Clinical Image - Volume 2 - Issue 6
A hyperplastic growth of lip
Bhumika Gumber1; Vikender Singh Yadav2*; Kanika Makker2; Deepika Mishra3; Subramony hagavatheeswaran1
1Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak, India.
2Division of Periodontics, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India.
3Department of Oral Pathology and Microbiology, Centre for Dental Education and Research, All India Institute of Medical Sciences,New Delhi, India.
Received Date : Oct 01, 2022
Accepted Date : Nov 12, 2022
Published Date: Dec 06, 2022
Copyright:© Amarkak Abdillahi Wais 2022
*Corresponding Author : Vikender Singh Yadav, Associate Professor, Division of Periodontics, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India 110029.
Email: vikenderyadav@gmail.com
DOI: Doi.org/10.55920/2771-019X/1314
Case Report
A 25- year-old systemically healthy female patient reported with an aesthetic complaint due to a growth in the corner of right upper lip present for 2 months. Clinical examination revealed a solitary spherical-shaped bright red fibrous overgrowth measuring 4x4 mm involving the mucocutaneous line of upper lip (Figure 1A & B). On palpation, it was non tender, smooth in texture, and soft in consistency. Based on the signs and symptoms, a provisional diagnosis of fibroma was made with a differential diagnosis of pyogenic granuloma. After obtaining written informed consent, the lesion was excised in totowith 1 mm of healthy margin by performing two elliptical incisions (Figure 1C). The biopsied tissue was fixed in 10% formalin and sent for histopathological examination. Double-layered microsurgical suturing was done with 7-0 polyglactin suture (Figure 1D) followed by superficial suturing of the wound margins (Figure 1E). Postoperative instructions were given and analgesics were prescribed, as and when required. Healing was uneventful and sutures were removed at 10 days follow-up (Figure 1F). A good cosmetic outcome and high patient satisfaction was achieved at 3 months (Figure 1G & H).
Diagnosis
Fibroma is a common non-neoplastic reactive lesion of oral cavity but rare on lips. It can be congenital, infectious, inflammatory, and traumatic in origin. The lesion in the present case report was suspected to be traumatic in origin due to lip biting.

Figure 1: (A, B) Preoperative view of lesion. (C) Excisional biopsy of 4*4 mm growth using elliptical incision with 1 mm healthy margin. (D) Suturing of deeper layer using 7-0 vicryl suture. (E) Superficial sutures in place to achieve primary closure of wound edges. (F) 1 month follow up. (G, H) 3 months follow up.
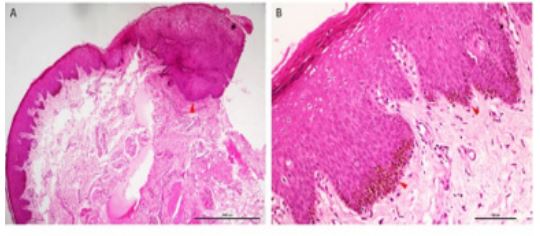
Figure 2: (A) Photomicrographs showing orthokeratotic stratified squamous epithelium continuing into hyperplastic parakeratotic stratified squamous epithelium with focal area displaying elongated and broad rete ridges (red arrowhead). Underlying collagenous stroma showed melanin incontinence in juxtaepithelial region, mild inflammation and AB-PAS negative eosinophilic exudate. (B) Basal third of epithelium showed basilar hyperplasia and melanin pigment (red arrowhead). S100 immunostaining showed no melanocytic hyperplasia.
Discussion
Fibroepithelialpolyp (FEP) or fibroma is a common non-neoplastic reactive lesion of theoral cavity. Although its aetiology is unknown, it can be congenital, infectious, inflammatory, or traumatic in origin. It clinically presents as a painless sessile or pedunculated growth. It can have firm and resilient, or soft and spongy consistency [1]. FEPs are non-malignant and have low recurrence rates. It is a commonly reported lesion on buccal mucosa and gingiva, but involvement of the lip is rare [2,3]. To the best of our knowledge this is a rare case reporting the occurrence of FEP on the lip.
Histologically, the present lesion showed ortho-keratinised stratified squamous epithelium continuing into hyperplastic para-keratinised stratified squamous epithelium with basilar hyperplasia and elongated rete ridges. Underlying connective tissue showed mild inflammation (Figure 2). Based on the histological picture, the case was diagnosed as FEP/ fibroma.
Lips are highly visible facial structureswhich are exposed to various internal and external stimuli, resulting in the development of diverse lesions. The diagnosis of these lesions can be difficult, often warranting the need for biopsy. Excisional biopsy of the suspected orofacial lesion can bemost challenging because it may result in deformity,especially those involving vermilion border of the lip.Patient satisfaction and self-reported aesthetics have become significant patient reported outcome measures.Utmost surgical precision is required for good cosmetic outcome. Early healing and good aesthetics with minimal scarring of the healed tissues can be better achieved by primary closure of the wound using microsurgical technique as compared to conventional suturing [4].
In the present case report double-layered microsurgical suturing was performed. The deeper layer was first sutured to minimize tension at the wound edge and reduce the dead space followed by superficial suturing of the wound margins to achieve primary closure [5]. The healing was uneventful with highly aesthetic outcome at 3 months follow up.
Outcome
A good cosmetic outcome and high patient satisfaction can be better achieved using microsurgical technique especially in highly cosmetic areas.
Conflict of interest statements: The authors declare no conflict of interest.
References
- Yeatts D & Burns JC. Common oral mucosal lesions in adults. American Family Physician. 1991; 44(6): 2043-2050.
- Monteiro LS, Albuquerque R, Paiva A, de la Peña-Moral J, Amaral JB & Lopes CA. A comparative analysis of oral and maxillofacial pathology over a 16-year period, in the north of Portugal. International Dental Journal. 2017; 67(1): 38-45.
- Sengüven B, Bariş E, Yildirim B, Shuibat A, Özer Yücel Ö, Museyibov F, et al. Oral mucosal lesions: A retrospective review of one institution’s 13-year experience. Turkish Journal of Medical Sciences. 2015; 45(1): 241-245.
- Yadav VS, Salaria SK, Bhatia A & Yadav R. Periodontal microsurgery: Reaching new heights of precision. Journal of Indian Society of Periodontology. 2018; 22(1): 5-11.
- Lloyd JD, Marque MJ & Kacprowicz RF. Closure techniques. Emergency Medicine Clinics of North America. 2007; 25(1): 73-81.

