requires the draining of purulent material, since medical treatment is predictably satisfactory for small abscesses, i.e., less than 3cm [3]. Surgical exploration is reserved only for severe uncontrolled cases. Although nephron-sparing interventions are more desirable, nephrectomy is indicated in cases of extensive parenchymal damage or severe sepsis [5]. Meng et al. reported that 16% of perinephric abscess cases would require surgical exploration and nephrectomy, with associated mortality rates of 12% [3].
The Gerota's fascia is comprised of the fascia of Toldt anteriorly and the fascia of Zuckerkandl posteriorly. Inferiorly, these fasciae fail to fuse with the continuum of the perinephric and pelvic fat. Perinephric collection has the potential to rupture through Gerota’s fascia into the pararenal spaces and extend to adjacent structures [4]. Extensions to the thorax, [6,7] the spleen, [8] the mediastinum, the epidural space, [9] and even intraperitoneally to the colon [10] have been described. However, our literature search failed to yield any similar cases in which the abscess reached the lower limbs. Our patient had an unusual extension of a giant perinephric abscess inferiorly to the inguinal canal and the anterior thigh. The initial presentation was misleading and concentrated on the soft tissues of the lower limb. Only thorough investigation revealed the whole picture. A multidisciplinary surgical intervention was mandatory to maximize prognosis, and the team was comprised of urologists, general surgeons, and orthopedic surgeons. We were aware that the extensions of the abscess to adjacent organs and anatomical compartments raised the risk of morbidity and portended a grim outcome. Despite all of our efforts, our patient did not survive the postoperative period.
Statement of Ethics: The deceased subject family has given its written informed consent to publish the case.
Disclosure Statement: The authors have no conflicts of interest to declare.
Funding Sources: The authors declare that there were no funding sources.
Author Contributions
All authors discussed the results and contributed to the final manuscript.
Ziv Savin imported all the case’s clinical details.
Ibrahim Fahoum provided all the case’s pathological details.
Nicola J Mabjeesh and Boaz Sagie made critical revision of the manuscript for important intellectual content.
References
- Coelho RF, et al. Renal and perinephric abscesses: Analysis of 65 consecutive cases. World J. Surg. 2007. [DOI:10.1007/s00268-006-0162-x].
- Haddad MC, et al. Radiology of perinephric fluid collections. Clinical Radiology, 2002. [DOI:10.1053/crad.2001.0854].
- MENG MV, MARIO LA & McANINCH JW. Current Treatment and Outcomes of Perinephric Abscesses. J. Urol. 2002. [DOI:10.1097/00005392-200210010-00007].
- Gardiner RA, Gwynne RA & Roberts SA. Perinephric abscess. BJU Int. 2011. [DOI:10.1111/j.1464-410X.2011.10050.x].
- Lee C & Henderson SO. Emergent surgical complications of genitourinary infections. Emergency Medicine Clinics of North Americ, 2003. [DOI:10.1016/S0733-8627(03)00067-1].
- Pérez JMH, Suárez PMR & Gilart JF. Empiema pleural secundario a pionefrosis. Archivos de Bronconeumologia, 2008. [DOI:10.1157/13119945].
- Granados Loarca EA, Quezada Ochoa RE & Salazar Monterroso CB. Renal abscess perforated into the thorax. Actas Urologicas Espanolas, 2004.
- Reese JH, Anderson RU & Friedland G. Splenic abscess arising by direct extension from a perinephric abscess. Urol. Radiol. A J. diagnostic imaging, 1990. [DOI:10.1007/BF02923976].
- Krishna GS, Vijayalakshmidevi B, Lakshmi AY, Mutheswaraiah B & Sivakumar V. Perinephric abscess with extension into mediastinum and epidural space. Indian J. Nephrol. 2012. [DOI:10.4103/0971-4065.98770].
- Truesdale BH, Rous SN & Nelson RP. Perinephric abscess: a review of 26 cases. J. Urol. 1977; 118: 910–1.