Case Report - Volume 2 - Issue 6
Large Colonic Lipoma: An Unusual Presentation and Colonoscopic Resection
Ribas Pedro HBV; Oliveira Vl; Bestetti AM* ; Sasso JGRJ; De Moura EGH
Department of Gastroenterology, University of São Paulo, Brazil.
Received Date : Sep 16, 2022
Accepted Date : Oct 28, 2022
Published Date: Nov 16, 2022
Copyright:© Bestetti AM 2022
*Corresponding Author : Alexandre Moraes Bestetti, Department of Gastroenterology, University of São Paulo, Brazil.
Email: bestetti.alexandre@gmail.com
DOI: Doi.org/10.55920/2771-019X/1295
Introduction
Lipomas are a very common benign neoplasm, the most common soft-tissue tumor, consisting of mature fat cells enclosed by a capsule. They are mostly superficial and located at the subcutaneous tissue of any part of the body [1]. However, they can be found at other sites, such as the central nervous system, abdominal solid organs and also in a subepithelial presentation in any part of the gastrointestinal (GI) tract [2-4].
In most cases, especially in organ presentation, patients are asymptomatic and lipomas are incidentally diagnosed through routine imaging or lower and upper endoscopy exams. They have specific traits that do not need biopsies and its benign condition often does not require exeresis. Exceptions can be made for larger lesions, with cosmetic or functional disturbances.
Regarding lipomas presenting as subepithelial lesions (SEL) of the GI tract, complications are uncommon and usually manifest as bleeding, intussusception, bowel obstruction [5], and rarely as rectal prolapse. We report here a case of a submucosal colonic lipoma misinterpreted as rectal mucosal prolapse.
Case presentation
A 39-year-old female came for a colonoscopy, with a history of constipation, tenesmus and a mobile rectal lump that was partially externalized during defecation, which she pushed back into her rectum after every evacuation, for over 3 years. She had been evaluated by a proctologist that diagnosed it as rectal prolapse, and ordered a pre-operative colonoscopic evaluation.
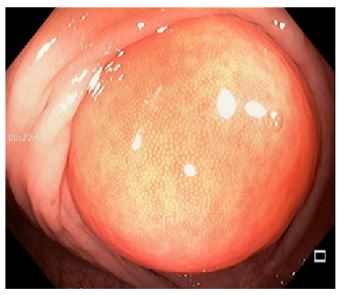
Digital rectal examination had no abnormalities, without any palpable masses. During the colonoscopic evaluation, a mobile, large, with short pedicle mass was spotted (Figure 1), located in distal sigmoid colon, with about 60mm in the largest axis and occupied the whole lumen. It had normal overlying mucosa, a yellowish hue, and soft consistency. The rest of the exam had no other abnormalities. The initial hypothesis was a subepithelial lipoma (Figure 2).
Figure 1: Short pedicled mass in sigmoid colon.
Figure 2: Yellowish hue occupying the whole lumen.
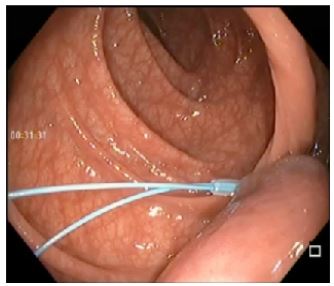
Considering the patient's symptoms and the risk of sigmoidoanal intussusception, we opted for an endoscopic exeresis. An endoloop ligation was performed, tightened at the base of the stalk, with mucosa color changing to dark red, confirming adequate positioning (Figure 3).
Figure 3: Positioned endoloop.
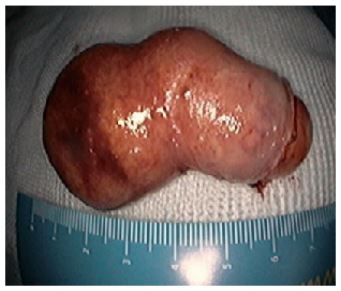
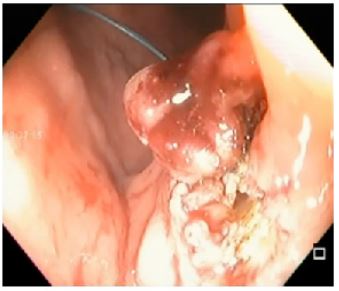
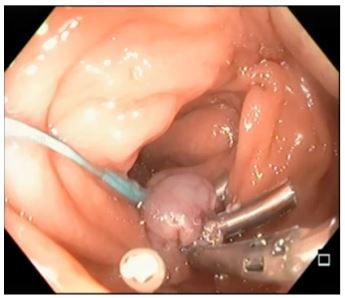
After the loop was positioned, a braided snare was placed above the closed endoloop and a cautery-assisted resection was performed with coagulation followed by ENDO-Cut (Figure 4 & 5) Although the endoloop was correctly placed, after the resection there was a possible millimetric perforation(Figure 6) An endoscopic repair was performed with three endoclips (Figure 7) The whole colonoscopic procedure was insufflated with carbon dioxide.
Figure 4: Braided snare below endoloop.
Figure 5: Mass after resection.
Figure 6: Colonic perforation.
Figure 7: Defect closure with endoclips.
The patient was admitted for a 48-hour vigilance. The patient was discharged two days after the procedure, asymptomatic, and defecating without tenesmus. On one-week and one-month phone follow-up, the patient had no symptoms, no delayed bleeding, abdominal pain or tenesmus. The histopathological evaluation confirmed a subepithelial lipoma completely resected.
Discussion
Lipomas of the GI tract are a benign and usually asymptomatic condition, most common in the colon with a general incidence of 0,2 to 4,4%, followed by the gastric antrum [5]. Among the benign SEL of the GI tract, they are the most common in the colon and second in the stomach [6], after leiomyomas. GI stromal tumors are the most common SEL overall [7]. Lipomas have some specific features at endoscopic imaging, such as yellowish hue and soft touch at forceps probe (pillow sign) [7] that often establish the definitive diagnosis without the need of complementary evaluation or biopsies.
If complementary investigation is required, for example when there are abnormal morphological characteristics or rapid growth, endoscopic ultrasound (EUS) is the most accurate and indicated method for this purpose. At EUS imaging, lipomas are homogeneous and hyperechoic lesions with well-defined limits arising from the submucosal layer (or third layer) [7]. Tissue samplings are usually not necessary to confirm the diagnosis when these typical characteristics are present. Submucous colonic lipomas may be sessile or pedunculated, accounting for 90% of the colorectal lipomas. The remaining 10% are subserous. 90% are in the ascending colon. Most of them are smaller than 2cm without the need for surveillance or resection. However, when larger than 4cm, 75% are symptomatic with pain, bleeding and even urgent situations such as colonic intussusception and bowel obstruction [3].
In complicated presentations, lipomas can be referred for resection and multiple options are available, from surgical treatment to many endoscopic resection techniques. Traditionally, surgical treatment was the preferred option for lesions >4cm due to its submucosal origin, and the risk of a large pedicle being formed by a serosal invagination, and could contain the deeper muscular layer, leading to a non-negligible risk of perforation in endoscopic resections [8]. However, endoscopic techniques and devices have evolved recently and now, the endoscopic approach could be the treatment of choice. The use of endoloop with or without complete snare resection using electrocautery has been described as a safe method for resection [4,7-8].
Even when complications arise, as in the case presented above, the possibility of an endoscopic resolution of the adverse event represents an evolution in therapeutic endoscopy, widening the capabilities of non-invasive procedures and avoiding surgery. Previous studies have proven that deep mural injuries and colonic perforations may be closed with endoclips [9].
Other techniques may be used for resection, such as endoscopic submucosal dissection, submucosal tunneling and endoscopic full-thickness resection, but those techniques require a specific skill set and a longer procedure duration that may not be widely available [7]. The management of colonic lipomas depend on size, location, symptoms and confirmed diagnosis, as abnormal characteristics may demand further investigation. Asymptomatic lipomas do not require follow-up or intervention. Symptomatic ones could be resected through endoscopic procedures [4,6-7].
References
- Johnson CN, Ha AS, Chen E, Davidson D. Lipomatous Soft-tissue Tumors. J Am Acad Orthop Surg. 2018; 26(22): 779-788. [PMID: 30192249 DOI: 10.5435/JAAOS-D-17-00045].
- WHO Classification of Tumours of the Central Nervous System, 4th ed, Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (Eds), International Agency for Research on Cancer, 2016.
- Zhang H, Cong JC, Chen CS, Qiao L, Liu EQ. Submucous colon lipoma: a case report and review of the literature. World J Gastroenterol. 2005; 11(20): 3167-9. [PMID: 15918213; PMCID: PMC4305863 DOI: 10.3748/wjg.v11.i20.3167].
- Deprez PH, Moons LMG, OʼToole D, Gincul R, Seicean A, Pimentel-Nunes P, et al. Endoscopic management of subepithelial lesions including neuroendocrine neoplasms: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022; 54(4): 412-429. [PMID: 35180797 DOI: 10.1055/a-1751-5742].
- Grasso E, Guastella T. Giant submucosal lipoma cause colo-colonic intussusception. A case report and review of literature. Ann Ital Chir. 2012; 83(6): 559-62. PMID: 23110909.
- Fernandez MJ, Davis RP, Nora PF. Gastrointestinal lipomas. Arch Surg. 1983; 118(9): 1081-3. [PMID: 6615219 DOI: 10.1001/archsurg.1983.01390090065015].
- Standards of Practice Committee, Faulx AL, Kothari S, Acosta RD, Agrawal D, et al. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest Endosc. 2017; 85(6): 1117-1132. [PMID: 28385194 DOI: 10.1016/j.gie.2017.02.022].
- Lee SH, Park JH, Park DH, Chung IK, Kim HS, Park SH, et al. Endoloop ligation of large pedunculated submucosal tumors (with videos). Gastrointest Endosc. 2008; 67(3): 556-60. [PMID: 18294522 DOI: 10.1016/j.gie.2007.10.049].
- Benites Goñi H, Palacios Salas F, Marin Calderón L, Bardalez Cruz P, Vásquez Quiroga J, Alva Alva E, et al. Closure of colonic deep mural injury and perforation with endoclips. Rev Esp Enferm Dig. 2020; 112(10): 772-777. [PMID: 32954773 DOI: 10.17235/reed.2020.6880/2020].