Research Article - Volume 2 - Issue 6
The Utility of Performing Screening Hip Ultrasound for Evaluation of Developmental Dysplasia of the Hip in Extremely Preterm Infants
Baotran N Vo1*; Meryle Eklund2; Heather ollins3; Julie Ross4; Robert F Murphy5
1Medical Student, University of the Incarnate Word School of Osteopathic Medicine, USA.
2Departments of Radiology and Pediatrics, Medical University of South Carolina, Charleston, SC, USA.
3Department of Radiology, Medical University of South Carolina, Charleston, SC, USA.
4Department of Pediatrics, Division of Neonatology, Medical University of South Carolina, Charleston, SC, USA.
5Department of Orthopaedics and Physical Medicine, Medical University of South Carolina, Charleston, SC, USA.
Received Date : Sep 28, 2022
Accepted Date : Nov 04, 2022
Published Date: Nov 28, 2022
Copyright:© Baotran N Vo 2022
*Corresponding Author : Baotran N Vo, Medical Student, University of the Incarnate Word School of Osteopathic Medicine, 7615 Kennedy Hill, Building 1, San Antonio, TX 78235, USA. Tel: 714-548-6590; Fax: 714-548-6590
Email: bnvo@student.uiwtx.edu
DOI: Doi.org/10.55920/2771-019X/1306
Abstract
Objective: Hip ultrasound (US) is recommended to screen at risk infants for developmental dysplasia of the hip (DDH), however few studies have investigated DDH in extremely preterm infants (<28 weeks gestational age). We aim to evaluate whether US screening for DDH is warranted in this population.
Study Design: We conducted a retrospective review of 2166 consecutive dynamic infant hip US studies. After exclusion criteria were applied, clinical and imaging factors were evaluated in the remaining 1113 subjects. Statistical analysis was targeted to evaluate the association between gestational age and incidence of DDH.
Result: Of 63 extremely premature infants, only one was diagnosed with DDH. In the remaining1050 infants, 91 infants were diagnosed with DDH. The incidence of DDH was significantly lower (p=0.04) in extremely preterm infants.
Conclusion: The incidence of DDH in extremely premature infants is significantly lower than other neonates but can occur in some high-risk patients.
Introduction
Developmental dysplasia of the hip (DDH) involves abnormal development of the acetabulum and femoral head due to mechanical instability of the hip joint [1,2]. If left untreated, DDH can lead to pain, a vascular necrosis, osteoarthritis, discrepancy in leg length, abnormal gait, and reduced mobility by early adulthood [3,4]. DDH is often detected by abnormal physical exam findings in the early postnatal period and if diagnosed appropriately and treated successfully, many children are able to develop a normal hip joint without functional limitation [5].
Screening guidelines have been established in the United States to promote early identification of at-risk infants and expedite appropriate orthopedic evaluation and treatment in order to mitigate adverse long-term outcome. The American College of Radiology Appropriateness Criteria for DDH recommends ultrasound (US) examination for infants between 4 weeks to 4 months of age with equivocal physical examination or risk factors for DDH, and for infants younger than 4 months with physical examination findings of DDH; however, no specific consideration is given for the patient’s gestational age (GA) at birth [1,6]. The American Academy of Pediatrics 2016 Guideline for DDH is generally similar, but explicitly states that breech presentation should prompt imaging screening in an otherwise normal patient when present in the third trimester only [4].
Few studies have explored the association of premature birth and DDH, and there is little published data on the incidence of DDH in extremely preterm infants (born before 28 weeks GA) [2,7-9]. As the number of extremely preterm infant births and percentage survival has increased over the past few decades [10], there is increased need to determine appropriate screening guidelines in this vulnerable patient population, particularly in the setting of known risk factors in other patient groups, such as breech position in utero, oligohydramnios, female sex, primiparity, family history of DDH, certain neuromuscular and musculoskeletal disorders, and improper swaddling [1,3,11,12]. We aim to evaluate whether extremely preterm infants warrant US screening for DDH as compared to other preterm and term infants (born at or after 28 weeks GA).
Materials and methods
Study sample
Our institutional review board approved this study, which complied with the Health Insurance Portability and Accountability Act. A retrospective review of all consecutive dynamic infant hip US studies (CPT code 76885) performed at the Medical University of South Carolina University Hospital from July 2014 through December2019 was conducted. Subjects with undocumented GA were excluded, as were data from repeat examinations performed for follow up of initial US findings at our hospital or referring institutions.
Imaging examination
Hip US was performed by experienced pediatric sonographers using a high frequency linear array transducer and standard static and dynamic techniques [13]. Studies were interpreted at the time of examination by board-certified pediatric radiologists (Figure 1). Orthopedic evaluation and treatment were provided by pediatric orthopedic subspecialists.
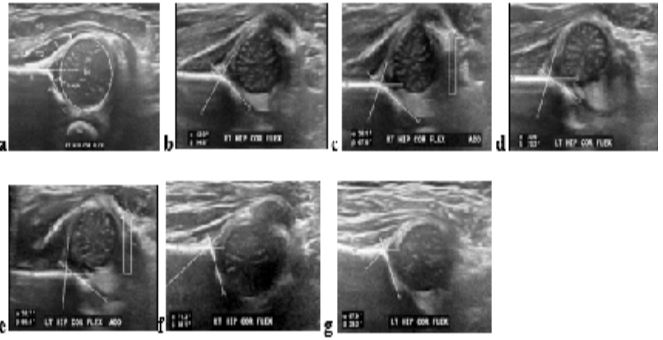
Figure 1: Hip ultrasound evaluation.
line circle), iliac bone (Ili), acetabulum (Ac), Ischium (Isch), triradiate cartilage (TC), labrum (L), joint capsule (small arrows) and lateral musculature (open arrows). The α angle is an important measurement in evaluation of hip dysplasia, formed by the acetabular roof and lateral cortex of the iliac bone b) A patient with hip dysplasia has abnormal acetabular morphology and corresponding α angle measurement of < 6)0 degrees c) Lateral subluxation of the femoral head occurs with adduction (arrow) and stress maneuvers (not pictured). d, e) Images of the left hip in the same patient demonstrate similar abnormal morphologic and dynamic findings of hip dysplasia f, g) After treatment with Pavlik harness, the acetabular morphology has normalized, with acetabular angles > 60 degrees and adequate acetabular coverage of the femoral head bilaterally. No imaging or clinical features of hip dysplasia remained in this successfully treated patient.
Data Collection
Subject sex, estimated GA at birth, corrected age at time of US examination, in utero fetal lie, amniotic fluid volume, delivery method, imaging setting (inpatient versus outpatient), ace tabular alpha angles, hip alignment, evidence of hip instability, types of treatments pursued, and long-term outcomes were recorded (if known) based on provider notes in the electronic medical record. For the purposes of this study, subjects with a stated history of “term” delivery, but with an unknown exact gestational age at birth were assigned a gestational age of 40.0 weeks, as an approximate average of the 39 0/7 weeks to 40 6/7 weeks defined as “full term” by the American College of Obstetrics and Gynecology [14]. Note was made of any coexisting musculoskeletal or systemic conditions with a known association with higher incidence of DDH (Table 1). Radiology images and reports were reviewed for accuracy. There was some mild variation in reporting of US imaging, diagnosis of hip condition, and orthopedic management. For the purposes of the study, an algorithm was created to classify subjects into three categories: normal, immaturity of the hips, and hip dysplasia (Figure 2).
Table 1: Coexisting anomalies in subjects.
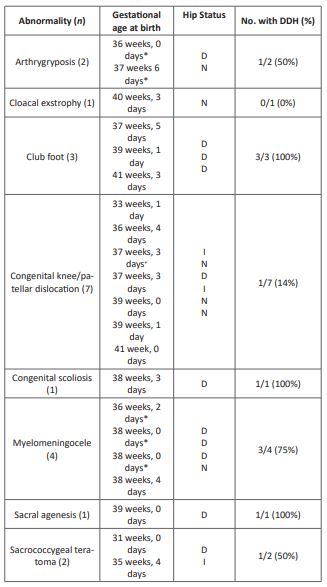
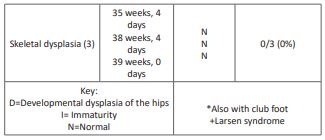
Figure 2: Algorithm for classifying hip status.
Statistical analysis
Frequency of dysplasia by sex and weeks of gestational age (WGA) was evaluated with chi-square tests with Fisher’s exact tests used when data table cells had frequencies <5. Relative risk ratios were calculated to evaluate the dysplasia risk in older groups relative to extreme preterm infants. Data are summarized with median, interquartile range (IQR: showing where the middle 50% of subjects lie), and range where applicable. Other frequencies related to dysplasia are summarized with percentages and number of subjects. Statistical significance was set at α<.05, two-sided p-values are reported, and analyses were conducted with SPSS version 25 (IBM: Armonk, NY).
Results
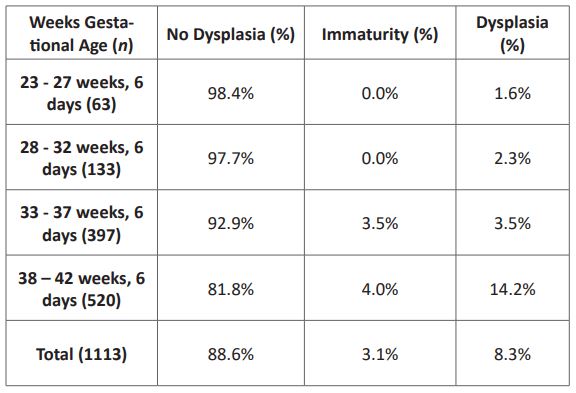
Out of 2166 total hip US studies performed as a primary encounter at our institution, 683 were excluded due to unknown GA of the subject and 370 were excluded due to performance of prior hip ultrasound or known diagnosis of DDH, leaving 1113 infants for evaluation.714 subjects (64.2%) were female, and 399 (35.8%) were male. The stated reason for the examination was breech positioning in 73.5%, physical examination concerns for hip instability in 15.9%, and other reasons in 10.6% of subjects. Ninety-four percent of subjects were imaged in an outpatient setting and 6% were imaged as inpatients. Distribution of subjects’ gestational age at birth is illustrated in (Figure 3). Sixty-three of the 1113 studied subjects (0.06%) were born extremely preterm. The corrected age at the time of hip US examination across all included subjects was a median of 42 days (IQR = 30 to 59 days) with a range of -58 to 211 days.
Normal amniotic fluid volume was documented in 52.6% (n = 585) of cases, oligohydramnios in 2.3% (n=26) and polyhydramnios in 2.3% (n = 26). Preterm premature rupture of membranes of unknown duration was documented in 8.4% (n = 94) of cases, and volume of amniotic fluid could not be determined from the available records in 34% (n = 382) of cases. Seventy-six percent (n=843) of subjects were born via Cesarean section and 17% (n = 188) were delivered vaginally.
Ninety-two (8.3%) patients were diagnosed with DDH, 35 (3.1%) with immaturity of the hips, and 986 (88.6%) were normal. Hip status relative to gestational age at birth is represented in (Table 2), with incidence of DDH by gestational age displayed on (Figure 3). All subjects classified as having immaturity of the hips were imaged at less than 12 weeks corrected age. Of the subjects with DDH, bilateral dysplasia (n = 63; 68.5%) was significantly more likely to occur than dysplasia only on the left (n = 25; 27.2%) or right (n = 4; 4.3%) side (p< .001.) The ratio of females (n=77; 83.7%) relative to males (n=15; 16.3%) was significantly higher in the dysplasia group, (p<.001). Of the 63 extremely preterm infants, only one infant had positive findings of DDH, and the incidence of hip dysplasia in extremely premature infants was significantly lower than patients born at or after 28 weeks GA (1.6% compared with 8.7%, respectively, p = .04). In conglomerate, infants born at or after 28 weeks gestational age were 5.46 times as likely to be diagnosed with DDH as extremely preterm infants and in the group born at or after 38 weeks gestational age, infants were 8.94 times as likely to have dysplasia.
In the subject group determined to have no dysplasia, none of the subjects received treatment for DDH. Of the subjects with immaturity of the hips, 17.1% (n=6) percent were treated with a Pavlik harness, 80% (n=28) received no treatment. Eighty percent (n=28) had a normal/normalized hip examination and 20% (n=7) were lost to follow-up. In the group with DDH, 84.8% (n=78) received treatment. This includes 59.8% (n=55) who wore a Pavlik harness, 10.9% (n=10) treated with a Rhino brace, 12.0% (n=11) who received surgical correction, 1.1% (n=1) 1 treated with casting only and 1.1% (n=1) with undocumented treatment type. Treatment was deferred due to coexisting comorbidities or subjects expired or were lost to follow up in the remaining 15.2% (n=14) of subjects. Patients treated for DDH had normalized hip examination 71.8% (n=66) of the time with 19.6% (n=18) of subjects still in the treatment phase at the time of data collection or no follow up documented in 8.7% (n=8) of cases.
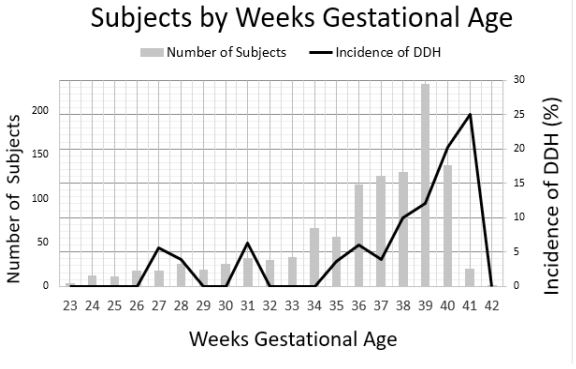
Figure 3: Subjects by weeks gestational age.
Table 2: Hip Status by Gestational Age.
Discussion
Hip instability in neonates can occur across a spectrum, as evidenced in some patient’s by physiologic laxity of the hip and immaturity of the acetabulum which resolves clinically and by imaging in the first few months of life. This may be due to maternal hormones that relax maternal ligaments during delivery and also affect the fetus [1]. Hip dysplasia is a condition that results from persistent abnormal laxity of the hip joint and involves abnormal development of the acetabulum and femoral head. It is a heterogeneous disorder that may be seen in otherwise healthy infants with known risk factors (female sex, family history, primiparity, breech presentation, and oligohydramnios). Hip dysplasia can also occur in certain medical conditions and syndromes, and usually has a worse prognosis (including abnormalities in collagen metabolism, neural tube defects, arthrogryposis, sacrococcygeal teratoma, and bladder exstrophy) [15-17].
Uterine risk factors, such as primiparity, fetal lie, and volume of amniotic fluid likely have an influence on development of DDH during the third trimester, whenfetal extremity motion is more restricted [5,18]. There is a normal decline in amniotic fluid volume after 28 weeks GAleading to reduced intrauterine space [10,19] and there is additional literature to support that rates of DDH increase significantly in near-term, term, and post-term infants [2,20]. Our data is in agreement with this prior published data, as we have also shown a low rate of DDH in extremely preterm infants as well as an increasing incidence of DDH with increasing GA at birth. In the one extremely preterm infant who was diagnosed and treated for DDH in our study, we suspect that a known prolonged seven-week episode of severe oligohydramnioscontributed significantly to the development of DDH, akin to other published data that suggest an association between oligohydramnios and DDH [21,22].
Universal imaging-based screening for hip dysplasia is impractical, resulting in overall increase in healthcare costs without adding benefits to patient care [4,23,24]. Robust screening guidelines have thus been developed for evaluation of DDH in otherwise healthy term or near-term infants, however DDH is understudied in premature populations. With a growing survivorship of among extremely preterm neonatal intensive care graduates, referral practices for imaging and orthopedic consultation in this patient group are left to the discretion of perinatologists. Our data show that the incidence is of DDH is diminished in infants born extremely preterm, but the risk is not zero. Uterine risk factors such as abnormal fetal lie and primiparity are unlikely to have the same adverse effect on hip development in the second trimester when compared to patients born in the third trimester, whereas conditions that significantly limit intrauterine space and contribute to abnormal extremity positioning (such as prolonged preterm premature rupture of membranes) may increase the risk of DDH. Patients with known neurologic and musculoskeletal conditions which have a higher association with DDH should still be evaluated and screened for DDH regardless of GA at birth.
One of the challenges in studying extremely premature infants who are examined with hip ultrasound is the low number of infants overall who can be included in the target study group. Although survival of extremely premature infants is increasing, these patients still make up a very small portion of patients who meet criteria for hip US. In our patient cohort, only 63 extremely preterm patients met inclusion criteria for the study.
Another barrier is lack of available clinical data. Despite the increase in use of electronic medical records, we encountered substantial challenges in acquiring target data from referring clinicians outside of our institution network. Approximately 30% of possible hip ultrasound studies were excluded for our study, primarily due to unknown GA at birth (683 patients). While GA was easily determined from the electronic medical record for subjects evaluated at our institution by the neonatal and pediatric orthopedic teams, referrals from outside providers often lacked this piece of clinical information. Also, whether born at our institution or elsewhere, amniotic fluid status was not known in enough subjects to meaningfully correlate with incidence of DDH.
Since our study is a retrospective review, other limitations include that subjects were not specifically matched for sex, amniotic fluid status, fetal lie, or other factors. Family history and primiparity were not evaluated due to insufficient data in the electronic medical record. Large birth weight (>5kg) and multiple gestation have also been correlated with DDH risk, but these factors were not assessed in our study [9,25,26].
Conclusion
Appropriate screening guidelines for DDH should be developed or adapted to encompass extremely preterm infants in order to ensure appropriate utilization of medical imaging and promote effective management in this increasing population. Recognition of high-risk factors for DDH (prolonged preterm premature rupture of membranes, coexisting musculoskeletal disorders, sacrococcygeal teratoma, and bladder exstrophy) may warrant heightened awareness of hip dysplasia screening in this population. We also advocate for repeat clinical hip examination in extremely preterm infants prior to discharge to assess clinical indications for screening. Future direction of research may require pooling data from multiple institutionsto increase study power and performing prospective studies that target evaluation of specific risk factors in the extremely preterm population.
Acknowledgement
Many thanks to the American College of Radiology (ACR) and the Nth Dimensions Program, who provided support for this project.
Conflict of Interest
None of the authors have a competing financial interest or other conflict of interest in relation to the work described.
Author Contributions
Baotran Vo – Completed data collection from chart and image review and significantly contributed to data analysis. Contributed significantly to manuscript production and will serve as corresponding author for the manuscript.
Dr. Meryle Eklund – Conceived the idea for the project; provided considerable guidance and mentorship to Baotran Vo in completing data collection and interpretation; collected multidisciplinary input while carrying out the project. Contributed to manuscript production.
Dr. Robert Murphy – Contributed to project development and manuscript production.
Dr. Julie Ross - Contributed to project development and manuscript production.
Dr. Heather Collins – Provided expertise in statistical analysis of data. Contributed to manuscript production.
Funding Information
No funding was received to support this project at any stage.
References
- Karmazyn BK, Gunderman RB, Coley BD, Blatt ER, Bulas D, Fordham L, et al. ACR Appropriateness Criteria on developmental dysplasia of the hip--child. J Am Coll Radiol [Internet]. 2009; 6(8): 551-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19643382
- Lee J, Spinazzola RM, Kohn N, Perrin M, Milanaik RL. Sonographic screening for developmental dysplasia of the hip in preterm breech infants: do current guidelines address the specific needs of premature infants? J Perinatol [Internet]. 2016; 36(7): 552-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26914014
- Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet (London, England) [Internet]. 2007; 369(9572): 1541-52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17482986
- Shaw BA, Segal LS, Section on Orthopaedics. Evaluation and Referral for Developmental Dysplasia of the Hip in Infants. Pediatrics [Internet]. 2016; 138(6). Available from: http://www.ncbi.nlm.nih.gov/pubmed/27940740
- Storer SK, Skaggs DL. Developmental dysplasia of the hip. Am Fam Physician [Internet]. 2006; 74(8): 1310-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17087424
- Expert Panel on Pediatric Imaging, Nguyen JC, Dorfman SR, Rigsby CK, Iyer RS, Alazraki AL, et al. ACR Appropriateness Criteria® Developmental Dysplasia of the Hip-Child. J Am Coll Radiol [Internet]. 2019; 16(5S): S94-103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31054762
- Orak MM, Onay T, Gümüştaş SA, Gürsoy T, Muratlí HH. Is prematurity a risk factor for developmental dysplasia of the hip? : a prospective study. Bone Joint J [Internet]. 2015; 97-B(5): 716-20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25922469
- Misanovic V, Jonuzi F, Maksic-Kovacevic H, Rahmanovic S. Ultrasound in detection of developmental hip dysplasia in premature born children. Acta Inform Med [Internet]. 2015; 23(2): 73-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26005270
- Sezer C, Unlu S, Demirkale I, Altay M, Kapicioglu S, Bozkurt M. Prevalence of developmental dysplasia of the hip in preterm infants with maternal risk factors. J Child Orthop [Internet]. 2013; 7(4): 257-61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24432084
- Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Analg [Internet]. 2015; 120(6): 1337-51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25988638
- Chan A, McCaul KA, Cundy PJ, Haan EA, Byron-Scott R. Perinatal risk factors for developmental dysplasia of the hip. Arch Dis Child Fetal Neonatal Ed [Internet]. 1997; 76(2): F94-100. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9135287
- Paton RW, Hinduja K, Thomas CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip. A ten-year prospective study. J Bone Joint Surg Br [Internet]. 2005; 87(9): 1264-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16129755
- AIUM-ACR-SPR-SRU Practice Parameter for the Performance of an Ultrasound Examination for Detection and Assessment of Developmental Dysplasia of the Hip. J Ultrasound Med [Internet]. 2018; 37(11): E1-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30308084
- ACOG Committee Opinion No 579: Definition of term pregnancy. Obstet Gynecol [Internet]. 2013; 122(5): 1139-40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24150030
- Loder RT, Skopelja EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop [Internet]. 2011; 2011: 238607. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24977057
- Kremer MEB, Althof JF, Derikx JPM, Van Baren R, Heij HA, Wijnen MHWA, et al. The incidence of associated abnormalities in patients with sacrococcygeal teratoma. J Pediatr Surg [Internet]. 2018; 53(10): 1918-22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29453131
- Mundy A, Kushare I, Jayanthi VR, Samora WP, Klingele KE. Incidence of Hip Dysplasia Associated With Bladder Exstrophy. J Pediatr Orthop [Internet]. 2016; 36(8): 860-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26090968
- Lange AE, Lange J, Ittermann T, Napp M, Krueger PC, Bahlmann H, et al. Population-based study of the incidence of congenital hip dysplasia in preterm infants from the Survey of Neonates in Pomerania (SNiP). BMC Pediatr [Internet]. 2017; 17(1): 78. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28302080
- Hinh ND, Ladinsky JL. Amniotic fluid index measurements in normal pregnancy after 28 gestational weeks. Int J Gynaecol Obstet [Internet]. 2005; 91(2): 132-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16126206
- Colta RC, Stoicanescu C, Nicolae M, Oros S, Burnei G. Hip dysplasia screening - epidemiological data from Valcea County. J Med Life [Internet]. 9(1): 106-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27489571
- Ömeroğlu H, Akceylan A, Köse N. Associations between risk factors and developmental dysplasia of the hip and ultrasonographic hip type: a retrospective case control study. J Child Orthop [Internet]. 2019; 13(2): 161-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30996740
- Manoukian D, Rehm A. Oligohydramnios: should it be considered a risk factor for developmental dysplasia of the hip? J Pediatr Orthop B [Internet]. 2019; 28(5): 442-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30839361
- Shorter D, Hong T, Osborn DA. Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health [Internet]. 2013; 8(1): 11-54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23878122
- Kotlarsky P, Haber R, Bialik V, Eidelman M. Developmental dysplasia of the hip: What has changed in the last 20 years? World J Orthop [Internet]. 2015; 6(11): 886-901. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26716085
- Sewell MD, Rosendahl K, Eastwood DM. Developmental dysplasia of the hip. BMJ [Internet]. 2009; 339: b4454. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19934187
- Barr LV, Rehm A. Should all twins and multiple births undergo ultrasound examination for developmental dysplasia of the hip?: A retrospective study of 990 multiple births. Bone Joint J [Internet]. 2013; 95-B(1): 132-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23307687

