Case Report - Volume 2 - Issue 6
Severe renal trauma after twice Extracorporeal Shockwave Lithotripsy (ESWL)
Zhengxi Zhou; Yanping Huang; Xiaoxiang Wang*
Department of Urology, The Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou 225000, Jiangsu Province,China.
Received Date : Oct 08, 2022
Accepted Date : Nov 18, 2022
Published Date: Dec 12, 2022
Copyright:© Xiaoxiang Wang 2022
*Corresponding Author : Xiaoxiang Wang, Department of Urology, The Affiliated Hospital of Yangzhou University, Yangzhou University, No. 368 Hanjiang Middle Road, Yangzhou 225000, Jiangsu Province, China.
Email: 18936489811@163.com
DOI: Doi.org/10.55920/2771-019X/1319
Abstract
Background: The complications of extracorporeal shockwave lithotripsy (ESWL) occur in a few patients. In addition, serious renal trauma is extremely rare. we report a severe complication of kidney trauma after receiving twice ESWL.
Case Presentation: A 56-year-old Man was transferred to our Emergency Department (ED) with severe left flank pain. He had undergone ESWL twice for the left renal stone at intervals of less than four days. Left flank pain developed immediately after second ESWL and was not spontaneously relieved. Computed tomography (CT) performed in our hospital showed an extensive left perinephric hematoma. His vital signs were unstable and were not stabilized even with fluid resuscitation and transfusion. Left nephrectomy was selected for the progressive decline of hemoglobin Hb levels. He was discharged on the 11th hospital day safely.
Conclusion: Although it is rare, patients may present with kidney trauma especially when receiving twice ESWL in a short time.
Key words: ESWL; hematoma; urolithiasis; renal trauma; nephrectomy; case report.
Abbreviations
ESWL: Extracorporeal shockwave lithotripsy; CT: Computerized tomography; ED: Emergency Department; NOM: non-operative management; RFs: Residual fragments; Hb: Hemoglobin; Hct: Hematocrit.
Introduction
It is well generally accepted that extracorporeal shockwave lithotripsy (ESWL) has becoming a safe and useful treatment modality for urolithiasis, since it was first applied in the early1980s [1,2]. Researchers have always believed that the destructive forces, created via the extracorporeal shockwave, would cause damages to adjacent tissues and vessels in the kidney [3]. Only less than 7% patients who receiving ESWL would generate mild Complications, and severe kidney trauma is extremely rare [4]. In this report, we describe the case of a grade Ⅳ renal trauma patient after ESWL treatment. The relevant literature was also reviewed in order to help improve the treatment of urolithiasis.
Case presentation
A 56-year-old man was transferred to our Emergency Department (ED) with severe left flank pain in Immediately after he had undergone ESWL twice at less than four days. He has no known significant past medical history and special family history. Initial vital signs at the emergency
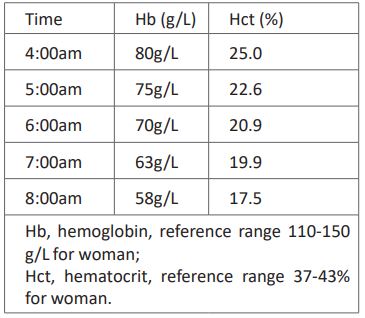
department was follows: blood pressure, 145/65 mmHg, heart rate,70 beats/min; respiratory rate,20/min; body temperature,36.4℃; and blood oxygen saturation, 99%. Routine blood test revealed an initial hemoglobin (Hb) level of 80g/L, a hematocrit (Hct) of 25.0%. In the following time these two indicators still showed a progressive decline, although physicians had tried a conservative therapy with many transfusions. These results are shown in (Table 1).
Table 1: The decline of the Hb and Hct.
Computed tomography (CT) demonstrated a huge left perirenal haematoma (Figure. 1A and B). the patient was diagnosed with grade Ⅳ renal trauma at least. Thus, it was finally decided to treat the patient with left nephrectomy. In the surgical report it is documented that the left kidney showed a rupture of the capsule, renal laceration >1.5 cm depth, subcapsular haemorrhage and massive haemorrhage around the left kidney. On the 5th hospital day, CT images showed that there was no additional hematoma (Figure. 2.). He was discharged from the hospital on the 11th hospital day without extra complications.
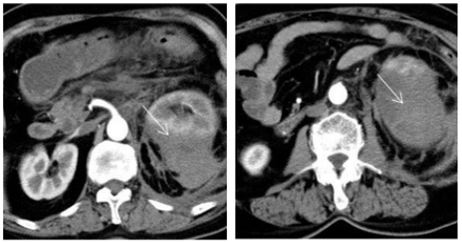
Figure 1: CT scans show an extensive left perinephric hematoma (white arrow, size: 8.6*7.3*15 cm).
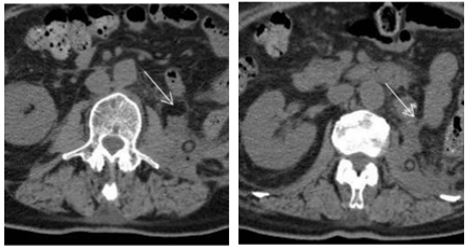
Figure 2: CT scans show there are no external hematoma after nephrectomy.
Discussion
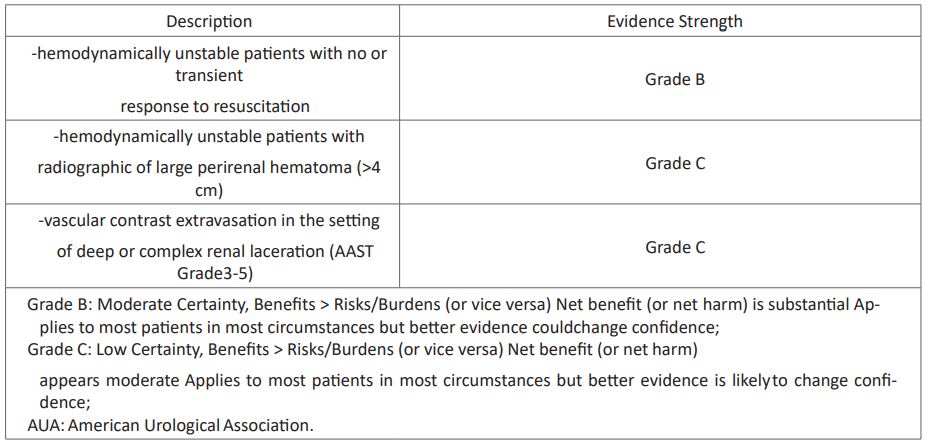
Renal Injury
The kidneys are paired retroperitoneal structures lying against the psoas muscles, cushioned by perinephric fat, and surrounded by Gerota’s fascia. Renal trauma accounts for approximately 3% of all trauma admissions and as many as 10% of patients who sustain significant abdominal trauma [5]. CT imaging has become the essential inspection for the diagnosis of organ injury after trauma [6]. Please refer to (Table 2) for the grading of kidney injury severity. Several studies have confirmed the safety of non-operative management (NOM) in renal injury [8], and NOM has become the standard in most patients with renal trauma, even in high grade patients, the NOM success rate can reach to 80% when haemodynamics is stable [9]. Although the angioembolization for the treatment of active bleeding complications may have established an intermediate step between NOM and traditional surgery [10]. Immediate surgical management is widely accepted in some special circumstances [11]. (Table 3) outlines the indications of operative intervention in blunt renal injury. Finally, we choose the left nephrectomy to save the life of patient.
Table 2: Kidney Injury Scale of 2018 AAST [7].
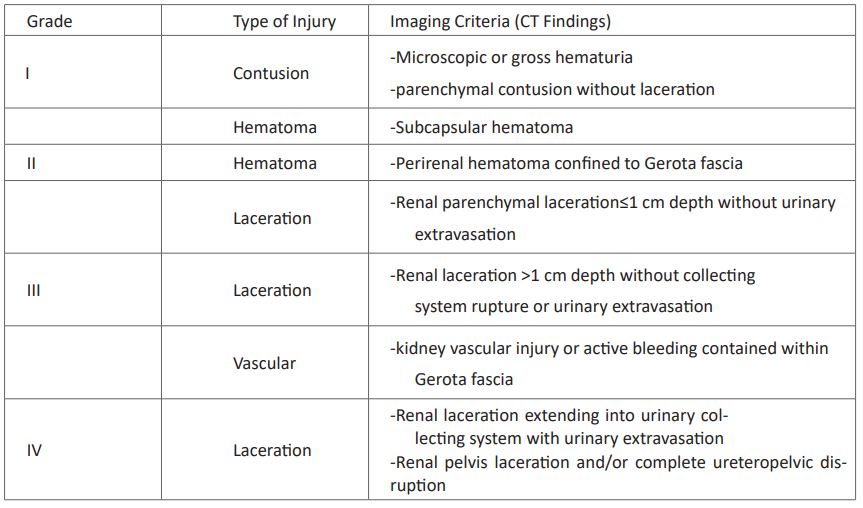
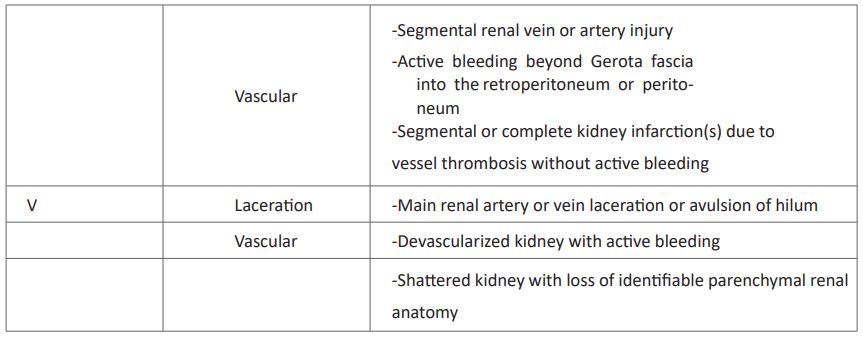
More than one grade of kidney injury may be present and should be classified by the higher grade of injury;
Advance one grade for bilateral injuries up to Grade III; ASST: the American Association for the Surgery of Trauma.
Table 3: Indications for Operative Intervention of 2020 AUA Guideline [12].
Our Experience of ESWL
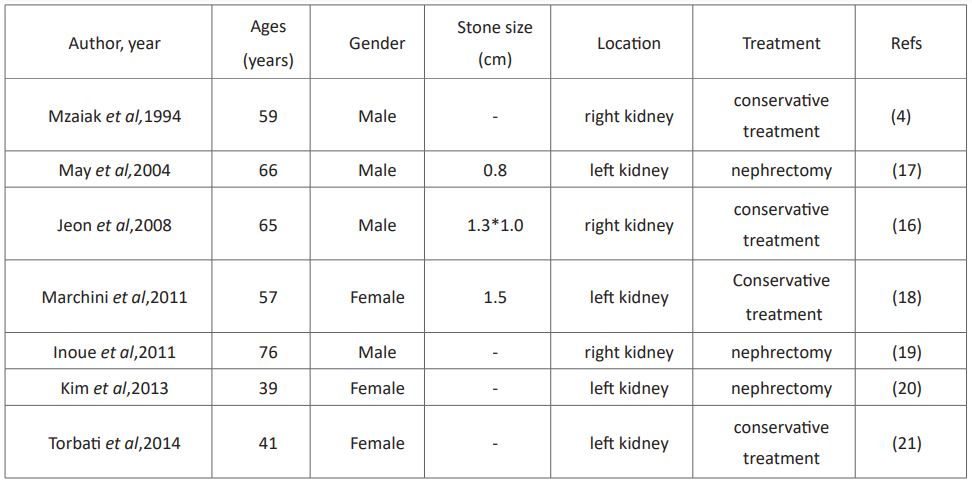
Extracorporeal shockwave lithotripsy (ESWL) has been widely used for treatment of ureteral and symptomatic renal stones, which is showed in (Table 4). While increasing evidence suggested that ESWL could lead to various complications (Table 5). Previous studies have proved that we could lower the pulse rate to 60-80 shock waves/min and ramp up the energy voltage gradually (rather than beginning at maximum energy) to improve the safety and efficacy of ESWL [15]. However, there is a report that the incidence of renal hematoma after ESWL to occur in 0.2– 0.7% of cases when examined by ultrasonography, but when examined by CT or magnetic resonance imaging, the figures would fly to 23–26% [16]. The results indicated that the ESWL may cause potential damages to kidney more than we expected. Reviewing the previous literature, only seven cases we found were reported for severe kidney trauma in adults after ESEL. The characters of each case are shown in (Table 6).
Residual fragments (RFs) following ESWL method seems inevitable [22]. At present, no acknowledged or standardized protocol exists regarding their definition, diagnosis, and treatment with the different procedures available [23]. In our patient, when He first received the ESWL for curing the ureteral calculus, the left kidney may have small renal hematoma. Unfortunately, the following ultrasonography only showed the left kidney stones, so our patient received a second ESWL treatment at intervals of less than four days. That may be the main reasons for the severe renal trauma.
Table 4: The relative indication of ESWL.
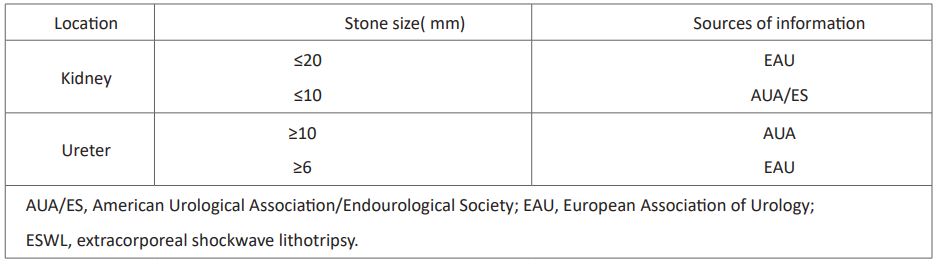
Table 5: Common complications after ESWL.
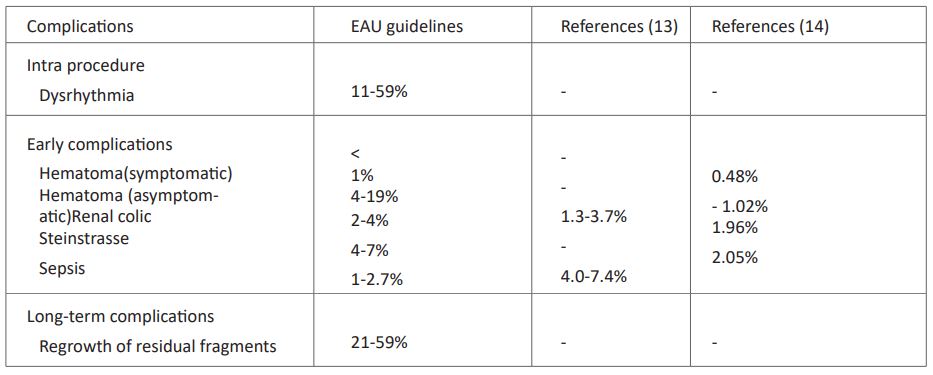
Table 6: Reported cases of severe renal trauma.
Conclusion
When patients would receive second ESWL treatment for RFs, there is a need for longer intervals. Physicians should bear in mind the possibility of potential kidney injury after ESWL method and should also closely observe there is a better way dealing with RFs.
Consent
Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Competing interests: The authors declare that they have no competing interests.
Author’s contributions
ZxZ and YpH drafted the report. XxW cared for patient and approved the final version of the manuscript. All authors read and approved the final manuscript.
Acknowledgements: No sources of funding need to be declared.
References
- Chaussy C, Schuller J, Schmiedt E, Brandl H, Jocham D, Liedl B. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology. 1984; 23: 59-66.
- Sundaram CP, Saltzman B. Extracorporeal shock wave lithotripsy: a comprehensive review. Compr Ther. 1998; 24(6-7): 332-335.
- McAteer JA, Evan AP. The acute and long-term effects of shock wave lithotripsy. Semin Nephrol. 2008; 28: 200-213.
- Maziak DE, Ralph-Edwards A, Deitel M, Wait J, Watt HJ, Marcuzzi A. Massive perirenal and intra-abdominal bleeding after shockwave lithotripsy: case report. Can J Surg. 1994; 37: 329-32.
- 5 Brandes SB, McAninch JW. Renal trauma: a practical guide to evaluation and management. Scientific World Journal. 2004; 4(1): 31-40.
- Stuhlfaut JW, Anderson SW, Soto JA. Blunt abdominal trauma: current imaging techniques and CT findings in patients with solid organ, bowel, and mesenteric injury. Semin Ultrasound CT MR. 2007; 28(2): 115-129.
- Kozar et al. Organ injury scaling 2018 update: Spleen, liver, and kidney. J Trauma Acute Care Surg. 2018; 85(6): 1119-1122
- MA Bjurlin, RJ Fantus, RJ Fantus, D Villines. Comparison of nonoperative and surgical management of renal trauma: can we predict when nonoperative management fails? J. Trauma Acute Care Surg. 2017; 82: 356-361.
- S Cimbanassi, O Chiara, A Leppaniemi, S Henry, TM Scalea, K Shanmuganathan, et al. Nonoperative management of abdominal solid organ injuries following blunt trauma in adults: results from an international consensus conference, J. Trauma Acute Care Surg. 2018; 84(3): 517-53.
- DJ Bryk, LC Zhao. Guidelines of guidelines: a review of urological trauma guidelines, BJU Int. 2016; 117: 226-234.1
- JJ Shoobridge, MF Bultitude, J Koukounaras, PL Royce, NM Corcoran. Predicting surgical exploration in renal trauma: assessment and modification of an established nomogram, J. Trauma Acute Care Surg. 2013; 75: 819-823.
- Morey AF, Broghammer JA, Hollowell CMP, McKibben MJ, Souter L. Urotrauma Guideline 2020: AUA Guideline. J Urol. 2021; 205(1): 30-35.
- Sun XZ, Zhang ZW. Shockwave lithotripsy: instrumentation and status in China. J. Endourol. 2005; 19: 774-9.
- Jagtap J, Mishra S, Bhattu A, Ganpule A, Sabnis R, Desai M. Evolution of shockwave lithotripsy (SWL) technique: a 25-year single centre experience of > 5000 patients. BJU Int. 2014; 114: 748-53.
- Elmansy HE, Lingeman JE. Recent advances in lithotripsy technology and treatment strategies: A systematic review update. Int J Surg. 2016; 36: 676-680.
- Jeon BH, Jang JH, Oh JH, et al. Kidney rupture after extracorporeal shockwave lithotripsy: report of a case. J Emerg Med. 2009; 37(1): 13-14.
- May M, Gunia S, Helke C, Seehafer M, Hoschke B. Eine seltene Komplikation der Extrakorporalen Stosswellenlithotripsie: Nierenruptur mit nachfolgender Nephrektomie [An unusual complication of extracorporeal shock wave lithotripsy: rupture of the kidney with consecutive nephrectomy]. Aktuelle Urol. 2004; 35(4) :316-319.
- Marchini GS, Lopes RI, Bruschini H, Torricelli F, Lopes RN. Tratamento conservador detrauma renal grave após litotripsia extracorpórea por ondas de choque [Conservative treatment of severe renal trauma after extracorporeal shockwave lithotripsy]. Rev Col Bras Cir. 2011; 38(6): 447-449.
- Inoue H, Kamphausen T, Bajanowski T, Trübner K. Massive retroperitoneal haemorrhage after extracorporeal shock wave lithotripsy (ESWL). Int J Legal Med. 2011; 125(1): 75-79.
- Kim HG, Bae SR, Lho YS, Park HK, Paick SH. Acute cyst rupture, hemorrhage and septic shock after a shockwave lithotripsy in a patient with autosomal dominant polycystic kidney disease. Urolithiasis. 2013; 41(3): 267-269.
- Torbati SS, Niku M, Vos E, Hogan S. Renal rupture following extracorporeal shockwave lithotripsy. West J Emerg Med. 2014; 15(6): 706-707.
- Tiselius HG and Chaussy CG. Arguments for choosing extracorporeal shockwave lithotripsy for removal of urinary tract stones. Urolithiasis. 2015; 43(5): 387-396.
- Prezioso D, Barone B, Di Domenico D, Vitale R. Stone residual fragments: A thorny problem. Urologia. 2019; 86(4): 169-176.

