Case Report - Volume 2 - Issue 6
Minimally invasive esophagectomy for cancer in a patient with giant paraesophageal hernia
N Daniel Velasco Hernández*; Héctor Raúl Horiuchi; María Micaela Zicavo
Department of Surgery of Diagnostic Institute of La Plata City. National University of La Plata, Buenos Aires, Argentina.
Received Date : Nov 09, 2022
Accepted Date : Dec 08, 2022
Published Date: Dec 30, 2022
Copyright:© N Daniel Velasco Hernández 2022
*Corresponding Author : N Daniel Velasco Hernández, Department of Surgery of Diagnostic Institute of La Plata City. National University of La Plata, Buenos Aires, St 8 N° 2877 Berisso, Buenos Aires, Argentina.
Email: daniels84@hotmail.com
DOI: Doi.org/10.55920/2771-019X/1335
Abstract
Minimally invasive esophagectomy in prone position is a procedure during which the patient is placed in a prone position during the thoracoscopic approach. A 67-year-old male patient consulted whit giant paraesophageal hernia and esophageal cancer. The treatment should be focused on the oncological resection of the esophagus despite the technical difficulties caused by the presence of a large hernia. A minimally invasive approach in the prone position and laparoscopic hernia repair can be considered an appropriate option for the resolution of both diseases with satisfactory results.
Keywords: Minimally invasive esophagectomy; Giant paraoesophageal hernia; Esophageal cancer.
Introduction
Minimally invasive esophagectomy in prone position is a procedure during which the patient is placed in a prone position during the thoracoscopic approach. The first experiences were published by Cuschieri et al. in 1994 who described this approach to access the posterior mediastinum and the esophagus for mobilization and resection [1,2]. Giant hiatal hernias are more common in older patients and can significantly reduce their quality of life [3]. The objective is to present a patient who underwent minimally invasive esophagectomy for cancer with a giant paraesophageal hernia. We reported and checked this case based on SCARE guidelines [4].
Case report
A 67-year-old male patient who consulted for thoracic pain, progressive dysphagia, and weight loss. Upper gastrointestinal endoscopy was performed, which revealed a raised ulcerated lesion at the lower esophagus, from which biopsies were taken. The pathology report revealed the presence of invasive differentiated adenocarcinoma. Thoraco-abdominal computed tomography was performed, which showed a giant paraesophageal hernia and tumor of the lower esophagus, and PET CT was performed to rule out distant disease and ultrasound endoscopy to see parietal infiltration. It was staged as T2N0MO according to the 8th edition of the AJCC. A surgical approach was decided, and minimally invasive esophagectomy was performed in the prone position. Technique Thoracic stage: The patient is positioned in prone position, with both arms extended. Two devices are used to provide support on the upper chest and pelvis for an adequate excursion of the diaphragm and ventilation. Three ports are introduced: a 10-mm port at the level of the tip of the scapula, a 5-mm trocar at the level of the 4th or 5th intercostal space, approximately 7 cm from the spine, and a 10mm port for the left hand at the ninth intercostal space, 7 cm from the spine. We used normal intubation with 8 mm Hg carbon dioxide insufflation. Once the camera has been introduced, the thoracic vertebrae are visualized and a huge hernia sac; the mediastinal pleura is opened, the azygos arch is cut, followed by total mobilization of the esophagus and resection of the sub-carinal lymph nodes. Image N°1,2and3.
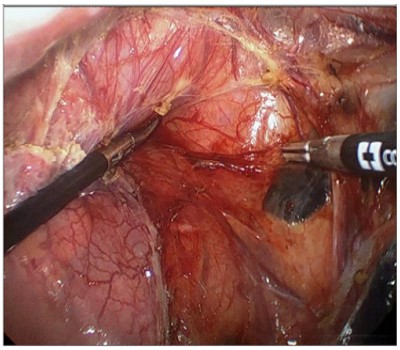
Image N°1: Prone position view. Dissection of the paraesophageal hernia sac.
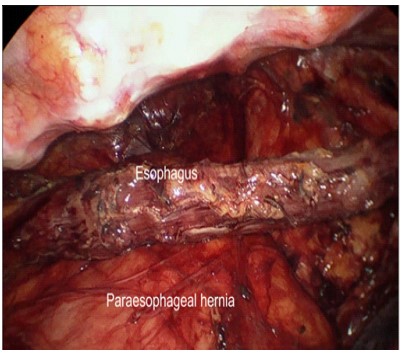
Image N⸰2: Complete esophageal dissection
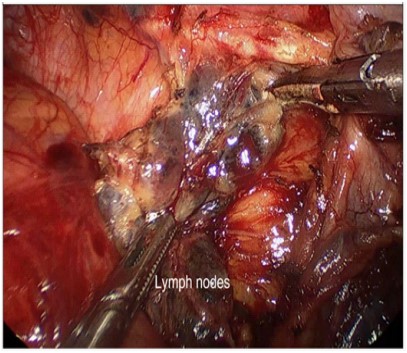
Image N⸰3: Subcarinal lymph nodes dissection.
Abdominal stage: the patient is repositioned to the supine position. The surgeon takes place between the legs, the first assistant on the right side of the patient, and the second assistant on the left side of the patient. The procedure starts complete reduction of the hernial sac, stomach, and associated herniated structures and opening of the greater omentum and continues along the greater curvature, preserving the right gastro-epiploic vessels that will provide irrigation to the gastroplasty. Lymph nodes from the celiac trunk are then dissected. An interrupted non-absorbable suture was applied for crus closure and as an additional reinforcement, the mesh was fixed with absorbable tacks. Image N°4 and5.
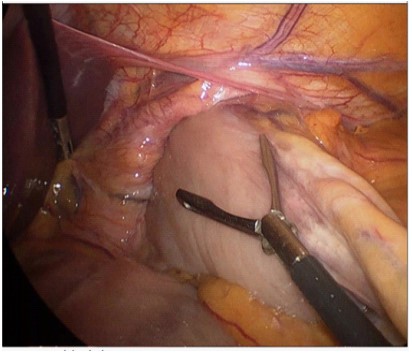
Image N⸰4: Abdominal stage.
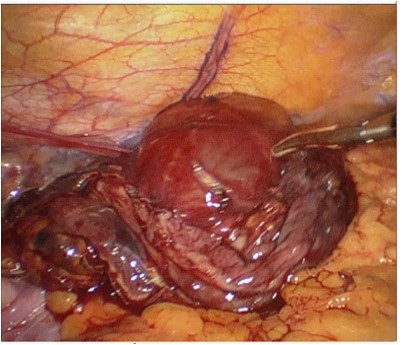
Image N⸰5: Hernia sac resection
After the mobilization of the stomach, the cervical esophagus is dissected, and the specimen is removed through a mini supraumbilical midline laparotomy. At this level, the gastric conduit is constructed using a mechanical stapler (hybrid technique). Then, the gastric conduit is pulled up through the mediastinum and an anastomosis is performed with the cervical esophagus (McKeown procedure) [5]. The patient evolved favorably and he was discharged on the eighth postoperative day. The pathology report revealed: semi-differentiated adenocarcinoma with adenocarcinoma metastasis in one right paracardial lymph node of 18 examine; PT3 N1 Mx.
Discussion
Prone position for the minimally invasive procedure has been proposed as an alternative to the lateral approach due to decreased pulmonary morbidity, better surgeon ergonomics, operative exposure, and higher lymph node yield due to better exposure of the sub-carinal space. The most important disadvantage is the difficulty generated by this position in case a rapid conversion is needed [5,6]. A giant paraesophageal hernia is an uncommon situation in which more than 50% of the stomach protrudes into the chest cavity. The association between this type of hernia and cancer is not frequent due they are usually very symptomatic, which requires their resolution as soon as the diagnosis is made [7,8]. The treatment should be focused on the oncological resection of the esophagus despite the technical difficulties caused by the presence of a large hernia [9]. A minimally invasive approach in the prone position and laparoscopic hernia repaircan be considered an appropriate option for the resolution of both diseases with satisfactory results.
Conflict of interest: The authors declare that they have no conflict of interest.
References
- Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C. Minimallyinvasiveversusopenoesophagectomy for patients with oesophageal cancer: a multicentre, open label, randomised controlled trial. Lancet. 2012; 379: 1887-92.
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, Mc-Caughan JS, Litle VR, et al. Minimally invasive esophagectomy. Outcomes in 222 patients. Ann Surg. 2003; 238: 486-94.
- Luketich JD et al. Laparoscopicrepair of giant paraesophageal hernia: 100 consecutive cases.Ann Surg. 2000; 232(4): 608-18.
- RA Agha, AJ Fowler, A Saeta, I Barai, S Rajmohan, DP Orgill. The SCARE statement: consensus-based surgical case report guidelines, Int. J. Surg. 2016.
- Shen Y, Zhong M, Wu W, Wang H, Feng M, et al. The impact of tidal volume on pulmonary complications following minimally invasive esophagectomy: a randomized and controlled study. J Thorac Cardiovasc Surg. 2013; 146: 1267-73.
- June S Peng, Moshim Kukar, Gary N Mann, Steven N Hochwald. Minimally Invasive Esophageal Cancer Surgery. urg Oncol Clin N Am. 2019; 28(2): 177-200.
- Mitiek MO, Andrade RS. Gianthiatal hernia.Ann Thorac Surg. 2010; 89(6): S2168-73.
- LePage PA, Furtado R, Hayward M, Law S, Tan A, Vivian SJ, et al. Durability ofgiant hiatus herniarepair in 455 patients over 20 years. Annals of the Royal College of Surgeons of England. 2015; 97(3): 188.
- Differences in esophageal cancer surgery in terms of surgical approach and extent of lymphadenectomy: Findings. A. S. van Rijswijk. Ann Surg Onco. [DOI: 10.1245/s10434-019-07316-9].

