Original Article - Volume 2 - Issue 6
Perineural spread of rhino-orbito-cerebral mucormycosis in post-Covid-19 patients-Description of this rare pathwayin the rural population of southern Rajasthan
Dr Kritika1 ; Dr Sunil Kast2; Dr Rajaram Sharma3*; Dr Saurabh Goyal3; Dr Tapendra Tiwari2
1PG Resident, Radio diagnosis, Pacific institute of medical sciences,Umarda,Udaipur.
2Assistant Professor, Radio diagnosis, Pacific institute of medical sciences,Umarda,Udaipur.
3Associate Professor, Radio diagnosis, Pacific institute of medical sciences,Umarda,Udaipur.
Received Date : Nov 07, 2022
Accepted Date : Dec 02, 2022
Published Date: Dec 24, 2022
Copyright:© Rajaram Sharma 2022
*Corresponding Author : Rajaram Sharma, PG Resident, Radio diagnosis, Pacific institute of medical sciences, Umarda, Udaipur. Tel: +91-7755923389
Email: hemantgalaria13@gmail.com
DOI: Doi.org/10.55920/2771-019X/1330
Abstract
Background: Various opportunistic infections were found to be more common in patients with a history of Covid-19 infection after the second wave of pandemic. The rural and tribal population was severly hit due to quack practices, lack of health care, and knowledge. Clinical features range from non-invasive sinusitis to aggressive invasive form in immunocompetent hosts. Rhino-orbito-cerebral mucormycosis (RCOM) is a very infrequent but lethal fungal infection, usually affecting diabetic patients (Ketoacidosis state). It has characteristic patterns of spread, i.e., continuous, direct spread or via vascular invasion, while perineural spread being the least common pathway of invasion. We report nine cases of invasive fungal infection with an symptomatic perineural spread in this study.
Objectives: This article discusses Rhino-orbito-cerebral mucormycosis (ROCM) and highlights the benefits of contrast-enhanced magnetic resonance imaging (MRI) in diagnosing this potentially deadly form of perineural invasive mucormycosis.
Methods: In this retrospective observational study conducted in rural and tribal belt of southern Rajasthan, we assessed the imaging and clinical data of five men and four women (age 45±15) yearswho had a history of Covid-19 pneumonitis, and secondarily became infected with invasive mucormycosis and also had perineural spread, which was proven by using KOH positive staining (within two months of duration).The total sample size was 108 patients.
Conclusion: Multimodality imaging is found to be very helpful in making early diagnoses and timely intervention in RCOM. Multiplanar MRI shows anatomical involvement in RCOM and helps in planning the surgery.
Introduction
Health is the major priority in every individual’s life; hence it is a matter of common concern. In fact, all community groups have their own concept of health as part of their culture. The major challenges regarding maintaining a healthy culture are faced by the rural and tribal population due to many factors like the lack of primary health services in these areas and a rise in quack practices. Considering all these factors, the Indian government is promoting many projects for health improvement. As our institute is located along with one of the tribal belt of southern Rajasthan, patients who came to our hospital are usually malnourished and immune-compromised, or have advanced medical illness due to treatment from the untrained medical quacks in their respective villages. Quacks are the people either from the same village or nearby area who don’t have any professional qualification or practice experience but merely know some of the fast relief medicines, i.e., steroids, most of the time.
Rhino-orbito-cerebral mucormycosis is an infrequent but lethal fungal infection, usually affecting the immune-compromised patients like diabetics (Ketoacidosis in diabetes enhances susceptibility to rhino-orbito-cerebral mucormycosis) or other immune-compromised patients. In our patients, the cause might be a prolonged and high dose of steroid administration during the treatment of Covid-19 pneumonia leading to increase blood sugar levels [1,2]. It progresses rapidly with a pronounced increase in the mortality when the fungus invades the cranium and involves the intracranial vasculature and nerves. It has a characteristic spread pattern, i.e., continuous, direct spread orvia vascular invasion, while the perineural spread is the least common pathway of invasive mucormycosis. We saw nine cases of at ypical patterns of disease extension via the perineural spread.
This infection arises in the sinus mucosa and detonates to surrounding structures. In our patients, infection begin within the nasal cavity or paranasal sinuses primarily and then extended along the cranial nerves into the cranium and sometimes to the nucleus of the nerve.
Rhino-orbito-cerebral mucormycosis has a very high impermanency rate due to the invasive nature of the fungus, which leads to vascular occlusion or neural involvement resulting in substantial tissue necrosis and nerve damage. Prompt diagnosis and timely intervention is the key to a favourable outcome. We have aimed to study these features with more emphasis on perineural invasion in cases of invasive Rhino-orbito-cerebral mucormycosis. We portray a few cases of Rhino-orbito-cerebral mucormycosis in this article, emphasizing the utility of M.R.I., especially contrast-enhanced images, in the diagnosis of this assuredly lethal form of mucormycosis.
Material/Methods
Our study was a retrospective observational study that included 108 patients diagnosed with Mucormycosis over a period of six months from May 2021 to October 2021. Nine patients were selected (five men and four women, with age 45±15 yrs) for this study who were diagnosed with invasive rhino-orbito-cerebral mucormycosis by clinical features and K.O.H. positive staining. All patients had a history of Covid-19 pneumonitis and had deranged blood sugar levels during ward stay for the present illness. The cases were clinically classified as rhino-orbital, rhinocerebral, or rhino-orbito-cerebral based on the presenting features of unilateral or bilateral periorbital facial tenderness, numbness, visual impairment/loss, chemosis, proptosis, ophthalmoplegia, eyelid oedema, multiple cranial nerve palsies, neurological deficits, surrounding bone involvement.
Patients under went multiparametric and multiplanar magnetic resonance imaging of the orbits, paranasal sinuses and brain on a 1.5 Tesla machine (G.E. healthcare 2014 model). The imaging entente comprises T1 weighted(W), T2W, susceptibility-weighted, diffusion-weighted, T2 fat-suppressed, pre and post-contrast T1W fat-suppressed images in multiple planes.10 ml of contrast Omniscan (0.5mmol/ml contains gadodiamide, caldiamide sodium hydroxide or hydrochloride acid) was injected intravenously before obtaining post-contrast images.
M.R.I. revealed polypoidal mucosal thickening involving unilateral or bilateral maxillary /ethmoid and frontal sinuses, causing opacification of the sinus cavity, which shows a hyperintense signal on the T2W images. In the post-contrast study, there were three patterns of mucosal enhancement observed in the mucosa and nasal cavity, intense homogenous enhancement, heterogeneous enhancement, and central non-enhancement with rim enhancement.
Feature indicating invasive Rhino-orbito-cerebral mucormycosis included abnormal signal intensities and enhancing thickening of either side of periorbital soft tissues, retro-antral fat, and facial skin. Extension into the orbit was characterized by fat stranding in extra or intra-conal fat and thickening of extraocular muscles resulting in anterior bulging of either of the eye (proptosis). Abscess formation and globe deformation were also observed in four cases. On contrast-enhanced T1W images, heterogeneous enhancement was noted in either side of cavernous sinus compatible with cavernous sinus thrombosis. Internal carotid involvement is diagnosed when there was a changecalibre of the vessel, thrombosis and abnormal arterial wall enhancement. Meningitis, encephalitis and abscess formation were intracranial manifestations of the disease.
The Rhino-orbito-cerebral mucormycosis lesions show hypointense signal on T1W images, the hyperintense signal on T2W images, which demonstrated evident restricted diffusion with corresponding low A.D.C. signals. Post-contrast images revealed abnormal meningeal enhancement and peripherally enhancing abscesses. Two of our patients showed enhancing lesions in the nasal cavity that spreaded through the cribriform plate into the brain parenchyma along the 1stcranial nerve (olfactory nerve) (Figure 1). The other four patients had involvement of periorbital soft tissue, with involvement of the 2nd cranial nerve (optic nerve) and that reached till the optic chiasma (Figure 2 & 3). The next category is three patients with primary involvement of pterygopalatine fossa, extended into the middle cranial fossa from the foramen ovale via mandibular nerve (Figure 4). Further more, the lesion spreaded to Meckel's cave and extended into the prepontine segment of the trigeminal nerve (Figure 5 & 6).
Nasal cavity tissue or infected soft tissue biopsy specimen divulge aseptate hyphae with branching pattern on K.O.H. smear and culture, thus confirmed as mucormycosis. The patient was managed on intravenous Amphotericin-B and underwent surgical debridement along with blood sugar control by an Insulin therapy.
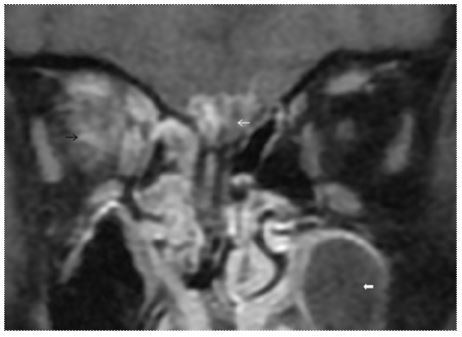
Figure 1: T1 weighted fat-saturated (T1W FS) post-contrast coronal image illustrates the intracranial extension of the disease through the cribri form plate and olfactory nerve (white arrow). The right orbital apex shows the involvement of the optic nerve and extraocular muscles (black arrow). Left maxillary sinus shows type 3 enhancement (thick arrow).
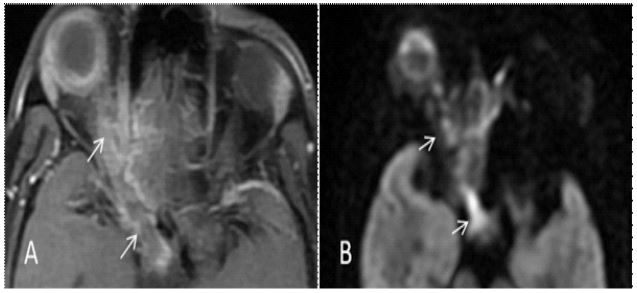
Figure 2: Images demonstrating an intracranial extension of disease along the optic nerve. (A) T1 weighted fat-saturated (T1 F.S.F.S.) post-contrast axial images shows diffuse orbital involvement and intracranial extension upto the chiasma along the right optic nerve (white arrow) (B) Diffusion-weighted image at corresponding level shows diffusion restriction along the path of extension of the disease (white arrow).
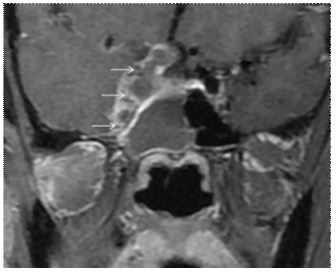
Figure 3: T1 fat-saturated (T1 F.S.F.S.) weighted post-contrast image shows: extension of the disease to left optic chiasma (white arrow).
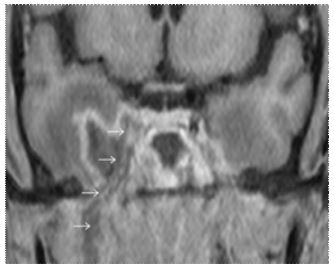
Figure 4: T1 weighted fat-saturated (T1 F.S.F.S.) post-contrast images demonstrates perineural spread along the right mandibular nerve extending intracranially via foramen ovale (white arrows).
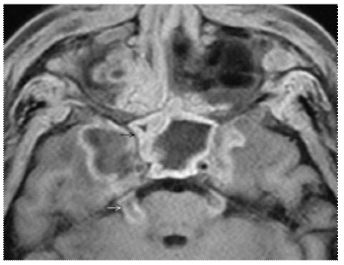
Figure 5: In a different patient, T1 weighted fat-saturated (T1W FS) post-contrast axial image shows bilateral cavernous sinus thrombosis and perineural spread along a right trigeminal nerve upto the nucleus the pons.
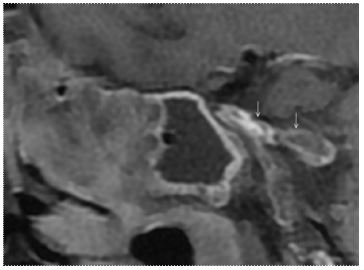
Figure 6: T1 weighted fat-saturated (T1W FS) post-contrast sagittal image showing heterogeneous enhancement in right sphenoid sinus extending to the trigeminal nerve.
Discussion
There were few specific features of Covid-19 seen in the second wave of the pandemic, firstly, a tendency to cause capacious pulmonary disease followed by analveolo-interstitial pathology that may aggravate the risk of invasive fungal infections. Secondly, the immune derangement linked with Covid-19, with reduced T lymphocytes, CD4+T, and CD8+T cells, may amend innate immunity making the patient more vulnerable to opportunistic fungal infections [3]. Mainly, neutrophils are responsible for protection against fungi, and any change in the number or function of these white cells leads to an escalate the risk of infection.
Letters or articles were searched on Pubmed with the search letter mucormycosis," "Mucor, " and "Covid-19" to spot any additional reported cases. Only a few case reports of secondary mucormycosis with perineural spread have been reported till now. Hanley et al. have reported a case of a young male with Covid-19 pneumonia and a middle cerebral artery (MCA) infarct in whom dispersed mucormycosis involving the lungs and brain was incidental during a postmortem study [4]. Mucormycosis is a potentially lethal opportunistic infection of immunocompromised patients. Rhino-orbito-cerebral mucormycosis is a rare assertive fungal infection. Around 80% of cases occurred in patients with diabetes and it had been declared endemic in India after the surge of the second wave. In diabetes, an elevated blood glucose levels augment fungal growth. The serum of a patient with ketoacidosis is not able to stop the growth of the fungus. Many probable explanations of this resurgence were given, like immunomodulation by Covid-19 itself, extensive steroid use, industrial oxygen usage and prolonged wearing and reuse of the same mask over a long period [1,2]. It is an acute, lethal infection caused by fungi of the order mucorales in the class zygomycetes [2]. Specifically, the hyphae infiltrate the vessel walls with ensuing local thrombotic infarction [4]. This action often headway from the sinus cavity to the orbit and then cavernous sinus. Central nervous system (CNS) connivance may occur from the hematogenous route or direct infiltration and have a bare prognosis with a five-year survival rate of 20% to 45% [3]. The extend of established rhino-orbito-cerebral mucormycosis is a bit expected. The spread is from the paranasal sinuses; mucor fungi invade the orbits and then into the cavernous sinus.
Nevertheless, straightway of infection through the cribriform plate into the anterior cranium may also occur, and it was suggested as a perineural spread [5]. Direct fungal invasion of the seventh and eighth cranial nerves from the internal auditory canal subarachnoid space has been documented in the former studies. However, it arises in the environs of fulminant meningitis from Cryptococcus or Aspergillus organisms [6]. There was no fungal involvement seen in the sensory ganglion [7]. The use of MRI to evaluate rhino-orbito-cerebral mucormycosis was first reported in 1988 by G.A. Press et al. in his study [4]. For evaluation of extracranial perineural spread, both CT and MRI imaging give sufficient information. However, MRI is proved to be superior for the cisternal segment, brain stem and skull base involvement and other potential routes of intracranial fungal invasion [8]. MRI has proved to be the most helpful technique for cavernous sinus involvement. Multiplanar ability and high tissue resolution make MRI the modality of choice for studying the entire intracranial pathway of the cranial nerve. MRI findings described in the R.O.C.M. include an abnormal hyperintense sinus mucosal wall, T2-W hyperintense lesion expanding from paranasal sinus across orbital apex then into intracranial structures encasing the vessel walls leading to slow flow in the ipsilateral vessel in the vicinity of mucor invasion. MRI well exhibited all these characteristic features in our cases. We further more noticed hyperintense signal intensity on D.W.I. and simultaneous hypointense signal on A.D.C. maps in the lesion lengthen from orbit to cavernous sinus, congenial with restricted diffusion [9]. D.W.I. of the brain also showed small infarcts in the watershed distribution in the high parietal region.
Our cases of perineural spread of rhino-orbito-cerebral mucormycosis are distinct in that fungal elements involved multiple cranial nerves, with no apparent leptomeningitis. Spread of infections to the hard and soft palate can easily ingress the greater and lesser palatine nerves, while these infections in the cheek and orbital soft tissues can encase the infraorbital nerve. Above mentioned nerves ascend to form the maxillary nerve, which through pterygopalatine fossa, enters into the cavernous sinus via the foramen rotundum. This fungal infection can also spread to Meckel's cave from the cavernous sinus and then by the sides of the cisternal portion of the trigeminal nerve to the lateral side of the pons or the trigeminal nucleus.
Hematogenous extend from the cavernous sinus or internal carotid may cause distant cerebral infarction and abscess, normally ipsilateral to the initial disease. Bone involvement is relatively rare in acute disease. However, the infection spreads from one bone or fascia into another via inherent dehiscences in the fascia or through fissures, canals and foramina within the bone [5]. The direct spread of the infection may invade the CNS through the cribriform plate, orbital fissure or basal foramina [2,6].
Radiological affirmation of the perineural spread of rhino-orbito-cerebral mucormycosis is very rare, and there were only two other cases (also involving the mandibular part of the trigeminal nerve) reported in the previous literature as per our knowledge. McLean et al. [6] described the radio-pathologic findings, while Press et al. told about the MRI findings of expansion of the disease from the cavernous sinus to the pons. With the presence of characeteristic MRI findings, it seems reasonable to assume the perineural spread for rhino-orbito-cerebral mucormycosis, especially when there is evidence of thickening and enhancement of the trigeminal nerve along its path and association of pons.
Aggressive surgical epithelialization, intravenous Amphotericin-B therapy, control of blood glucose, and correction of the weakened immune response are the treatment strategies for invasive mucormycosis. The prognosis of cerebral mucormycosis is indigent, with 5-year survival rates of just 20%–45%. Health is essential for an individual’s well-being; it is also necessary for all productive activities in a society (Goel, 2002). Therefore, the Rajasthan State has ensured strong delivery of health and family welfare services throughout the peripheral areas of Rajasthan via voluntary workers, community health workers, and ASHA (Accredited Social Health Activists) etc. Continuous attempts are being made to supply the primary health care to these areas, conceding some issues like gender imbalance, inequality, availability, accessibility, and delivery of quality health care services and major one i.e., affordability. In order to build up the potency and quality of this primary health care delivery systems, Rajasthan Health System Development Project is being executed in all the 32 districts with financial encouragement from the World Bank. The prime goal is to strengthen secondary-level medical institutions. One of the significant issues in providing good medical care in India is the untrained/unqualified quacks providing unlicensed medical services. Since our institute is also located in the tribal area of southern Rajasthan where these quack practices, lack of healthcare services and health hygiene are major issues, so, we get a maximum number of patients who came up in the end-stage of the disease or are in a worsened state due to lack of awareness and are treated wrongly by these quacks.
Conclusions
The incident and recognition of invasive fungal and fungal-like infections are pick up threads in the population of post-Covid-19 patients. These organisms can cause more severe infections in immunosuppressed individuals. Moreover, they have a propensity to spread quickly and can promptly become lethal in immunocompromised patients. Some fungal and fungal-like infections have particular imaging presentations, while others exhibit atypical findings. Therefore, the radiologist must be awareof the embodiment of these fungal infections in the central nervous system and comment on the extension of thedisease based on their unique disease patterns. Although rare, the perineural spread should be kept in mind while reporting such cases. The availability and affordability of advanced diagnostic and therapeutaic health care is still limited in the tribal and rural population of India. The government or non proft social organisations should help these communities, so they can get adequate treatment.
References
- Basan C III, Rinoldi MG, Rauch RR, Jinkins JR. Fungal infections ofthebrain.NeuroimagingClin N Am. 1991; 1: 57-582.
- Yousem DM, Galetta SL, Gusnard DA, Goldberg HI. M.R.M.R. findings inrhino-cerebralmucormycosis.JComput Assist Tomogr.1989; 13: 878-8824.
- Gangneux JP, Bougnoux ME, Dannaoui E, Cornet M, Zahar JR. Invasive fungal diseases during COVID-19: we should be prepared. J Mycol Med. 2020; 30: 100971.
- Hanley B, Naresh KN, Roufosse C, et al. Histopathological findings and viral tropism in U.K.U.K. patients with severe fatal COVID-19: a postmortem study. Lancet Microbe. 2020.
- Bowen BC, Post MJD. Intracranial infection. In: Atlas S.W.S.W., ed.Magnetic Resonance Imaging of the Brain and Spine.NewYork:Raven Press. 1991: 501-5386.
- McGill TJI. Mycotic infection of the temporal bone.ArchOtolaryn-gol Head Neck Surg. 1978; 104: 140-1448.
- Ellis CJK, Daniel SE, Kennedy PG, Oppenheimer SM, Scaravilli F. Rhino-orbital zygomycosis.JNeurolNeurosurg Psychiatry. 1985; 48: 455-458.
- Parker GD, Harnsberger HR. Clinical-radiologic tissues in perineuraltumour spread of malignant disease of the extracranial head andneck.Radiographics. 1991; 11: 383-3997.
- Press GA, Weindling SM, Hesselink JR, Ochi JW, Harris JP. Rhino-cerebral mucormycosis: M.R.M.R.manifestations.JComput Assist To-mog. 1988; 12: 744-7495.

