Clinical Image - Volume 3 - Issue 1
Ossification of the lumbar posterior longitudinal ligament and lumbago
Khadija Laasri*; Salma Marrakchi; Zakia El yousfi; Jamal El fenni; Issam En nafaa
Department of Radiology, Mohammed V military teaching Hospital, Mohammed V University, Rabat, Morocco.
Received Date : Nov 07, 2022
Accepted Date : Dec 16, 2022
Published Date: Jan 06, 2023
Copyright:© Khadija Laasri 2023
*Corresponding Author : : Khadija Laasri, Department of Radiology, Mohammed V military teaching Hospital, Mohammed V University, Rabat,Morocco.
Email: kadijalaasri93@gmail.com
DOI: Doi.org/10.55920/2771-019X/1341
Abstract
Ossification of the posterior longitudinal ligament (OPLL) is a condition of abnormal calcification of the posterior longitudinal ligament, mostly found in men, the elderly, and Asian patients, hence the name Japanese disease. The cervical spine area is the most typical location (75%), but can also affect the thoracic (15%) or lumbar (10%) spine. The spinal cord can be compressed by this lesion, which can cause neurological deficits. The treatment of choice for patients with symptomatic OPLL is surgery to relieve spinal cord compression. We report an exceptional case of lumbar ossification of the OPLL in a Moroccan patient.
Keywords: Ossification; posterior longitudinal ligament; spine.
Clinical history
A 45-year-old woman with no previous pathological history who was referred to the physical medicine unit for lumbago that had been evolving for 9 months and was interfering with sitting and activities of daily living. There was no vesicosphincter disorder, nor limitation of walking perimeter. The neurological examination and peripheral joints were normal. Standard radiographs of the lumbar spine showed ossification of the lumbar posterior longitudinal ligament at the D12 and L1 level. The CT scan of the lumbar spine confirmed calcification of the lumbar posterior longitudinal ligament at the D12 and L1 with a mass effect on the canal content, essentially in the left posterior-para-medial region. The etiological and phosphocalcic workup was negative. A decompression laminectomy of the lumbar spine and an excision of the ossification were performed followed by an adapted rehabilitation. The evolution was favorable with complete disappearance of the symptoms.
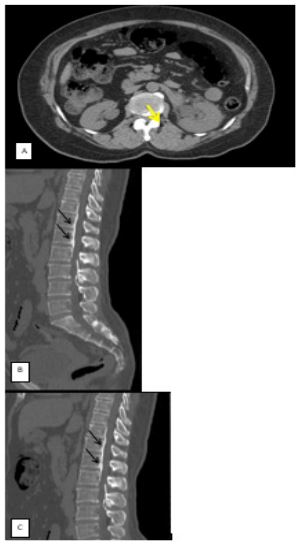
Figure: CT scan of the lumbar spine: A) in axial section: ossification of the posterior common vertebral ligament at D12 and L1 (yellow arrow); B and C) in sagittal plane reconstruction: hyper-density of the posterior common vertebral ligament at D12 and L1 (black arrow).
Discussion
Ossification of the posterior longitudinal ligament (OPLL) is most commonly found in men, the elderly, and Asian patients. OPLL can be associated with other musculoskeletal diseases such as diffuse idiopathic skeletal hyperostosis, ankylosing spondylitis, and other spondyloarthropathy. The pathogenesis of OPLL is still unclear, but several factors have been reported to be associated with OPLL formation and progression, including genetic, hormonal, environmental, and lifestyle factors [1,2]. Clinical presentation of OPLL depends on the size of the OPLL, spinal canal diameter, and range of motion of the spine. Although patients are asymptomatic, others present with neurological deficits such as radiculopathy, myelopathy, and in severe cases, bowel and bladder symptoms. Despite symptoms often appear gradually, but there are also some reports of patients with trauma-induced sudden onset myelopathy [2]. Plain radiography, CT, and MR imaging are used to evaluate OPLL extension and the area of spinal cord compression. Plain radiography is the simplest method to detect OPLL, showing ossification of the ligament behind the vertebrae alone (segmental), behind the vertebrae including the intervertebral disc spaces (continuous), and combinations of the segmental and continuous variants and OPLL opposite disc spaces alone, but it has some limitations especially in the early stages of the disease. Both magnetic resonance imaging (MRI) and computed tomography (CT) examinations are critical. MRI better delineates the extent of soft tissue abnormalities in three dimensions, including the cervicothoracic junction, whereas CT more readily identifies the foci of frank ossification [3,4,5]. Management of OPLL depends on the degree of symptoms. When symptoms are mild and non-progressive, conservative treatments and periodic observations are good enough, but once symptoms of myelopathy are present and neurologic symptoms are progressive, the treatment of choice is surgery to relieve spinal cord compression [2].
Author’s Contributions: All authors contributed to this work. All authors have read and approved the final version of the manuscript.
Conflicts of Interest: The authors declare that there are no conflicts of interest regarding the publication of this paper
References
- Saetia K, Cho D, Lee S, Kim DH, Kim SD. Ossification of the posterior longitudinal ligament: a review. Neurosurgical Focus. 2011; 30(3): E1. [DOI:10.3171/2010.11.focus10276].
- Byung-Wan Choi, Kyung-Jin Song, Han Chang. Ossification of the Posterior Longitudinal Ligament: A Review of Literature. Asian Spine J. 2011; 5(4): 267-276.
- Epstein N. Diagnosis and surgical management of cervical ossification of the posterior longitudinal ligament. The Spine Journal. 2002; 2(6): 436-449. [DOI:10.1016/s1529- 9430(02)00394-7].
- Wu D, Liu CZ, Yang H, et al. Surgical interventions for cervical spondylosis due to ossification of posterior longitudinal ligament: a meta-analysis. Medicine (Baltimore). 2017; 96: e7590.
- Saetia K, Cho D, Lee S, Kim DH, Kim SD. Ossification of the posterior longitudinal ligament: a review. Neurosurgical Focus. 2011; 30(3): E1. [DOI:10.3171/2010.11.focus10276].

