Case Report - Volume 2 - Issue 6
The Salford technique of correction of rotational malalignment in lower limbs
Rajkumar Sundarapandian1*; Paul Nesbitt2; Aiman Khunda3
1Senior clinical fellow in Orthopaedics Department of Orthopaedics, Salford Royal Hospital, Stott lane, Salford M6 8HD, United Kingdom.
2Orthopaedic Registrar, Department of Orthopaedics, Salford Royal Hospital, Stott lane, Salford M6 8HD, United Kingdom.
3Consultant Orthopaedic and Limb Recon Surgeon, Department of Orthopaedics, Salford Royal Hospital, Stott lane, Salford M6 8HD, United Kingdom.
Received Date : Oct 12, 2022
Accepted Date : Nov 21, 2022
Published Date: Dec 14, 2022
Copyright:©Rajkumar Sundarapandian 2022
*Corresponding Author : Rajkumar Sundarapandian, Senior clinical fellow in Orthopaedics Department of Orthopaedics, Salford Royal Hospital, Stott lane, Salford M6 8HD, United Kingdom. Tel: 07402 423902.
Email: rkzzwig@gmail.com
DOI: Doi.org/10.55920/2771-019X/1321
Abstract
Derotational osteotomies of lower limb are widely used to correct rotational deformity and the ability to translate pre-operative plan to accurate intra-operative correction remains challenging in these situations. Salford technique uses pre-operative CT scan, limb length radiographs and PACS tools to calculate a correction distance that can be marked on the surface of bone at the osteotomy site intra-operatively to obtain accurate correction. The calculation is based on the two dimensional geometrical formulae of a circle. We present this case report of a patient who underwent derotational osteotomies of femur and ipsilateral tibia along with Medial patellofemoral ligament reconstruction using this technique. Salford technique is simple, reproducible and cost effective in allowing surgeons to accurately correct rotational deformity of lower limbs without the need for specialist equipment.
Keywords: Rotational deformity; derotational osteotomy; Salford technique.
Introduction
Rotational deformities of lower limb such as excessive anteversion and tibial torsion are often idiopathic [1]. These deformities resolve spontaneously in 90% with physiological growth [2]. Deformities which persist beyond the age of resolution can cause femoro-acetabular impingement and patellar instability [3]. De-rotational osteotomyiswidely used to correct symptomatic deformities. The ability to translate pre-operative plan to accurate intra-operative correction remains challenging in these situations, aslandmarks in long bones away from osteotomy site are often used in pre-operative planning. We propose a new technique using pre-operative CT scan, limb alignment radiographs and PACS tools to calculate correction distance that can be marked on the surface of bone at the osteotomy site intra-operatively to obtain accurate correction.
Case report
A 23-year-old female presented with in-toeing gait and patellar instability in both knees. She was more symptomatic on the left side which was planned for a single stage left femoral and tibial derotation osteotomy. Femoral ante-version of 46 degrees was measured with the angle subtended by axis of the femoral neck and posterior femoral bi-condylar axis using axial CT scan images (Figure 1a and 1b).The desired ante-version was set at 16 degrees (opposite side was not used as reference) and a correction value of 30 degrees was needed to achieve it.
The site of osteotomy in femur was determined by the presence or absence of patellofemoral instability. Where the osteotomy is intended to improve stability of patellofemoral joint, a distal femoral osteotomy is employed. If the purpose is purely to correct foot progression angle, then an osteotomy just proximal to the femoral isthmus is carried out. A distal osteotomy will rotate the distal femur and bring it under the patella/extensor mechanism, improving stability of patello-femoral joint. A proximal osteotomy will not only rotate the femur but also the extensor mechanism including the patella, resulting in little or no effect on patello-femoral joint stability.
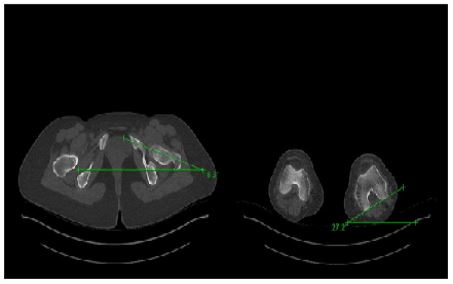
Figure 1: Measurement of ante-version on axial CT images.
De-rotation distance is then calculated after the site of osteotomy is chosen. The calculation method is based on two dimensional geometrical formulae of a circle. The circumference of a circle can be worked out by measuring its diameter (Circumference = P x diameter). The diameter of the circle in this instance being medio-lateral distance of femur at the site of osteotomy on axial CT image (Figure 2a and 2b). Distal femoral osteotomy site above the trochlea was chosen and measured 60mm proximal to knee joint. The medio-lateral distance/diameter of circle at the osteotomy site measured 45mm on axial CT and this was used to calculate circumference of circle (Figure 2a and 2b).
Circumference =3.14 x 45 = 141.3mm.
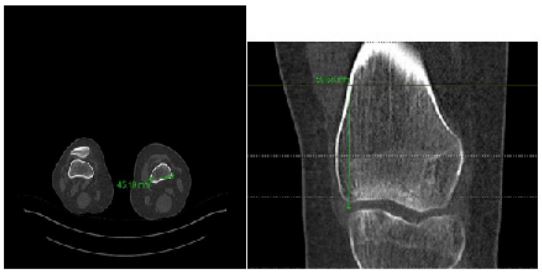
Figure 2: Measurement of medio-lateral distance of bone at the planned osteotomy site.
A circle is then superimposed at the site of osteotomy with its centre at the centre of de-rotation. Circumference is then divided by 360 to determine the degrees of rotation per millimetre of circumference. Multiplying this by the correction value for desired ante-versionwill give us the correction distance along the circumferenceto achieve the desired rotational correction.
De-rotation distance(mm) = (circumference/360) x correction value for desired ante-version
De-rotation distance = (141.3/360) x 30 = 11.775mm
A medial sub-vastus approach was used to expose the distal femoral osteotomy site. Bone was marked in coronal plane with a 20mm osteotome representing the starting point for the osteotomy.The plane of osteotomy was perpendicular to the mechanical axis. Using image intensifier a 2mm wire was passed though the distal femur at the osteotomy site. Osteotomy was then carried out using a saline cooled oscillating saw. The distal fragment was externally rotated by 11.7mm till point A and point B were colinear (Figure 3a and 3b). A flexible ruler was used to ensure de-rotation distance (mm) was accurate. Osteotomy was stabilised using medial distal femoral plate ensuring maintenance of rotational correction obtained (Figure 4). This de-rotation distance of 11.7mm indicated that every millimeter of de-rotation reduced ante-version by 2.5 degrees. The technique of correction of excessive tibial torsion is similar to the one described above (Figure 5).
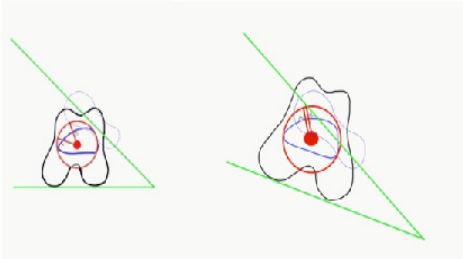
Figure 3: Derotation osteotomy demonstrating reduction of ante-version.

Figure 4: Fixation of distal femur with plate and screws after derotation osteotomy.

Figure 5: Fixation of tibia with intramedullary nail after derotation osteotomy.
Persistent patellar instability noted after derotation of femur and tibia was completed in this patient. Medial patellofemoral ligament reconstruction was done at the end of the procedure. Post-operative followup at 2 years revealed good functional outcome with no evidence of patellar instability.
Discussion
CT scan can help measure planned correction to 0.1 of a millimetre [4,5], assisted by PACS tools. Our method of superimposing a circle with centre of rotation at the anatomical axis of diaphysis and using a simple mathematical formula to calculate measurable rotation distance is easy to understand, employ and reproduce without the need for specialist equipment. It can be used on any location of femur or tibiaonce the centre of rotation is on the osteotomy site. We have used the above described technique to correct rotational abnormality in 5 patients.
Kamath et al [6] describe a sub-trochanteric technique for correcting femoral rotation with surgical hip dislocation, trochanteric osteotomy and a period of non-weight bearing post-operatively. None of our patients required hip dislocation or non-weight bearing post-operatively. Naqvi et al [7] in their series used a blade plate or proximal femoral plate and reported complications including non-union, knee pain and metal failure. Results were good with satisfactory patient reported outcome in all but 3 cases.
Nelitz et al [8] and Dickshas et al [9] have shown patello-femoral instability can be resolved by de-rotational osteotomy. Two patients in our studypresented with patellar instability with persistent laxity when tested after de-rotation of femur and tibia were complete. MPFL is often found to be weak and insufficient in patients with chronic rotational malalignment. Our observations indicate that despite improvement of TT-TG distance, it fails to provide a checkreinto patella. We suggest MPFL reconstruction if pre-operative MR scan showed incompetence of ligament.
Limitations of our study include small number of patients, lack of a long term followup and inability to quantify achieved correction with CT scan in all patients. Assessment of surgical outcome depend on restoration of normal foot progression angle and patient reported functional improvement. We are in the process of prospectively establishing longer term follow-up and increasing the number of patients in our study to further validate our findings.
Conclusion
Salford technique of osteotomy will allow the surgeon to correct rotational deformity in lower limbs accurately by removing the need to use distant landmarksaway from the centre of rotation. Our technique is simple, reproducible, cost effective and requires no specialist equipment.
Conflict of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- Gelberman RH, Cohen MS, Desai SS, Griffin PP, Salamon PB, O'Brien TM. Femoral anteversion. A clinical assessment of idiopathic intoeing gait in children. The Journal of bone and joint surgery. British volume. 1987; 69(1): 75-9.
- Dunn PM. Congenital postural deformities. British Medical Bulletin. 1976; 32(1): 71-6.
- Cameron JC, Saha S. External tibial torsion: an under recognized cause of recurrent patellar dislocation. Clinical Orthopaedics and Related Research®. 1996; 328: 177-84.
- Weiner DS, Cook AJ, Hoyt WA, Oravec CE. Computed tomography in the measurement of femoral anteversion. Orthopedics. 1978; 1(4): 299-306.
- Jakob RP, Haertel M, Stussi E. Tibial torsion calculated by computerised tomography and compared to other methods of measurement. The Journal of bone and joint surgery. British volume. 1980; 62(2): 238-42.
- Kamath AF, Ganz R, Zhang H, Grappiolo G, Leunig M. Subtrochanteric osteotomy for femoral mal-torsion through a surgical dislocation approach. Journal of hip preservation surgery. 2015; 2(1): 65-79.
- Naqvi G, Stohr K, Rehm A. Proximal femoral derotation osteotomy for idiopathic excessive femoral anteversion and intoeing gait. SICOT-J. 2017; 3.
- Nelitz M, Dreyhaupt J, Williams SR, Dornacher D. Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. International orthopaedics. 2015; 39(12): 2355-62.
- Dickschas J, Harrer J, Pfefferkorn R, Strecker W. Operative treatment of patellofemoral maltracking with torsional osteotomy. Archives of orthopaedic and trauma surgery. 2012; 132(3): 289-98.

