Case Report - Volume 2 - Issue 6
Spontaneous surgical emphysema: A case report of a unique post-sleeve gastrectomy presentation
Ahmad E Al-Mulla1*; Abdulla E Sultan2; Fatemah Buhamad3
1Senior Specialist General Surgery, Fellowship Minimal Invasive and Bariatric and Endoscopy, fellowship American college of surgeons. Department of Surgery Farwaniya Hospital, Ministry of Health, Kuwait
2Consultant general surgeon, Fellowship Minimal Invasive and Bariatric surgery. Department of Surgery, Farwaniya Hospital, Ministry of Health, Kuwait.
3General surgery resident, department of surgery Farwaniya hospital, Ministry of health Kuwait.
Received Date : Nov 08, 2022
Accepted Date : Dec 06, 2022
Published Date: Dec 28, 2022
Copyright:© Ahmad E Al-Mulla 2022
*Corresponding Author : J Ahmad E Al-Mulla, Senior Specialist General Surgery and Bariatric Surgery, Fellowship Minimal Invasive and Bariatric and Endoscopy, fellowship American college of surgeons. Department of Surgery Farwaniya Hospital, Ministry of Health, Sabah Al-Nasser, Block 6, P. O. Box 13373, Farwaniya 81004, Farwaniya, Kuwait. Tel: 0096524888000
Email: draalmulla2007@gmail.com
DOI: Doi.org/10.55920/2771-019X/1333
Abstract
Nausea and vomiting are common joint presentations in post-sleeve gastrectomy. Nevertheless, it is uncommon forpost-sleeve gastrectomyto manifest through subcutaneous emphysema. It is essential to distinguish spontaneous subcutaneous emphysema from other more severe presentations. However, this is sometimes challenging due to its resemblance to numerous ambiguous conditions. Acknowledging these conditions in the early phases is essential to prevent adverse complications. In this report, we discuss the approach to and management of a unique post-operative presentation.
Keywords: Subcutaneous emphysema; vomiting; oesophageal rupture; Boerhaave syndrome; sleeve gastrectomy.
Introduction
Obesity is considered a pandemic disease [1]. In 2016, over eighteen per cent of the world's population was obese, according to the World Health Organization [2]. Bariatric procedures are the best solution in the management of obesity [3]. In total, 59.4 % of bariatric procedures are sleeve gastrostomies, according to the American Society of Metabolic and Bariatric Surgery’s report in 2019 [4]. However, they are highly successful procedures with outstanding outcomes in obesity and its co-morbidities [5]. Many known complications are associated with sleeve gastrectomy, such as gastroesophageal reflux (GERD), pulmonary embolism, infections, haemorrhage, and leaks [6]. Others are infrequent. We present a case report of a 19-year-old female with a rare presentation of neck-and-chest subcutaneous emphysema (SE) due to excessive forceful vomiting after sleeve gastrectomy.
Case report
A 19-year-old female patient was admitted with a case of post-sleeve-gastrectomy nausea and vomiting. The patient underwent sleeve gastrectomy two weeks prior to admission and had uneventful post-operative recovery and follow-up. Upon admission, the patient complained of severe nausea with forceful vomiting. She was nauseated and retching and had mild epigastric pain. She was vitally stable, and her investigations were unremarkable. A computer tomography scan (CT scan) showed no leakage or abnormal findings on admission. She was kept for observation and supportive management. The patient was well after three days of admission and was discharged home. Nevertheless, she presented again atour casualty department with an identical complaint. However, on this occasion, she had apparent swelling in the neck, upper chest, and per-orbital region. Neck and chest X-rays were conducted (Figures 1-2). Theserevealed marked subcutaneous emphysema (SE) and pneumomediastinum. A CTscan of the abdomen and chest with oral and IV contrast were requested for the patient to rule out airway or oesophageal injury. The CT scan displayed marked and ample subcutaneous emphysema with pneumomediastinum (Figure 3). No contrast leak from the oesophagus or stomach was noted. The patient was maintained on nil per oral with intravenous antibiotics and total parenteral nutrition. Ultimately, the SE diminished, and the patient resumed oral feeding. The patient was discharged after drinking adequate fluids and being seen by a nutritionist. After fourteen days, the patient was followed up in the surgical outpatient department with no symptoms of SE.
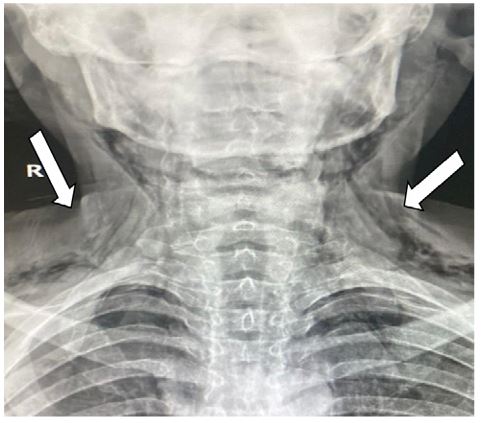
Figure1: Neck x-ray showing subcutaneous emphysema.
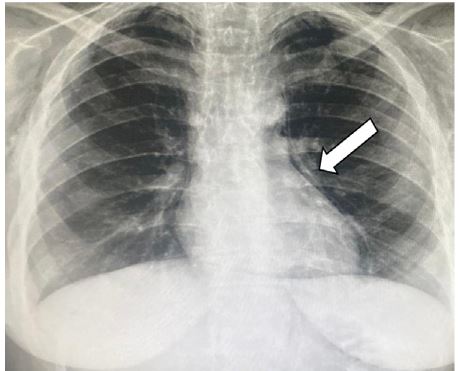
Figure2: Chest X-ray showing pneumomediastinum and subcutaneous emphysema.
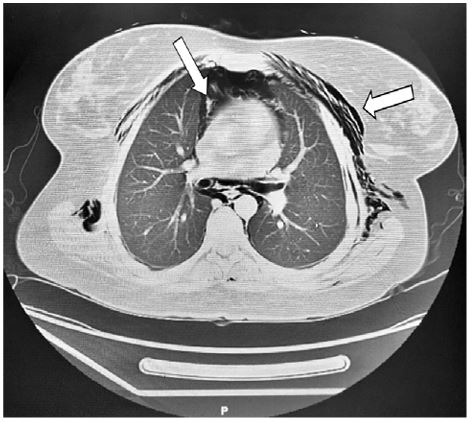
Figure 3: CT-scan chest demonstrating subcutaous emphysema.
Discussion
Subcutaneous emphysema (SE) is air infiltration in the skin’s subcutaneous layer. The development of SE indicates that air is occupying a deeper body region [7]. Air preferentially accumulates in the subcutaneous region with minor tension until the pressure increases enough to travel along another plane, leading to extensive spread [8]. The level of surgical emphysema can vary from mild subcutaneous emphysema to severe life-threatening airway compression, pneumomediastinum, and pneumothorax complications [9]. Subcutaneous emphysema and pneumomediastinum are infrequent post-operative presentations ofsleeve gastrectomy; this was especially notable in our patient sincesheunderwent uneventful post-operative recovery and was discharged and followed up two weeks after surgery. Nevertheless, her recent events of excessive forceful vomiting and retching led to the development of SE.
Aberrant air in the mediastinum and subcutaneous regions can originate from the oesophagus, lungs, airways, neck, and abdominal cavity [10] when (SE) and pneumomediastinum form spontaneously. The two most likelycauses are alveolar rupture or oesophageal rupture called Boerhaave’s syndrome (BS) [11]. The mechanism of alveolar rupture in vomiting appears to be abdominal contraction against a closed glottis, resulting in increased intra-alveolar pressure. On the other hand, oesophageal ruptures occur due to excessive vomiting and retching, leading to increased intra-luminal pressure of the oesophagus, subsequently exceeding the wall’s tensile strength [12]. Both conditions are associated with symptoms such as retrosternal chest pain, cough, sore throat, dysphonia, dysphagia, palpitation, neck discomfort, and dyspnoea [13]. However, BS patients present with a classic triad of vomiting, chest pain, and subcutaneous emphysema (Mackler’s triad) and are generally septic due to mediastinitis.
The diagnosis of (SE) and pneumomediastinum can be difficult due to its delayed presentation and vague symptoms. After a careful medical history and detailed physical examination, it is vital to exclude other diseases with a similar presentation, such as ischemic heart attack, pulmonary embolism, pericarditis, musculoskeletal disorders, and chest infections. The X-ray of the chest is a helpful tool to diagnose this condition. Reliable signs on posterior chest X-rays include the separation of the mediastinal pleura from the left heart border and subcutaneous emphysema [14]. X-rays are also abnormal in 90% of cases of BS with additional signs, including left pleural effusion and hydropneumothorax [15]. Water-soluble swallow and diluted barium studies help to exclude perforation of the oesophagus; however, a false-negative result occurs in 26–66% of all patients [16]. Computer tomography (CT) scans with oral contrast are helpful when the diagnosis is questionable, as well as a diagnosis of perforation in the oesophagus.
The management of SE involves the determination of the underlying cause, analgesia, rest, and reassurance. Furthermore, patients may require antibiotics as a prophylaxis to prevent mediastinitis. Subcutaneous emphysema is typically a self-limiting condition once the diagnosis is confirmed [17]. Most presentations last a few days, including a hospital stay, as in our case report. Nevertheless, some authors suggest that hospitalization is not always required. Possible complications are tension pneumothorax, tension pneumomediastinum, air embolism, and pneumopericardium, although these are all rare [13].
Conclusions
Spontaneous emphysema is a unique manifestation of post-sleeve gastrectomy. It is usually a self-limiting disorder that can be established when other more severe conditions have been excluded, such as oesophageal rupture, whichcan be lethal. To avoid future complications, it is critical to report these cases to identify others in a timely manner.
References
- DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007; 356: 2176-83.
- Online source: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight Access. 2020.
- Hoyuela C. Five-year outcomes of laparoscopic sleeve gastrectomy as a primary procedure for morbid obesity: A prospective study. World J Gastrointest Surg. 2017; 9(4): 109-117. [DOI:10.4240/wjgs.v9.i4.109].
- Online source: https://asmbs.org/resources/metabolic-and-bariatric-surgery.
- Kheirvari M, Dadkhah Nikroo N, Jaafarinejad H, et al. The advantages and disadvantages of sleeve gastrectomy; clinical laboratory to bedside review. Heliyon. 2020; 6(2): e03496. [DOI:10.1016/j.heliyon.2020.e03496].
- Woźniewska P, Diemieszczyk I, Hady HR. Complications associated with laparoscopic sleeve gastrectomy - a review. Prz Gastroenterol. 2021; 16(1): 5-9. [DOI:10.5114/pg.2021.104733].
- Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984; 144(7): 1447-1453.
- Dixit R, George J. Subcutaneous emphysema in cavitary pulmonary tuberculosis without pneumothorax or pneumomediastinum. Lung India. 2012; 29(1): 70-72. [DOI:10.4103/0970-2113.92369].
- Barengo JH, Yuen SN, Kennedy P, Shott SR. Subcutaneous emphysema with pneumomediastinum after tonsillectomy: Case report and review of the literature. Int J PediatrOtorhinolaryngol. 2020; 131: 109885. [DOI:10.1016/j.ijporl.2020.109885].
- Panacek EA, Singer AJ, Sherman BW, Prescott A, Rutherford WF. Spontaneous pneumomediastinum: clinical and natural history. Ann Emerg Med. 1992; 21(10):1 222-1227.[DOI:10.1016/s0196-0644(05)81750-0].
- Forshaw MJ, Khan AZ, Strauss DC, Botha AJ, Mason RC. Vomiting-induced pneumomediastinum and subcutaneous emphysema does not always indicate Boerhaave's syndrome: report of six cases. Surg Today. 2007; 37(10): 888-892. [DOI:10.1007/s00595-006-3493-1].
- Schwartz M, Rossoff L. Pneumomediastinum and bilateral pneumothoraces in a patient with hyperemesis gravidarum. Chest. 1994; 106(6): 1904-1906. [DOI:10.1378/chest.106.6.1904].
- Langwieler TE, Steffani KD, Bogoevski DP, Mann O, Izbicki JR. Spontaneous pneumomediastinum. Ann Thorac Surg. 2004; 78(2): 711-713. [DOI:10.1016/j.athoracsur.2003.09.021].
- Lillard RL, Allen RP. The extrapleural air sign in pneumomediastinum. Radiology. 1965; 85(6): 1093-1098. [DOI:10.1148/85.6.1093].
- Pate JW, Walker WA, Cole FH Jr, Owen EW, Johnson WH. Spontaneous rupture of the esophagus: a 30-year experience. Ann Thorac Surg. 1989; 47(5): 689-692. [DOI:10.1016/0003-4975(89)90119-7].
- Koullias GJ, Korkolis DP, Wang XJ, Hammond GL. Current assessment and management of spontaneous pneumomediastinum: experience in 24 adult patients. Eur J Cardiothorac Surg. 2004; 25(5): 852-855. [DOI:10.1016/j.ejcts.2004.01.042].
- Jougon JB, Ballester M, Delcambre F, Mac Bride T, Dromer CE, Velly JF. Assessment of spontaneous pneumomediastinum: experience with 12 patients. Ann Thorac Surg. 2003; 75(6): 1711-1714. [DOI:10.1016/s0003-4975(03)00027-4].

