Case Report - Volume 2 - Issue 6
Posterior lumbar puncture in old orthopedic table: A two case report and two videos
Luiz Eduardo Imbelloni
Anesthesiologist and Co-responsible for CET-SBA Hospital Clínicas Municipal de São Bernardo do Campo, SP, Brazil. Senior Researcher of INCA, Rio de Janeiro, RJ, Brazil”.
Received Date : Sep 30, 2022
Accepted Date : Nov 10, 2022
Published Date: Dec 03, 2022
Copyright:© Luiz Eduardo Imbelloni 2022
*Corresponding Author : Luiz Eduardo Imbelloni, Anesthesiologist and Co-responsible for CET-SBA Hospital Clínicas Municipal de São Bernardo do Campo, SP, Brazil. Senior Researcher of INCA, Rio de Janeiro, RJ, Brazil”.Tel: + 55.11.99429-3637
Email: dr.luiz.imbelloni@gmail.com; luiz.imbelloni@edu.inca.gov.br
DOI: Doi.org/10.55920/2771-019X/1311
Abstract
Objectives: The purpose of these two case reports was to demonstrate the possibility of using the space between the back and the buttocks for access to the subarachnoid space and injection of spinal anesthesia complementation.
Methods: Two patients admitted to our institution with a femoral fracture were selected to report the anesthetic approach used.Each patient had similar problems intraoperatively. The presentation, the problem that occurred during the surgery, and management plan for each patient is described.
Results: Both cases, a man and a woman, were hospitalized for fracture of the femur. Performed on both inguinal plexus block for preventive analgesia and examinations. Performed spinal anesthesia with 10 mg of 0.5% isobaric bupivacaine. During the surgical procedure, in both patients during the reduction, a distal fracture of the femur occurred, and a new spinal anesthesia was performed with puncture in the space between the back and the buttocks with a sharp needle and 15 mg of the same substance was injected, with a total of 25 mg. At the end of the surgery, a new inguinal plexus block was performed for postoperative analgesia lasting around 20 hours.
Conclusion: The use of a total of 25 mg of 0.5% isobaric bupivacaine was justified by the increase in surgery time due to the distal fracture of the femur in both patients, and by the possibility of performing a puncture between the back and the buttocks, to avoid the use of general anesthesia.
Keywords: Spinal anesthesia; Lumbar plexus block; Bupivacaine isobaric; Orthopedic surgery; Geriatric.
Introduction
There are two schools of anesthesia that teach and practice spinal anesthesia: one prefers the lateral decubitus position and the other the sitting position to access the subarachnoid space, before the injection of the local anesthetic.The anesthesiologist who remains using only the sitting position cannot offer his patients all the best techniques of spinal anesthesia, as unilateral spinal anesthesia (with hypobaric or hyperbaric solution), posterior spinal anesthesia favoring sensory roots (hypobaric solution) [1-3].
The efficacy and safety of two high-dose glucose free 0.5% bupivacaine 25 mg and 30 mg were evaluated in terms of maximal spread, regression of maximal spread, total duration of analgesia, and hemodynamic and respiratory side effects, showing that 30 mg gave a duration significantly greater than 25 mg, no difference in cephalad spread, and no severe uncontrollable haemodynamic or respiratory side effects [4].
We recently used high-dose 0.5% isobaric bupivacaine (30 mg) for the surgical treatment of complex orthopedic surgery, which was justified by the long duration of surgery, as it was not part of the hospital's therapeutic arsenal, nor of the continuous or combined spinal-epidural kits, showing that spinal anesthesia was satisfactory for a long-term major surgery, with excellent cardiocirculatory stability and without adverse events [5]. The purpose of these two case reports was to demonstrate the possibility of using the space between the back and the buttocks (Figure 1) for access to the subarachnoid space and injection of spinal anesthesia complementation (Videos 1 and 2) and show the efficacy and safety of the total dose of 25 mg isobaric 0.5% bupivacaine.
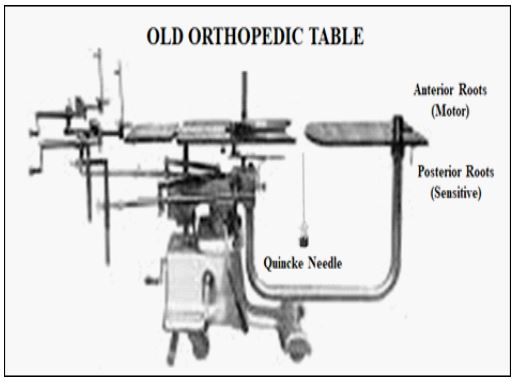
Figure 1: Old orthopedic surgery table with space between the back and buttocks.
Below is the link to the two videos
https://drive.google.com/drive/folders/12bx4zHCyjpnZ5QvVIHmDBANMN1uzsyI9?usp=sharing
Case 1
A 87-year-old female, height 1.59m, weight 89kg, ASA II, was admitted with fracture of theright hipwith the following exams (Hm=3,960,000, Hb=10.2 g/L e Ht=37). Radiographs showed a fracture at the right proximal femur reduction with Richards osteosynthesis is indicated, performed two days after admission. She had no history of hypertension, hyperlipidemia, diabetes, and cardiac arrhythmia. We obtained informed consent and discussed throughout the anesthetic technique with the patient and family. Tests revealed all electrolytes normal. Bilirubin, urea, creatinine unchanged. Total protein 6.9 g/dL. Chest X-ray and ECG were normal. Heart rate of 73 bpm and blood pressure of 148/64 mmHg.
In the bedroom the access to the anterior lumbar plexus, for analgesia and imaging tests, was achieved using a stimulator connected to a 50-mm, and the quadriceps was stimulated with a 0.5 mA current until a response was observed. After negative aspiration of blood, 20 mL of 0.5% bupivacaine and 20 mL of 2% lidocaine plus epinephrine 1:200.000 were injected through the extension connector of the needle.
The next day, before induction of spinal anesthesia, routine monitoring (electrocardiogram, pulse oximetry, and noninvasive blood pressure measurement) was started and an intravenous line was placed. Intraoperatively, 4 mL/kg of crystalloids and 500 mL of 6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride solution were administered intravenously. After sedation with ketamin (7.5mg) and midazolam (0.5mg) intravenously and cleaning the skin with70% alcoholspinal puncturewasperformed with the patient in the lateral decubitus, by the paramedian linein the L3-L4 inter spaces using 25G Quincke needle. After appearance of cerebrospinal fluid (CSF) 10 mg of 0.5% isobaric bupivacaine were administered at a speed of 1 mL 15s-1. Patients were immediately placed in the supine position to the beginning of surgery. The level of sensory block was observed in T11 and motor blockade (grade 3) of the lower limbs. During the insertion of the material, there was a distal fracture of the femur, with a surgical forecast of another 3 hours. At this point, I decided to go under the orthopedic table (Figure 1) and perform a new lumbar puncture with a 25G needle and injection of 15 mg of 0.5% isobaric bupivacaine (Video 1).Total 25 mg of 0.5% isobaric bupivacaine.The surgical procedure lasted 5 hours without hypotension, bradycardia, or decreased oxygen saturation. At the end of the surgery, a new lumbar plexus block via the inguinal route with neurostimulator aid and injection of 40 ml of 0.25% bupivacaine for analgesia, which lasted 22 hours, was performed. Full recovery from motor blockade of the lower limbs occurred 1:45h after injection of local anesthetic. First analgesic dose was performedat end of surgery in the operating room, tenoxican (20mg) and dipyrone (3g) were administered intravenously, the patient being sent to her room. The patient was discharged on the morning of the second day was sent to her residence.
Case 2
After written informed consent for anesthesia and publication,a man patient 80 years old, height 1.73m, weight 65 kg, ASA II, scheduled for a surgery of his left hip presented with blood test (Hm = 4,030,000, Hb = 11,8 g/L e Ht = 38,7%). We obtained informed consent and discussed the anesthetic technique with the patient and family. His clinical history revealed arterial hypertension and use of tobacco. At physical evaluation she exhibited a holosystolic blow (1+/4+) in the aortic and mitral focus. The echocardiogram revealed mild abnormalities. The electrocardiogram (ECG) revealed sinus bradycardia. Other exams as clotting time, renal function, liver function was within normal range. There was no history of allergy to any drug. In the bedroom the access to the anterior lumbar plexus, for analgesia and imaging tests, was achieved using a stimulator connected to a 50-mm, and the quadriceps was stimulated with a 0.5 mA current until a response was observed. After negative aspiration of blood, 20 mL of 0.5% bupivacaine and 20 mL of 2% lidocaine plus epinephrine 1:200.000 were injected through the extension connector of the needle.
The next day, in the operating room, he was continuously monitored with ECG (CM5), noninvasive blood pressure equipment (PANI) and peripheral oxygen saturation (SpO2). A peripheral vein was accessed through an 18G Teflon catheter in the right arm to provide medication and hydration with crystalloid (4 mL/kg) and 500mL of 6% hydroxyethyl starch (130/0,4) in sodium chloride at 0.9%.
After sedation with midazolam (0.5 mg) and ketamine (6 mg) intravenously, the patient was in lateral decubitus for the block. The skin was prepared with 70% alcohol and the punction was placed paramedially in the L3-L4 interspace with a 27G Quincke needle. After the appearance of liquor (CSF), 10 mg of isobaric bupivacaine 0.5% were administered at a speed of 1 mL.15s-1. The patient was immediately placed recumbent for the beginning of the surgery. The sensory block level reached T10. During the insertion of the material, there was a distal fracture of the femur, with a surgical forecast of another 3.30 hours.At this point, I decided to go under the orthopedic table (Figure 1) and perform a new lumbar puncture with a 27G Quincke needle and injection of 15 mg of 0.5% isobaric bupivacaine (Video 2).Total 25 mg of 0.5% isobaric bupivacaine.
The procedure lasted 5.30 hours, without hypotension, bradycardia, or hypoxia. At the end of the surgery, a new lumbar plexus block via the inguinal route with neurostimulator aid and injection of 40 ml of 0.25% bupivacaine for analgesia, which lasted 20 hours, was performed.The patient was conducted to his infirmary, fully conscious, oriented, and preserved vital signs. The patient was discarded home in the morning of the second day postoperatively, aware, oriented, and painfree.
Discussion
These two case reports demonstrate that with an old type of orthopedic table, there is the possibility of accessing the subarachnoid space posteriorly from under the table with Quincke needles and injection of isobaric solution of bupivacaine to complement the spinal anesthesia because it has distal fracture of the femur occurred when performing osteosynthesis of the hip.
In a recent article, we showed that spinal anesthesia is much more than the injection of hyperbaric solution in the sitting position [3]. In this article we describe all the possibilities of performing spinal anesthesia in different positions, different techniques, different indications that are not often used, continuous techniques and baricity of the different solutions. However, we do not describe a technique that few have the possibility to use, as described in these two cases, with two videos explaining the approach to the subarachnoid space in the posterior region under the orthopedic table.
Spinal anesthesia can safely provide excellent operating conditions for orthopedic surgery for lower limbs. For orthopedic lower limb surgeries, intrathecal 0.5% bupivacaine isobaric has predominantly been used in doses ranging from 7.5 mg to 15 mg [6]. A review of over 2,000 bupivacaine spinal anesthetics in one setting revealed a mean dose of 14 mg was utilized [7]. The 20 mg dose of bupivacaine is often used in daily hospital teaching practice, comparing isobaric and hyperbaric bupivacaine during lower abdomen surgery, when the duration of surgery is unpredictable [8]. Concluding that the isobaric producedmore rapid onset and longer duration when compared to hyperbaric bupivacaine, with comparable adverse effects.
Many types of anesthesia can be used for orthopaedic procedures. The type of anesthesia chosen depends on the nature and duration of the surgery, the patient’s health and medical conditions and the preferences of the patient, surgeon and anesthesiologist. Spinal anesthesia is chosen for hip or lower extremity surgery. The choice of anesthesia type for orthopedic surgery significantly influences perioperative outcome [9]. In elderly patients with femoral fractures, spinal anesthesia is commonly used for surgical anesthesia while peripheralnerve blocks are often used for postoperative analgesia [10-12]. In both cases, I performed inguinal lumbar plexus block with neurostimulator and local anesthetic at the patient's admission for radiological examinations and preventive analgesia. The day after release, spinal anesthesia was performed with 10 mg and subsequent new spinal anesthesia with 15 mg of 0.5% isobaric bupivacaine. At the end of the surgery, a new inguinal lumbar plexus block for postoperative analgesia.
Consulting websites about all orthopedic table catalogs for surgery, we found that all these new tables do not allow this possibility of space between the back and buttocks, for further entry into the subarachnoid space [13]. Thus, this new approach to the subarachnoid space via the posterior approach and under the orthopedic surgery table can only be used again in new orthopedic table designs.
Conclusion
The use of a total of 25 mg of 0.5% isobaric bupivacaine was justified by the increase in surgery time due to the distal fracture of the femur in both patients, and by the possibility of performing a puncture between the back and the buttocks, to avoid the use of general anesthesia. In the conditions of both patients, spinal anesthesia with posterior puncture of the subarachnoid space under the table caused by an accident during the surgical procedure, transforming a simple surgery into a long-term complex surgery, with excellent cardiocirculatory stability and without adverse events.These two cases showed that, knowing all the puncture positions, much more can be done than most anesthesiologists know.
Financial Support: No.
Conflict of Interest: No.
Contribution: No
References
- Imbelloni LE. Spinal hemianesthesia: Unilateral and posterior. Anesth Essays Res. 2014; 8: 270-276.
- Imbelloni LE, Pistarino MA, Miranda MG et al. Posterior spinal anesthesia for orthopedic, anorectic and plastic surgeries in prone position: It should be used more. Int J Anaesth Res. 2020; 3(3): 125-134.
- Imbelloni LE, Gouveia MA, Ghorayeb NM, Lemos Neto SV. Spinal anesthesia: Much more than single shot of hyperbaricbupivacaine. Int J Anesthetic Anesthesiol. 2021; 8 (1): 122. [DOI: 10.23937/2377-4630/1410122].
- Povey HM, Albrecht Olsen P, Pihl H, Jacobsen J. High dose spinal anaesthesia with glucose free 0.5% bupivacaine 25 and 30 mg. Acta Anaesthesiol Scand. 1995; 39: 457-461.
- Imbelloni LE, Costa EG, Lara R. High dose spinal anesthesia with glucose free 0.5% bupivacaine for ipsilateral fracture of the femur and tíbia. World J Pharm Pharm Sciences. 2018; 7(2): 1087-1094.
- Imbelloni LE, Braga RL, Morais Filho GB, Silva A. Low dose of isobaric bupivacaine provides lower incidence of spinal hypotension for hip surgery in elderly patients. Anaesth Pain & Intensive Care. 2014; 18(1): 17-20.
- Horlocker TT, Mc Gregor DG, Matsushige DK, Schroeder DR, Besse JA. A retrospective review of 4,767 consecutive spinal anesthetics: central nervous system complications. Anesth Analg. 1977; 84: 578-84.
- Helmi M, Uyun Y, Suwondo BS, Widodo U. Comparison of intrathecal use of isobaric and hyperbaricbupivacaine during lower abdomen surgery. Journal of Anesthesiology. 2014; 4. [DOI: org/10.1155/2014/141324].
- Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic care for orthopedic patients is there a potential for differences in care? Anesthesiology. 2016; 124: 608-623.
- Imbelloni LE, Gomes D, Braga RL, Morais Filho GB, da Silva A. Clinical strategies to accelerate recovery after surgery orthopedic femur in elderly patients. Anesth Essays Res. 2014; 8: 156-161.
- Imbelloni LE, de Morais Filho GB. Attitudes, awareness and barriers regarding evidence-basedorthopedic surgery between health professionals from aBrazilian Public Health System (SUS) hospital: Study of 400patients. Anesth Essays Res. 2016; 10: 546-551.
- Imbelloni LE, Teixeira DMP, Lima U, Miranda Jr MG, Soares ARA, Morais Filho GB. Are we ready for hip fracture geriatric patients? Study with 224 patients of the fourth age. Orthop & Spo Med Op Acc J. 2019; 3(2): 247-254.
- Websites consulted about orthopedic surgical tables.
https://saisurgicals.com/products-orthopaedics-surgical-tables
https://www.made-in-china.com/new-products/surgery-orthopedic-table_2.html
https://www.mizuhosi.com/product/hana
https://www.hillrom.com/en/products/ortho-table
https://www.magnatekenterprises.com/orthopaedics-surgical-tables

