Case Report - Volume 2 - Issue 6
Ovarian dysgerminoma with abdominal metastasis in a 6-year-old girl
Amarkak Abdillahi Wais*; Daoud Ali Mohamed; Madina Rabileh; Walid Mohamed; S El Haddad; N Allali;L Chat
Department of Radiology, Hospital of Specialty, CHU Ibn-Sina, Mohamed V University, Rabat Morocco.
Received Date : Oct 01, 2022
Accepted Date : Nov 11, 2022
Published Date: Dec 05, 2022
Copyright:© Amarkak Abdillahi Wais 2022
*Corresponding Author : Amarkak Abdillahi Wais, Department of Radiology, Hospital of Specialty, CHU Ibn-Sina, Mohamed V University, Rabat Morocco.
Email: amarkak.a.wais@gmail.com
DOI: Doi.org/10.55920/2771-019X/1313
Abstract
Malignant germ cell tumors of the ovary (OGCTs) are rare and represented less than 5% of all germ cell tumors of the ovary. GCTs are composed of several histological types and are divided into two groups: dysgerminomatous germinal malignancies and non-dysgerminomatous germinal malignancies. Ovarian dysgerminomas represented 33% of OGCTs. They can occur at any age but very often in children and adolescents, most often in the second and third decade, rarely in the first decade. The circumstances of discovery are acute abdominal pain, abdominal distension with palpable mass, sometimes we observe menstrual disorders and endocrinological disorders. Imaging findings, ovarian dysgerminoma is presented as a huge solid pelvic mass that can be confused with neuroblastoma which is very common in infants and children. Imaging features with tumor markers permits to confirm the ovarian origin. The Diagnosticof certainty is established by anatomopathological study. These tumors are characterized by a very high chemosensitivity with a better prognosis. We are reporting here a case of ovarian dysgerminoma with abdomino-pelvic metastasis in a 6-year-old girl.
Introduction
Solid tumors of gynecological origin in children are rare and represent less than 5%. Ovarian germ cell tumors (OGCTs) are the most frequent. They represent 95% of benign tumors (dermoid cysts) and 5% of malignant tumors.The dysgerminomas represent 33% of all GCTs. They are fast growing neoplasm’s. They can occur at any age but very frequently in children and adolescents, most often in the second and third decade, rarely in the first decade. The circumstances of discovery are acute abdominal pain, abdominal distension with palpable mass, sometimes we observe menstrual disorders and endocrinological disorders.Imaging findings, ovarian dysgerminoma is presented as a huge solid pelvic mass that can be confused with neuroblastoma which is very common in infants and children. Imaging features with tumor markers permits to confirm the ovarian origin. The Diagnosticcertainty is established by anatomopathological study. These tumors are characterized by a very high chemosensitivity with a better prognosis.
Case Report
We are reporting a case of a 6-year-old girl, with no pathological history, consulting for abdominal pain evolving since a week. Who underwent an abdomino-pelvic ultrasound showed a right latero-vesicalsolid pelvic mass, lobulated, well-limited, echogenic, discretely heterogeneous, Doppler-vascularized and a retroperitoneal median mass, discretely hypoechogenic, well-limited, without Doppler-vascularized. Later, completed by abdominal-pelvic CT scan without and with contrast injection, showed a right latero-vesical solid mass, encapsulated, multi-lobulated, iso-dense compared to the muscle, enhanced after injection, without vascular pedicle twist. There was also abdomino-pelvic adenopathy, the largest one was a median retroperitoneal adenopathy, discreetly hypodense, strongly enhanced in the periphery and coming into contact with the inferior vena cava (IVC) responsible of a thrombosis. A malignant ovarian mass or a neuroblastoma has been mentioned. To better characterize, an MRI was performed showing a right ovary enlarges, multi-lobulated, iso-intensein T1 and T2-weighted sequences, heterogeneous with hyperintensity on diffusion-weighted sequences, enhanced after injection of gadolinium measuring 73x51 mm with necrotic abdominal adenopathy including a median retroperitoneal with thrombosis of the IVC. The morphology and size of the uterus and left ovary were normal. Biological investigations: BhCG=3.7 mul/ml, alpha fetoprotein (AFP) =0.52ng/ml, the rest of the biological investigations were normal. The patient was operated by laparotomy for exploration and surgical excision. Intraoperatively, an excision of the right ovarian mass was performed with biopsy of the left latero-aortic adenopathy. The anatomopathological study concluded to a pure ovarian dysgerminoma with retro peritoneal metastases classified stage III C according to revised FIGO staging of ovarian cancer 2014(Chest CT scan was normal).
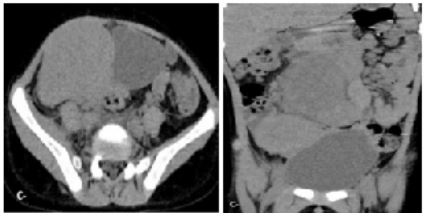
Figure 1: CT-scan axial and coronal view with non-contrast injection showing: Right latero-vesical solid mass, encapsulated, multi-lobulated, iso-dense.
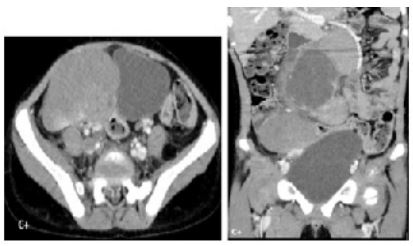
Figure 2: CT-scan axial and coronal view with injection showing: right latero-vesical solid mass, encapsulated, multi-lobulated, iso-dense enhanced after injection of the mass.

Figure 3: CT-scan coronal view after contrast injection showing: The thrombosis of the IVC and right iliac vein.

Figure 4:Per-operative image confirmed the right ovarian mass.
Discussion
GCTs represent less than 5% of ovarian tumors withincidence rate of 0.5/100,000 women. GCTs are composed of several histological types and are divided into two groups: dysgerminomatous germinal malignancies and non-dysgerminomatous germinal malignanciescomposed of vitelline tumors, embryonal carcinomas, pure choriocarcinomas, immature teratomas and composite tumors. Ovarian dysgerminomas count33% of all GCTs.Ovarian dysgerminoma occurs most often in the second and third decade of life. It rarely occurs in the first decade. It is located mainly in the right ovary. A study by Santesson L reported that the tumor was located on the right in 51% of cases, on the left in 32% andbilaterally 17% of cases. More recently, Shuhui Zhao and al reported that in 75% of cases, the tumor was located on the right, in 16.7% on the left and 8.3% bilaterally [REF]. The circumstances of discovery are abdominal pain, abdominal distension with a palpable mass, endocrinological signs such as menstrual disorders or precocious puberty, sometimes of fortuitous discovery. [REF] (B fresneau ref, ref de cigdem kilic: ovarindy germinoma tertiary). Biologically, BhCG is low in 5-15% of cases when associated with a syncitiotrophoblasticelements. LDH is often high (95%) but non-specific. AFP is normal, never increased contrary to vitelline tumors. On imaging investigations, dysgerminoma presents as a solid mass, often voluminous, well encapsulated, multi-lobulated, purely solid or predominantly solid, containing inter-lobular septa characteristic of this tumor, sometimes with necrotic areas. These inter-lobular septa are seen as hypoechogenic trabeculae on ultrasound, which are strongly enhanced on CT scan with contrast injection and hypo-intensity T2-weigthed on MR. The study of Shuhui Zhao and alfound that the inter-lobular septa can be hypo-intensity T2-weighted and weakly enhanced on MR with contrast injection, depending on the degree of fibrous stromal edema and classified them into four groups (ref shuhui).In infants and children, the most common solid tumors are neuroblastomas and hematological cancers. Imaging findings, mainly MRI, can be used to determine the gynecological origin, particularly ovarian, and staging according to revised FIGO staging system in order to guide the therapeutic approach. The diagnosiscertainty is based on the histological results from the surgical parts obtained by surgical exploration. The anatomo-pathological study allows to confirm the diagnosis of ovarian dysgerminoma, and to specify if the dysgerminoma is pure, or associated with a syncitiotrophoblasticelements, or sometimes associated with a gonadal dysgenesis. The treatment consists of a conservative surgical excision in case of a pure dysgerminoma without metastasis.
Conclusion
Ovarian germ cell tumors (OGCTs) a very common malignant tumors in children and adolescent. The dysgerminomas represent 33% of all GCTs. Imaging features such as ultrasound, CT-scan and MR with tumor markers allow to confirm the ovarian origin. The Diagnosticcertainty is established by anatomopathological study. These tumors are characterized by a very high chemosensitivity with a better prognosis. The treatment of those tumors is mainly surgical.
References
- Duhil de Bénazé G, Pacquement H, Faure-Conter C, Patte C, Orbach D, et al. Paediatric dysgerminoma: Results of three consecutive French germ cell tumours clinical studies (TGM-85/90/95) with late effects study. Eur J Cancer. 2018; 91: 30-37.
- Zogbi L, Gonçalves CV, Tejada VF, Martins D, Karam F, Machado Dos Santos S, et al. Treatment of bilateral ovarian dysgerminoma with 11-year follow-up: A case report. Ann Med Surg (Lond). 2018; 33: 50-52.
- Madenci AL, Vandewalle RJ, Dieffenbach BV, Laufer MR, Boyd TK, et al. Multicenter pre-operative assessment of pediatric ovarian malignancy. J Pediatr Surg. 2019; 54(9): 1921-1925.
- Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Pediatric ovarian malignancy presenting as ovarian torsion: incidence and relevance. J Pediatr Surg. 2010; 45(1): 135-9.
- Lacour B, Guyot-Goubin A, Guissou S, Bellec S, De´sandes E, Clavel J. Incidence of childhood cancer in France: National Children Cancer Registries, 2000-2004. Eur J Cancer Prev. 2010; 19(3): 173-81.
- Terenziani M, Massimino M, Casanova M, Cefalo G, Ferrari A, Luksch R, et al. Childhood malignant ovarian germ cell tumors: amonoinstitutional experience. Gynecol Oncol. 2001; 81(3): 436-40.
- H Al Husaini, H Soudy, A El Din Darwish, M Ahmed, A Eltigani, ALM Mubarak, et al. Pure dysgerminoma of theovary: a single institutional experience of 65 patients, MMed. Oncol. 2012; 29: 2944-2948.
- W Xu, Y Li. Is Omentectomy Mandatory Among Early Stage (I, II) Malignantovarian germ cell tumor patients? A retrospective study of 223 cases, Int. J.Gynecol. Canc. 2017; 27: 1373-1378.
- Llueca Y. Maazouzi JL Herraiz, MC Medina, D Piquer, B Segarra, et al. Bassols, Treatment and follow-up in an asymptomatic malignantstruma ovarii: a case report, Int. J. Surg. Case Rep. 2017; 40: 113-115.
- NM Kamal, U Khan, S Mirza, K Mazoun, FM Mirza, M Jundi. Ovarian dysgerminoma with normal serum tumour markers presenting in a child with precocious puberty, J. Canc. Res. Therapeut. 2015; 11(3): 661.

