Case Report - Volume 3 - Issue 1
Traumatic Phacocele: A case report
Chiguer S*; AitElhajj J; Elbelhadji I; Mchachi A; Benhmidoune L; Rachid R; Elbelhadji M
Department of Adult Ophthalmology, 20 Août 1953 Hospital/IbnRochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco.
Received Date : Nov 14, 2022
Accepted Date : Dec 22, 2022
Published Date: Jan 12, 2023
Copyright:© Chiguer S 2023
*Corresponding Author : Chiguer S, Department of Adult Ophthalmology, 20 Août 1953 ospital/IbnRochd University Hospital, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco.
Email: selma.chiguer@hotmail.fr
DOI: Doi.org/10.55920/2771-019X/1346
Abstract
Most cases of phacocele are secondary to a blunt trauma, associated with a risk factor like advanced age, surgery, or systemic diseas affecting scleral rigidity. We report the case of a 76-year-old patient admitted for a subconjunctival dislocation of the crystalline lens after a blunt trauma, without other associated ocular lesions, managed with extraction of the crystalline and a secondary implantation, with an amelioration of the visual acuity.
Introduction
Contusive ocular trauma is very frequent in our context, often secondary to aggression, professional or domestical accidents [1]. These contusive traumas can cause lesions on all tissues of the eye [2]. The lens is an organ frequently affected by contusive trauma due to anteroposterior and longitudinal forces, causing either cataract or crystalline dislocation, these dislocations are often in the anterior chamber or in the posterior segment [3], subconjunctival lens dislocation remains an uncommon complication [4]. We report the case of a 76 year old patient with no pathological history who was admitted to theophtalmological emergency for subconjunctival lens dislocation secondary to a blunt trauma in the context of a domestic accident. This type of crystalline dislocation is very rare, especially without any underlying pathology [5].
Case Report
A 76-year-old patient, pseudophakic of the left eye for 5 months without incident, admitted for management of a contusive ocular trauma by a blunt object 24 hours before his admission. The ophthalmological examination of the traumatized eye, the right eye, found hand motion as best correted visual acuity, an ocular tone at 12 mmHg, a lens dislocated subconjunctivally in the supra-nasal area without conjunctival effraction or chemosis or subconjunctival hemorrhage (Figure 1), The rest of the examination revealed a minimal corneal edema, vitreous in the anterior chamber with an hyphema stade 1, aphakia and a difficult fundus examination. The examination of the left eye revealed a corrected visual acuity at 8/10, a crystalline implant in place with no abnormalities on the rest of the examination.

Figure 1: Traumatic subconjunctival crystalline lens dislocation.
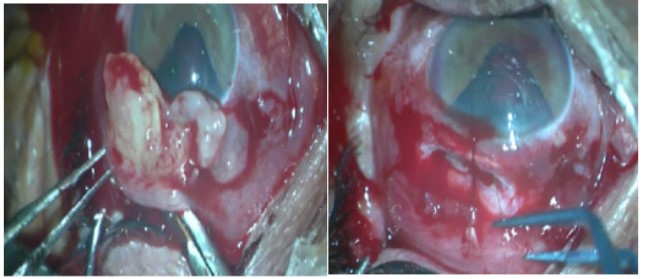
Figure 2: Extraction of the crystalline nucleus by the scleral effraction.
The surgical exploration found an arciform scleral effraction of 3 to 4 mm in superior-nasal quadrant 2 mm of the limbus with a crystalline nucleus and masses in subconjunctival, we proceeded to the ablation of the crystalline lens and masses, with an anterior vitrectomy, then we suture the scleral effraction with vicryl 7/0 (Figure 2). Patient had a secondary implantation with crystalline lens with irien fixation, 15 days after the first surgery. The postoperative follow-up revealed a corrected visual acuity at 5/10, with no abnormalities on the rest of the examination, and the B-mode ocular ultrasound did not reveal any retinal detachment or intravitreal hemorrhage
Discussion
The incidence of phacocele is rare and is rarely reported in the literature, representing 13% of all cristaline dislocations, initially described by Fejir in 1928 [1]. The most commun mecanism of post traumatic Phacocele is a blunt injury to the eye, resulting from indirect trauma leading to scleral perforation [2], responsible to a dislocates of the lens through the scleral dehiscence into subconjuctival or subtenon space, this dehiscence is mostly in the quadrant supero-nasal followed by supero-temporal quadrant because of a projection of energy from temporal quadrant which is the most common site of impact, this rupture is mostly seen between limbus and spiral of Tillaux [3]. Clinical presentation include a painfull eye with a diminution of visual acuity, with a subconjonctival crystalline lens, an aphakia, vitreous in anterior chamber, sometimes an iridodialysis, and a normal or low ocular tonus [4]. Ultrasound B-scan is necessair to confirm the diagnosis, and to detect associated lesions like vitreous hemmoragea, retinal or choroidal detachement [5].
The management of post-traumatic phacocel consist in a chirugical extraction of the sub-conjonctival crystalline lens, and treatment of the other associated lesions in the order to restitue a visual acuity. We start with a conjunctival decouvrement, an extraction of the lens, an anterior vitrectomy, and a suture of the scleral defect [6], implantation should be realised secondary, to avoid error of IOL puissance, Cohen reported that primary IOL implantation results in a difference of refraction of 4 dioptres on using biometry of the non-traumatic eye [7]. In our case, the age was the risk factor of subconjonctival luxation of the crystalline lens because of the increased scleral rigidity and hard crystalline lens [8], the others risk factors include previous surgical or traumatic scleral scar, recurrent episodes of scleritis, a prolonged elevated intra-ocular pressure, and collagen disseas [9-3].
Conclusion
Traumatic phacocel is a rare type of lens post traumatic luxation, caused by blunt trauma in a fragilised sclera by age or general diseas. treatment is always surgical by extraction of crysatlline lens and implantation of artificiel lens and the prognosis depend of associeted oculare lesions.
References
- Fejér AJ. Subconjunctival lens dislocation. Am J Ophthalmol. 1928; 11: 254-6.
- Traumatic phacocele: a rare but unique scenario Manthan Hasmukhbhai Chaniyara, Anubha Rathi, Amar Pujari, Jayanand Sudhakar Urkude. 2017.
- Aniridia- Mandeep Tomar, Gaurav Sharma. A Case of Traumatic Phacocele in a Patient. Department of Ophthalmology, Hospital Sarkaghat, District Mandi, Himachal Pradesh, India. Delhi J Ophthalmol. 2019; 29: 117-119. http://dx.doi.org/10.7869/djo.464
- Neupane S, Das D & Korgaonkar S. Migrated subconjunctival crystalline lens: a traumatic phacocele. BMJ Case Reports. 2020; 13(7): e237014. [DOI:10.1136/bcr-2020-237014].
- Sindal MD, Mourya D. A rare case of traumatic posterior phacocele with retinal detachment. Indian J Ophthalmol. 2016; 64: 89.
- Hacocele Due To Blunt Trauma. Dr. SujataPriyambada Assistant Professor, Hi-Tech Medical College and Hospital, Rourkela. 2014.
- Cohen KL. Inaccuracy of intraocular lens power calculation after traumatic corneal laceration and cataract. J Cataract Refract Surg. 2001; 27: 1519-22.
- Traumatic phacocele: Review of eight cases, Kasturi Bhattacharjee, MS, FRCS, Harsha Bhattacharjee, Indian J Ophthalmol. 2007; 55(6): 466-468. [DOI: 10.4103/0301-4738.36487]
- Santos-Bueso E, Sáenz-Francés F, Díaz-Valle D, et al. [Ocular rupture associated with lens dislocation to the subconjunctival space]. Arch Soc Esp Oftalmol. 2007; 82: 641-4.

