Review Article - Volume 2 - Issue 6
Social theories of mental illness and its relevance in prevention of psychiatric disorder
Saroj Rajoo
Consultant Psychiatrist at Brain Care neuropsychiatry center, Nabha, Patiala, Punjab 147201, India
Received Date : Sep 30, 2022
Accepted Date : Nov 10, 2022
Published Date: Dec 03, 2022
Copyright:© Rajoo Saroj 2022
*Corresponding Author : Rajoo Saroj, Consultant Psychiatrist at Brain
Care neuropsychiatry center, Nabha, Patiala, Punjab 147201, India.
Email: dr.rajoosaroj@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1312
Abstract
Sociological concept of mental illness is based on assumption that outer environment is directly connected with inner psyche of individuals. Any change in outer environment directly affects the people’s psychological milieu by changing itself. Hence destabilize the environment-psyche ecosystem. Sociological theories play a pivotal role in genesis and management of psychiatric disorders. These theories provide the basic framework for treatment and prevention of mental illness. These theories are foundation for various governments and non-government based preventive programmes for mental illness. Overall, there is need of better understanding of sociological theories and its implication in current day practice for prevention and management of mental disorder.
Keywords: Mental illness; Prevention; National strategies.
Introduction
The six schools of theories (psychodynamic, behavioral, cognitive, social, existential and biological) forms the foundation of current day practice for prevention and management of mental disorder [1]. In sociology, mental illness is a deviant behaviour resulted from problem in thoughts, feelings and cognition which is not appropriate for surrounding environment. The positive aspect of such model is that it is based on cultural/social context but the negative aspect is that such approach leads to generalization which is often not the case, as individuals vary from one another in many aspects [2]. However it creates a window for intervention in society to prevent genesis of mental disorder in large number of individual living in that society. Sociological theories widens the concept of mental disorder to include the conditions of life, individuality, structure of power and dominance in a society, government policies for resource allocation [3]. Thus, research in the sociology of mental health is essential for grounding, refining, challenging, or modifying the conceptions of social theorists.
The important sociological theories, which have revolutionary effects in defining mental disorder, are functionalism theory, interpersonal theory, attachment theory, and stress theory, labeling theory, social class, migration and urbanization. According to functionalism theory all elements of a society forms a well-defined ecosystem, any change in one element, destabilizes the whole ecosystem, and then society alter itself to re-stabilize the ecosystem. However, if society changes too fast, it become impossible to re-stabilize the ecosystem and then it enters in to anomie or normlessness, which weakens its collective conscience and create anomic society [2,4]. The individual start feeling alienation (feeling of powerless, meaningless, normless, isolated and self-estranged) i.e. person does not feel that he is a part of the whole societal ecosystem [5]. The alienated person is "empty and depressed" [6]. The Interpersonal Theory is principally based on needs (needs for satisfaction and security) and anxiety. Anxiety occurs when fundamental needs are in danger of not being met. According to this theory needs acts as primary motivator of human behavior. That is also the major set-back for this theory because this theory ignores instinctual life and its role in development of child completely [7]. He believed that infant biological needs evoke tenderness in mother. Her tender gratification of infantile urges brings about relief of tension and feeling of security, which helps in building the self-esteem of child. If anxiety interferes with tenderness in mother, this anxiety imparted directly in to children leading to insecurity, low self-esteem and increased vulnerability to mental illness [7]. He regards anxiety as purely psychogenic and quite mystic in origin, the outcome of child’s first interpersonal relationship.
Attachment Theory: According to this theory, human instinct forms a strong and persistent affectional attachment bond with other objects. Loss of such affectional attachment bonds causes development of intense anxiety, restlessness as a behavioral change in individual. This behaviour tries to recoup the lost attachment bond and relationship with object. According to this theory the infant-mother attachment bond is prototype of such attachment bond. There are 4 types of attachment bonds, Secure- The individual is able to give and receive care. The care is provided, when needed, Anxious- ambivalent-Individuals are never sure that their attachment needs will be met; believe that care must be sought constantly, Anxious -Resistant: attachment needs are provided but individual reject it, Anxious-avoidant- the individual behaves as if other will never provide care, when needed. The quality of attachment bond in childhood, influence though, feeling, behavior and shapes the cognitive and emotional development in adults. It has been observed that series of disorganized attachment interaction along developmental path of children increases risk of developing borderline personality disorder [8] and eating disorder [9]. Research on attachment theory required to understand the mechanism of development of psychiatric disorder due to disorganized attachment bonding.
Stress theory: The “nonspecific response of body to any demand caused by either pleasant or unpleasant condition”. Stress has direct relation with either genesis and prognosis of mental disorder [10,11,12]. There is enough evidence that stress has epigenetic effect i.e. it affect DNA methylation (expression of genes) resulting in increased chances of developing psychiatric disorder [13]. It provide direct link of sociological theory with biological theory of mental disorder. According to Labeling theory people, who are labeled as deviant, treated as deviant eventually become deviant. Socioeconomic condition play a significant role in labeling as deviant because people with higher socio-economic status have higher control over society. People with deviant behaviour are blocked to access normal life and needs. Furthermore these individuals develop secondary deviance, become socialized to mental- patient culture and continue to live with abnormal behavior [14]. Bruce Link in 1987 proposed modified labeling theory, which state that stigmatised individuals recognise the negative label applied on them have projected their role in society as less intelligent, trust worthy and more dangerous and incompetent. This type of thinking decreases their self-esteem and self-efficacy and eventually restricts them from social participation. People with mental disorder are generally labeled as deviant, unpredictable, violent, disruptive, dangerous and incurable. This theory sensitizes mental health professional about stigma of mental illness and danger of institutionalization. Social class-this theory gave the special importance to social class are social causation hypothesis and social drift hypothesis. According to Social causation hypothesis, the prevalence of mental illness is higher in lower socioeconomic status group due higher psychological stress produced by environmental adversity (such as unemployment and poverty, social disadvantage, homelessness). According to Social drift hypothesis, person with mental illness of those who have trait that predisposes to mental illness drift down in to or unable to rise from lower socioeconomic status [18,19]. Migration-Migration is a universal phenomenon, which existed with the subsistence of the human beings on earth. People migrate from one place to another for several reasons, but the goal or main reason behind changing the residence would be improving their living conditions or to escape from debts and poverty. Several factors like language barriers, concerns about legal status, difficulties related to acculturation, racism, isolation, housing, and health problems leads increases the risk of mental health problems after settlement in host countries. Studies have reported that around 24% of migrant women in cities are mentally unhealthy and around 50 % migrant population develops at least one psychiatric symptoms [20,21]. Migrant population have found increased rates of schizophrenia, depression, anxiety disorders, and other psychiatric disorders than general population. The increased frequency of mental disorders in migrants can be explained due to development of sense of insecurity, low self‑esteem, non-availability of member of their own community changing concepts of self, their role in society, and mismatch between aspiration and achievements [22]. Urbanization-Urbanization, defined as the increase in the number of cities, urban population and industrialization, is not only a demographic movement but also includes, social, economic and psychological changes that constitute the demographic movement. Urbanization is promotes individualism, weakens the collective conscience of society. Urbanization affects mental health through the influence of increased stressors and factors such as overcrowded and polluted environment, high levels of violence, and reduced social support [23]. This is responsible for increase in frequency of mental disorder such as psychoses, depression, substance abuse, crime, delinquency, vandalism, family disintegration. There are studies, which have shown the direct association of urbanization and increase in prevalence of schizophrenia [24,25].
Prevention for mental disorder
This paper will provide a brief review of primary prevention for various psychiatric disorders. Primary prevention includes universal, selective and indicated prevention. Universal prevention focus whole population irrespective of risk factors, Selective prevention focus on a subgroup of population with increased risk for mental disorder as evidenced by biological and psychosocial factor and Indicated prevention targets people with detectable sign and symptoms of mental disorder.
Addressing risk and protective factors for mental disorder: Risk factors are associated with an increased probability of onset, greater severity or longer duration of major psychiatric problems. Protective factors refer to conditions that strengthen the people against those factors, which are associated with increased risk of mental disorder and also ameliorate or modify the course of mental illness [26].
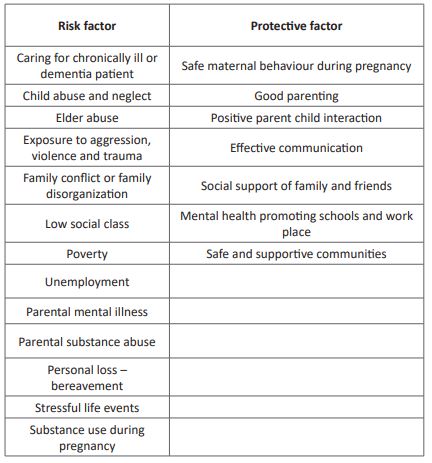
The cumulative effects of presence of risk factor and absence of protective factor predisposes individuals to move from a healthy mental state to a psychological problem and finally to a full-blown mental disorder [27]. These risk and protective factors forms the backbone of prevention program and help in development of national policies, legislation and resource allocation and sociological intervention to reduce stress and enhance resilience.
Universal Prevention
National policies, legislation and resource allocation in any country or region affect significantly in prevention of mental disorder. There is strong evidence that improving nutrition and socioeconomic empowerment in underprivileged society leads to better cognitive development, improved educational outcome, and reduced risk of mental disorder. For a healthy and sustainable society, it is responsibility of government to ensure financial security, health security, social equality and better housing condition to its citizen [28]. In India, to achieve these goals the government has started PMJDY (Pradhan mantra Jandhan Yojana) to ensure financial security, ABPMJAY (Ayushman Bharat Pradhan Mantri Jan Arogya Yojana) to ensure health security, (MDM) Mid-day meal programme to ensure food security and social equality in school aged children and PMAY (Pradhan Mantri Awas Yojana) to ensure better housing. Pradhan Mantri Jan Dhan Yojana (PMJDY): its national mission for financial inclusion to ensure access to financial services, namely, a basic savings & deposit accounts, remittance, credit, insurance, pension in an affordable manner. Under the scheme, a basic savings bank deposit (BSBD) account can be opened in any bank branch or business correspondent (Bank Mitra) outlet, by persons not having any other such account. There is no requirement to maintain minimum balance in PMJDY account, an overdraft facility of Rs. 10,000 is available for one account holder, preferably lady of the household. Around 4 per cent of interest per annum can be earned on deposits in PMJDY account. On accident insurance cover of rs.2 lakh is available with Rupay card issued to the PMJDY account holders along with life insurance cover of around 30000 rupees [30].
Government of India, was launched as recommended by the National Health Policy 2017, to achieve the vision of universal health coverage. This initiative has been designed provide health care facilities to everyone with a commitment “leave no one behind”. It covers the bottom 40 percent of poor and vulnerable population. The inclusion of households is based on the deprivation and occupational criteria of the socio-economic caste census 2011 (SECC 2011) for rural and urban areas, respectively. This number also includes families that were covered in the RSBY (Rastriyasuraksha bema yojana). Free treatment can be availed in all public and private hospitals (listed by government) in times of need and whole process is paperless and cashless. No limit on the age and size of the family. Scheme covers all pre-existing conditions from the time the scheme comes into force and the insurance covers pre and post-hospitalization expenses [31].
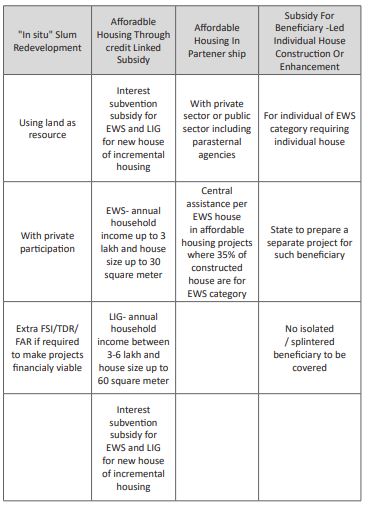
Pradhan Mantri Awas Yojana (PMAY): In India, although multiple programs has been launched in past to tackle the housing problem but recently it has been observed that rapid growth of urban population has led to acute shortage of housing and increase in slums in urban area and increased prevalence mental disorder simultaneously [32]. The government of India has declared the mission of “Home for All” by 2022 and launched a comprehensive mission “Pradhan Mantri Awas Yojana-Housing for All (Urban)”. The mission seeks to address the housing requirement of urban poor including slum dwellers [32].This program provide subsidized loan to construct pucca house in urban area for those, who doesn’t hold a pucca house and have not availed any of similar scheme from government of India. PMAY consists of four pillars, as can be seen in the graphic below [33].
Source: MoHUPA 2015
Preference under the Scheme, subject to beneficiaries being from EWS/LIG segments, should be given to Manual Scavengers, Women (with overriding preference to widows), persons belonging to Scheduled Castes/Scheduled Tribes/Other Backward Classes, Minorities, Persons with disabilities and Transgender [37].
Mid-day meal programme: Poor nutritional support during childhood may lead to malnutrition, growth retardation, reduced work capacity and poor mental and social development [35]. The Mid-Day Meal programme (MDM) was started as nutritional support program for disadvantage group of school aged children. It has multidimensional effects, such as satisfying class hunger, increase in enrollment rate, class attendance and also increases social equality as all children in school has to take feed together. However, there are some reports that it has not implemented properly in some places due to cast discrimination. On 15th august 1995, it was universalized nationwide by the Government of India to ensure the prosperity of nation(http://mdm.nic.in/mdm_website/).
Mahatma Gandhi National Rural Employment Guaranty Act: Although complex but there is fairly strong association between unemployment and suicide rate. Unemployment may drive up the suicide risk through factors such as poverty, social deprivation, domestic difficulties, and hopelessness. Furthermore person with psychiatric disorder are at more risk of unemployment [41,42]. According to NCRB data 2019, suicide rate in Indian is highest among housewives, farmer, private sector employee and students. This programme offers guaranteed 100 day employment for rural Indian. It is largest social protection program in world covering around 50 million rural households. It ensures that workers get paid timely and payment is made directly in their bank account. It has been reported that it has significantly reduced the stress in underprivileged society of India [38]. The Act was ambitious in intention and objectives. It promises the employment on demand, livelihood security, and empowerment of marginalized population along with deepening of democracy. However despite great efforts by Indian government the achievement couldn’t meet its objective due to endemic [43].
Selective prevention: Targeting vulnerable populations to decrease stressors and to enhance resilience can be effective in preventing mental and behavioral disorders. Infancy, childhood and adolescence-Parental training: In Indian school, parents are called up for parent - teacher meeting frequently. It provides great opportunity to educate parents about application of contingency management, positive and negative reward/punishment in behaviour modification of child. Parents are advised to improve the positive involvement with child, enhanced communication, parental attention, and praise for good behaviour. It may improves the parent child emotional bond and hence the sense of security in child [44,45].
Children of family with mental disorder: Mental illness in parents is usually associated with adverse family environment, high stress reactivity, frequent violence, alienation in society and reverse care giving “parentification” [48]. The children of parents with mental disorder are at risk of developing affective dysregulation, behavioral problem and poor adaptive functioning. Carefully designed intervention to enhance the coping ability and resilience in these children protect them from developing mental disorder [49]. Also the school based program targets children undergoing specific type of stressful situation or suffering any specific cognitive and behavioral problem to enhance coping assets and strategies, are very effective in prevention of development of mental disorder [50,51,52]. Adults-Work stress and unemployment, stressful life events (separation, divorce, death of spouse or any other relative etc.) are major risk factor for increase in the incidence of depression, anxiety, burn-out, alcohol-related problems, cardiovascular illness and suicidal behaviour in adults. Such high risk adults are targeted to either increase the coping strength by changing or eliminating the stressful demand on themselves or by altering the perception and reaction to stressful demand. It is advised to change the stressful environment if nothing works. There are few strategies for improving the work environment. (1)Task and technical intervention such as Job enrichment, ergonomic improvement, reduction of noise, lowering of workload (2) Improving role clarity and social relationship such as communication and conflict resolution however the most intervention worldwide focuses on reduction in cognitive appraisal of stress and its subsequent effect rather than reducing or eliminating stressor [53].
Burden of Caregiver- Caregivers of chronically ill patients or elderly are at increased risk of suffering from high levels of stress and hence at risk to various mental disorder (such as depression, anxiety disorder). The psycho educational intervention addressing detailed information about illness of patient, treatment, available resources and services that can help in care of patients and training of caregiver to handle the disease specific problem helps in reducing the stress of care giver. It also improves the subjective well-being and perceived caregiver satisfaction [54].
Geriatric population-The geriatric population is nonproductive and socially marginalized especially in Indian society. The lack of social support leads to significantly higher stress and immense suffering if they develop chronic illnesses like (diabetes mellitus, Hypertension, Dementia etc.) and loss of visual and auditory senses [55]. It has been observed that the various interventions such as Yoga, aerobic exercise, participating in fun activities (e.g. playing cricket, badminton, recycling household waste material, gardening etc.) are very helpful in improving the both mental and physical health. Also the training of caregiver about elderly age problem and its management such as early screening and intervention for diabetes, hypertension, and hypercholesterolemia, dementia at frequent interval, providing hearing add in elderly people with hearing loss is very helpful in reducing the various psychiatric morbidity [56]. The study, published in lancet psychiatry in 2020, suggest that the prevalence of mental disorders with onset in childhood and adolescence decreased in India from 1990 to 2017, however the contrary to this prevalence of mental disorders that manifest predominantly during adulthood increased during this period [57].
Indicated prevention: Along with treatment for mental disorder, patients are encouraged to incorporate yoga and relaxation exercise, increased social participation, increase problem solving capability to strengthen coping ability and self-efficacy. Person with severe mental disorder are provided certificate of disability and some financial benefit as per Indian disability evaluation and assessment score. It reduces the morbidity associated with mental disorder.
Conclusion
The mental illnesses are not purely biological, purely psychological or purely social but it is consequences of abnormal interaction among these 3 key factors.Mental disorder is outcome of interplay among biological, psychological and social factor but its genesis is chiefly dependent on psychological and social factor. Biological (Genetic) factor is very important in determining the severity of mental disorder but it rarely determines the behaviour outcome. The social analyses of health and illness drew attention to the need for restructuring the economic policies and resources allocation of society for efficient prevention of mental disorder. However more research and amendment in economic policies needed to design the more effective program for prevention of mental disorder and to enhance the prosperity in society.
Funding: There is no source of funding for study.
Conflict of interest: There is no conflict of interest.
References
- Avasthi A. Are social theories still relevant in current psychiatric practice. Indian J SocPsychiatr. 2016; 32: 3-9.
- Horwitz AV. The sociological study of mental illness: a critique and sythesis of four perspectives. In: Aneshensel CS, Phelan JC (eds) Handbook of the sociology of mental health. Plenum, New York. 1999; 57-78
- Branaman A. Contemporary social theory and the sociological study of mental health. In Mental Health, Social Mirror. Avison W, McLeod J, Pescosolido B, eds. New York, NY. 2007; 95-126.
- Wirth-Cauchon J, Horwitz A. Creating Mental Illness. Contemporary Sociology. 2002; 31: 785.
- Channabasavanna S & Bhatti R. Student perception of anomie. Indian J Psychiatry. 1977; 19: 17-23.
- Seeman M. "On the meaning of alienation." Amer. Soc. Rev. 1959; 783-790.
- Jacobson E. Sullivan’s Interpersonal Theory of Psychiatry. Journal of the American Psychoanalytic Association. 1995; 3(1): 149-156.
- Levy KN. The implications of attachment theory and research for understanding borderline personality disorder. Development and psychopathology. 2005; 17(4): 959-86.
- Tasca GA, Ritchie K, & Balfour L. Implications of attachment theory and research for the assessment and treatment of eating disorders. Psychotherapy (Chicago, Ill.). 2011; 48(3): 249-259.
- Duman RS. Pathophysiology of depression: the concept of synaptic plasticity. European psychiatry : the journal of the Association of European Psychiatrists. 2002; 17(3): 306-310.
- Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. The American journal of psychiatry. 1992; 149(8): 999-1010.
- Zubin J & Spring B. Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology. 1977; 86(2): 103-126.
- Klengel T, Pape J, Binder EB & Mehta D. The role of DNA methylation in stress-related psychiatric disorders. Neuropharmacology. 2014; 80: 115-132.
- Wright ER, Gronfein WP & Owens TJ. Deinstitutionalization, social rejection, and the self-esteem of former mental patients. Journal of health and social behavior. 2020; 41(1): 68-90.
- Bryan S. Turner. Medical Power and Social Knowledge, Sage Publications, Newbury Park, CA, 1995.
- Daumerie N, VasseurBacle S, Giordana JY, Bourdais Mannone C, et al. Premiers résultatsfrançais de l'étude INDIGO [Discrimination perceived by people with a diagnosis of schizophrenic disorders. INternational study of DIscrimination and stiGma Outcomes (INDIGO): French results]. L'Encephale. 2012; 38(3): 224-231.
- Dohrenwend BP. Socioeconomic status (SES) and psychiatric disorders. Are the issues still compelling?. Social psychiatry and psychiatric epidemiology. 1990; 25(1): 41-47.
- Wadsworth ME & Achenbach TM. Explaining the link between low socioeconomic status and psychopathology: testing two mechanisms of the social causation hypothesis. Journal of consulting and clinical psychology. 2005; 73(6): 1146-1153.
- Perry MJ. The relationship between social class and mental disorder. The journal of primary prevention. 1996; 17(1): 17-30.
- He X & Wong DF. A comparison of female migrant workers' mental health in four cities in China. The International journal of social psychiatry. 2013; 59(2): 114-122.
- Adhikari R, Jampaklay A, Chamratrithirong A. Impact of children's migration on health and health care-seeking behavior of elderly left behind. BMC Public Health. 2011; 11: 143.
- Virupaksha HG, Kumar A & Nirmala BP. Migration and mental health: An interface. Journal of natural science, biology, and medicine. 2014; 5(2): 233-239.
- Srivastava K. Urbanization and mental health. Industrial psychiatry journal. 2009; 18(2): 75-76.
- Kelly BD, O Callaghan E, Waddington JL, Feeney L, Browne S, Scully PJ, et al. Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophrenia research. 2010; 116(1): 75-89.
- Vassos E, Pedersen CB, Murray RM, Collier DA & Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophrenia bulletin. 2012; 38(6): 1118-1123.
- Joshi Mrunal & Rajpu rohit, Vikram. PradhanMantri Jan DhanYojana (the Financial Inclusion): A Study of Awareness. SSRN Electronic Journal. 2016. [DOI:10.2139/ssrn.2816493].
- Angell BJ, Prinja S, Gupt A, Jha V & Jan S. The Ayushman Bharat Pradhan Mantri Jan ArogyaYojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLoS medicine. 2019; 16(3): e1002759.
- Thomson H, Petticrew M, & Morrison D. Health effects of housing improvement: systematic review of intervention studies. BMJ (Clinical research ed.). 2001; 323(7306): 187-190.
- World Health Organization. A critical link: interventions for physical growth and child development. Geneva: World Health Organization. 1999.
- PS Ravindra, T Suguna, M Satyavathi, K Santosh Kumar, A Venkata Lakshmi. Does Pradhan Mantri Jan Dhan Yojana (PMJDY) Scheme Leads To Better Financial Inclusion Outcomes? An Investigation. Journal of Critical Reviews. 2020; 7 (15): 2728-2736.
- Angell BJ, Prinja S, Gupt A, Jha V, & Jan S. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLoS medicine. 2019; 16(3): e1002759.
- Ministry of Housing & Urban Poverty Alleviation (MoHUPA). Pradhan Mantri Awas Yojana; Housing for All (Urban)- Scheme Guidelines; Government of India. 2016.
- Puttkamer Laura von. India: Slum-free by 2022? A people-centered evaluation of the Pradhan Mantri Awas Yojana Scheme; Housing for All; Source: MoHUPA 2015. 2016.
- Ministry of Housing & Urban Poverty Alleviation (MoHUPA). Pradhan Mantri Awas Yojana (Urban)-Housing for All; Credit Linked Subsidy Scheme for EWS/LIG; Operational Guidelines; Government of India. 2017.
- Awasthi CP, Kumar S, Tiwari PP, & Singh AB. Nutritional status of pre-school and school children in rural area of Sultanpur district. Journal of Dairying Foods & Home Science. 2020; 19(1): 16-21.
- http://mdm.nic.in/mdm_website/
- https://nrega.nic.in/netnrega/home.aspx
- Van Hal G. The true cost of the economic crisis on psychological well-being: a review. Psychology research and behavior management. 2015; 8: 17-25.
- Pelzer B, Schaffrath S, &Vernaleken I. Coping with unemployment: the impact of unemployment on mental health, personality, and social interaction skills. Work (Reading, Mass.). 2014; 48(2): 289-295.
- Parmar D, Stavropoulou C, & Ioannidis JP. Health outcomes during the 2008 financial crisis in Europe: systematic literature review. BMJ (Clinical research ed.). 2016; 354: i4588.
- Herbig B, Dragano N, &Angerer P. Health in the long-term unemployed. DeutschesArzteblatt international. 2013; 110(23-24): 413-419.
- Agrawal GK. Mahatma Gandhi National Rural Employment Guarantee Act: Design Failure, Implementation Failure or Both? Management and Labour Studies. 2019; 44(4): 349-368.
- Farrington DP, Jolliffe D, Loeber R, Stouthamer-Loeber M, & Kalb LM. The concentration of offenders in families, and family criminality in the prediction of boys' delinquency. Journal of adolescence. 2001; 24(5): 579-596.
- Beauchaine TP, Webster-Stratton C, & Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: a latent growth curve analysis. Journal of consulting and clinical psychology. 2005; 73(3): 371-388.
- Kling A, Forster M, Sundell K, & Melin L. A randomized controlled effectiveness trial of parent management training with varying degrees of therapist support. Behavior therapy. 2010; 41(4): 530-542. https://doi.org/10.1016/j.beth.2010.02.004
- Ogden T, & Hagen KA. Treatment effectiveness of Parent Management Training in Norway: a randomized controlled trial of children with conduct problems. Journal of consulting and clinical psychology. 2008; 76(4): 607.
- Maybery D & Reupert AE. The number of parents who are patients attending adult psychiatric services. Current opinion in psychiatry. 2018; 31(4): 358-362.
- Murphy G, Peters K, Wilkes L & Jackson D. A Dynamic Cycle of Familial Mental Illness. Issues in mental health nursing. 2014; 35(12): 948-953.
- Wolchik SA, West SG, Sandler IN, Tein JY, Coatsworth D, et al. An experimental evaluation of theory-based mother and mother-child programs for children of divorce. Journal of consulting and clinical psychology. 2020; 68(5): 843-856.
- Sandler I, Gunn H, Mazza G, Tein JY, Wolchik S, Kim H, et al. Three perspectives on mental health problems of young adults and their parents at a 15-year follow-up of the family bereavement program. Journal of Consulting and Clinical Psychology. 2018; 86(10): 845–855.
- Caplan RD, Vinokur AD, Price RH & van Ryn M. Job seeking, reemployment, and mental health: a randomized field experiment in coping with job loss. The Journal of applied psychology. 1989; 74(5): 759-769
- Vinokur AD, Schul Y, Vuori J, & Price RH. Two years after a job loss: long-term impact of the JOBS program on reemployment and mental health. Journal of occupational health psychology. 2000; 5(1): 32-47.
- Vuori J, Silvonen J, Vinokur AD, & Price RH. The Työhön Job Search Program in Finland: benefits for the unemployed with risk of depression or discouragement. Journal of occupational health psychology. 2002; 7(1): 5-19
- Sörensen S, Pinquart M, & Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. The Gerontologist. 2002; 42(3): 356-372.
- Fuzhong Li, Terry E Duncan, Susan C Duncan, Edward McAuley, Nigel R Chaumeton, & Peter Harmer. Enhancing the Psychological Well-Being of Elderly Individuals Through Tai Chi Exercise: A Latent Growth Curve Analysis, Structural Equation Modeling: A Multidisciplinary Journal. 2001; 8(1): 53-83.
- Haight BK, Michel Y, & Hendrix S. The Extended Effects of the Life Review in Nursing Home Residents. The International Journal of Aging and Human Development. 2000; 50(2): 151-168.
- Sagar R, Dandona R, Gururaj G, Dhaliwal RS, Singh A, Ferrari A & Dandona L. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. The Lancet Psychiatry. 2020; 7(2): 148-161.

