Case Report - Volume 3- Issue 1
Regional aggressive cervical root resorption in a young female adult
Inger Kjaer*
Department of Odontology Faculty of Health and Medical Sciences University of Copenhagen Denmark.
Received Date : Nov 11, 2022
Accepted Date : Dec 13, 2022
Published Date: Jan 04, 2023
Copyright:© Inger Kjær 2023
*Corresponding Author : Inger Kjaer, Department of Odontology, Faculty of Health and Medical Sciences, University of Copenhagen, Denmark.
Email: ik@sund.ku.dk
DOI: Doi.org/10.55920/2771-019X/1339
Introduction
In a former study it was demonstrated in two clinical cases, that regional aggressive cervical resorption was caused by neuronal virus infection in the jaws during early childhood [1]. Virus infection can spread along the peripheral nerves, illustrated schematically on a panoramic radiograph with peripheral nerves innervating different tooth groups [2], as demonstrated in (Figure 1).
Case report
The first case in the former study [1] demonstrated cervical resorptions in the right maxillary incisors. These resorptions were caused by a meningitis virus attack between the ages of 8 to 9 years. An impaired sensitivity in the skin was observed in an area extending from the right prolabium to the right medial and lateral crus of the external nose. This change in skin sensitivity began between 8 and 9 years of age. The teeth adjacent were not affected in the resorption process. It was suggested, that the meningitis virus had spread along the right naso palatine nerve, innervating the skin and the right incisors. Follow up examinations demonstrated, that the destructive process was limited to the region, innervating the right incisors (Figure 1).
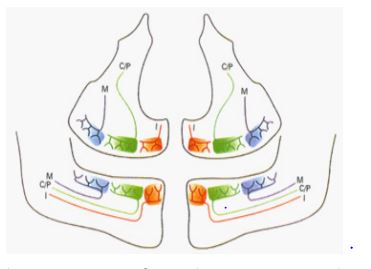
Figure 1: Schematic overview of an orthopantomogram with nerves to the different tooth groups (fields). Red: Nerves to incisors, I, green: Nerves to the canines/premolars, C/P, and blue: Nerves to the molars, M.
The second case demonstrated cervical resorptions in the entire left maxilla and in two right mandibular incisors. In the maxilla a stepwise spreading had occurred, starting in the first molar and second premolar. This destructive process arrested at the maxillary midline. This second case demonstrated neurogene spreading of the pertussis virus, according to the innervate on pattern (Figure 1). The child was hospitalized for three months at the age of 9 years, due to whooping cough and sequelae. Several years of observation documented that the resorption processes were not spread further to other innervation regions.
The present case
The present case is demonstrated by radiographs from a young female adult. The radio graphs were forwarded to the author at the Department of Odontology for diagnostics and treatment guidance. Contact to the referring dentist was limited.
Radiographs
(Figure 2) illustrates the first radiographs received. At that stage, the patient was 22 years of age. It demonstrates cervical resorptions in the left maxillary first and second molars. Immediate treatment was recommended.
(Figure 3) demonstrates an orthopantomogram taken a few weeks after the radiograph, demonstrated in (Figure 2). The indication for this radiograph was to investigate if cervical resorption occurred in other teeth in the dentition. The orthopantomogram demonstrated that cervical resorption occurred only in the two left maxillary molars, illustrated in (Figure 2).
(Figure 4) demonstrates, at the age of 23 years, that the second molar had been extracted, and that the first molar had been end odontically treated. Resorption had not spread to other teeth in the dentition. (Figure 5) demonstrates, at the age of 24 years, that the first molar has also been extracted. Resorption did not appear on the third molar or in the second premolar.

Figure 2: Radiograph from a young patient, 22 years of age, demonstrating cervical resorptions in the maxillary first and second molars.

Figure 3: Orthopantomogram taken a few weeks after the radiograph I Figure 2. The orthopantomogram demonstrated that cervical resorption occurred only in the two left maxillary molars.

Figure 4: Orthopantomogram taken at the age of 23 years. Now the second molar has been extracted, and the first molar has been endodontically treated. Resorption has not spread to other teeth.
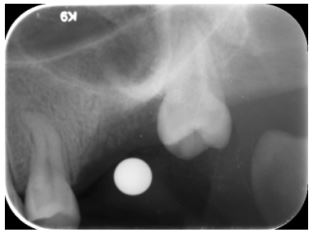
Figure 5: Dental film taken at the age of 24 years. Now also the first molar has been extracted. Resorption did not appear on the third molar or in the second premolar.
Evaluation and discussion
There was not direct contact between the author and the patient, and anamnestic information from the referring dentist to the author was lacking, at the time of reference. It was hypotisized, that this case in agreement with the two cases published [1] had cervical resorption after a bacterial or virus attack. The referring dentist informed the author, when the patient was 24 years of age, that septicemia had occurred with severe skin affections of the entire body, when the patient was 7 years of age. The infection was caused by bordetelia pertussis bacteria and treated with antibiotics. The third molar might have been formed after the age of 7 years, at the time for recovering after infection. This could explain why the third molar was not affected by cervical resorption. The case demonstrates how fast acervical resorption can progress and destroy the whole dentition, shortly after having been diagnosed. There was no spreading of bacterial attack to the premolars, belonging to another innervation field (See Figure 1).
It was not possible to acquire a later radiograph from the actual patient. The last radiograph (Figure 5), demonstrates that cervical resorption was not diagnosed in the left third molar. The purpose of demonstrating this case, and informing about further two cases, is to focus on how the regional spreading of
cervical resorption within innervation fields can occur and be of importance for immediate treatment.
It is interesting to observe that the initial sites of cervical resorption in the present case was within the molar field. In the former first case demonstrated, the initial sites of cervical resorption was within an incisor field. In both cases, the resorption was not spread outside the initial fields. The former second case referred demonstrated initial involvement of two fields, followed by a more severe spreading in several fields. This information might be of importance for predicting spreading of cervical resorption processes and for early treatment.
The etiology behind the cervical resorption process is not known. The root resorption process has been explained from the composition of the periodontal membrane [4]. The cervical onset of the destructive resorption process has also focused on gaps in the cementum at the enamel/cementum junction, leaving the underlying mineralized dentine exposed for osteoclastic activity in the dentine [6]. The aggressive resorption reported in this case, and in the two cases formerly published [1], seems to be the first cases on column resorption with an etiology based on the innervation layer in the periodontal membrane [7]. The innervation layer occurs closest to the root surface, and the cervical gingival area might be specifically rich in innervation.
Acknowledgements: Thanks to departmental secretaries Linda Michelsen and Eva Reinwald for manuscript preparation.
References
- Kjær I, Strøm C, Worsaae N. Regional aggressive root resorption caused by neuronal virus infection. Case Reports in Dentistry. 2012.
- Kjær I. Prenatal traces of aberrant neurofacial growth. Acta Odontol Scand. 1998; 56: 326-30.
- Kjær I. Etiology-bases dental and craniofacial diagnostics. Wiley & sons ltd. Blackwell. 2017.
- Kjær I. External root resorption - different aetiologies explained from the composition of the human root-close peri-odontal membrane.Hypotheses. 2013; 4: 75-9.
- Kjær I. Root resorption-focus on the heredity behind this destructive process. EC Dental Science. 2022: 55-63.
- Patel S, Kanagasingam S, Ford TP. External cervical resorption: a review. Journal of Endodontics. 2009; 35(5): 616-25.
- Kjær I, Nolting D. The human periodontal membrane - focusing on the spatial interrelation between the epithelial layer of Malassez, fibers, and innervation. Acta Odontol Scand. 2009; 67: 134-8.

