Case Report - Volume 3 - Issue 1
Osteoarthritis of the ankle revealing disseminated tuberculosis
M Rimaoui1*; M soussi2; F Marnissi3; S Chiheb1
1Department of dermatology, CHU Ibn Rochd, Casablanca, Morocco.
2Department of bacteriology, CHU Ibn Rochd, Casablanca, Morocco.
3Department of pathological anatomy, CHU Ibn Rochd, Casablanca, Morocco.
Received Date : Nov 10, 2022
Accepted Date : Dec 12, 2022
Published Date: Jan 03, 2023
Copyright:© M Rimaoui 2023
*Corresponding Author : M Rimaoui, Department of dermatology, CHU
Ibn Rochd, Casablanca, Morocco.
Email: maryemrimaouip1@gmail.com
DOI: Doi.org/10.55920/2771-019X/1338
Introduction
Tuberculosis is a major public health problem. It has a high annual incidence in Africa and Asia. The estimated number of new cases of tuberculosis is constantly increasing. The estimated number of new cases of tuberculosis (TB) is constantly increasing and will reach 10 million in 2019 [1]. Osteoarticular tuberculosis is rare and represents only 10-15% of extrapulmonary localisations. It is most often the result of haematogenous dissemination of BK. Extension to adjacent soft tissues with formation of cold abscesses is also observed. Its main location is in the axial region, which accounts for about 50% of cases [2]. Localization in the peripheral joints is less frequent. Tuberculous osteoarthritis of the ankle is very rare [3]. We report an original observation of an immunocompetent patient who developed disseminated tuberculosis with an osteoarticular origin, confirmed by the detection of the tuberculosis complex genome in synovial and bone tissue.
Case report
The patient was 40 years old and had a recent tuberculosis infection with a fatal outcome (death of the two brothers due to untreated pulmonary and lymph node tuberculosis). He consulted for a painful swelling of the ankle that had been evolving for 2 years in a context of anorexia, weight loss and apyrexia. The clinical examination revealed a circumferential swelling of the ankle, renitcent, sensitive with multiple fistulised nodular lesions emitting pus and serosities. The biology revealed an inflammatory syndrome (CRP at 170 mg/L and hyperleukocytosis at 15,000 elements/mm 3); a hypochromic and microcytic anaemia at 9.7 g/dL and lymphopenia at 970. The fasting blood glucose level and HIV serology were within the norm. The ankle X-ray showed osteocondensation and pinching of the tibial-astragalar joint space. The ankle CT scan showed distal tibioperoneal osteoarthritis, intra-articular talocrural joint effusion and chronic synovitis. hese lesions were associated with a soft tissue collection in the ankle. All the clinical and radiological findings suggested tuberculosis. A surgical bone and synovial biopsy was performed and concluded to be granulomatous dermatitis with the presence of Mycobacterium tuberculosis DNA on PCR. The lesion assessment including a thoracic-abdominal-pelvic CT scan showed a diffuse micronodular infiltrate in both lung fields and a fluid collection in contact with the parietal pleura measuring 55*34mm. The diagnosis of disseminated tuberculosis was retained. A quadritherapy of rifampicin, isoniazid, pyrazinamide and ethambutol was initiated for 2 months, followed by a dual therapy of rifampicin and isoniazid for 8 months. Orthopaedic immobilisation with a posterior splint and limitation of physical activity was recommended. Surgical treatment was not considered necessary. The evolution was slowly favourable.
Discussion
Morocco is a tuberculosis endemic country. Despite ministerial efforts, the incidence is constantly increasing. In 2015, 30,636 cases were reported; a total of 656 cases died of tuberculosis [4]. Its anatomical polymorphism and the difficulty of isolating the pathogen make its diagnosis difficult. Its treatment must be rapid and effective in order to prevent the emergence of drug-resistant forms. Extra-pulmonary tuberculosis accounts for 10% of all tuberculosis cases. Bone involvement is the fifth most common site, mainly involving the spine. Tuberculous osteoarthritis of the ankle is rare. This location often results from haematogenous dissemination from a primary infection site, for which the role of local trauma has been suggested [5]. The clinical picture is insidious. A diagnostic triad is often present: pain, swelling and joint limitation. The presence of systemic symptoms such as fever, sweating and anorexia are inconstant [6]. In our patient, the recent tuberculosis infection, the systemic signs and the insidious chronic monoarthritis were in favour of tuberculosis. The cutaneous localization adjacent to an osteoarticular site is frequent in the form of scrofuloderma. This can be explained by endogenous contamination. Hematogenous dissemination in our patient is likely due to the disseminated nature of the infection.
The diagnosis is the result of the constellation of clinical, radiological and histological elements. Indeed, the standard radiograph is quite normal at the beginning. Images of bone destruction and osteolysis can be seen in the advanced stages. The CT scan provides an accurate assessment of the bone lesions and shows signs of osteopenia, marginal erosions, soft tissue calcifications, cartilage destruction and geodes. Magnetic resonance imaging (MRI), the test of choice, can provide early evidence of synovitis, soft tissue collections, joint effusion, granulation tissue and synovial thickening [7]. Culture is currently the gold standard. Other tests have been developed more recently, namely nucleic acid amplification techniques that allow rapid identification of MTB as well as rapid assessment of susceptibility to rifampicin [8]. The treatment of tuberculosis of the bone consists of two elements. The medical part is based on antibacillary chemotherapy for a period of 9 months and the orthopaedic component is based on the resting of the joint and the correction of deformities.

Figure 1: Ankle swelling and scrofuloderm lesions.
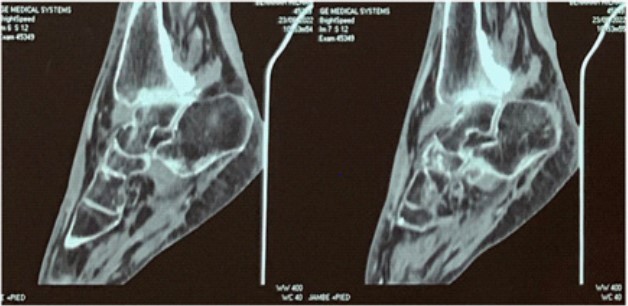
Figure 2: Coronal section of foot showing tibiofibular osteoarthritis.
Conclusion
We report a rare case of ankle arthritis revealing disseminated tuberculosis in an immunocompetent patient. Articular tuberculosis can mimic different joint pathologies. Any delay in diagnosis and treatment can be life threatening. We emphasise that in case of uncertainty about the diagnosis of chronic monoarthritis, an early surgical biopsy should be mandatory.
Conflicts of interest: I declare that I have no conflicts of interest.
References
- Cords O, Martinez L, Warren JL, O’Marr JM, Walter KS, Cohen T, et al. Incidence and prevalence of tuberculosis in incarcerated populations: a systematic review and meta-analysis. Lancet Public Health. 2021; 6(5): e300‑8.
- Martini M, Ouahes M. Bone and Joint Tuberculosis: A Review of 652 Cases. Orthopedics. 1988; 11(6): 861‑6.
- Ostéo-arthrite chronique de la cheville révélatrice d’une tuberculose pulmonaire. Rev PneumolClin. 2016; 72(3): 214‑7.
- Sadeq M, Bourkadi JE. Spatiotemporal distribution and predictors of tuberculosis incidence in Morocco.Infect Dis Poverty. 2018; 7(1): 43.
- Benchanna R, Benjelloune A, Abdelafatah Z, Arsalane A, Janah H, Oujaber J, et al. L´arthrite tuberculeuse isolée du genou, un diagnostic difficile chez l’adolescent: rapport de cas. Pan Afr Med J [Internet]. 2020; 37(225). Disponible sur: https://www.panafrican-med-journal.com/content/article/37/225/full
- Basnayake O, Mathangasinghe Y, Nihaj A, Pitagampalage R, Jayarajah U, Gunawardena K, et al. Tuberculosis presenting as arthritis of the ankle: A case report. SAGE Open Med Case Rep. 2021; 9: 2050313X211035574.
- Natsis K, Grammatikopoulou D, Kokkinos P, Fouka E, Totlis T. Isolated tuberculous arthritis of the ankle: a case report and review of the literature. Hippokratia. 2017; 21(2): 97‑100.
- Saktiawati AMI, Putera DD, Setyawan A, Mahendradhata Y, Werf TS van der. Diagnosis of tuberculosis through breath test: A systematic review. eBioMedicine. 2019; 46: 202‑14.

