Case Report - Volume 3 - Issue 1
Septic shoulder osteoarthritis post-covid-19 vaccination: A case report with literature review
Ibtissam EL OUALI*, Sara habib chorfa, kenza berrada, laila jroundi, FZ laamrani
Emergency Department, Ibn Sina University Hospital of Rabat, Morocco.
Received Date : Nov 17, 2022
Accepted Date : Dec 26, 2022
Published Date: Jan 16, 2023
Copyright:© Ibtissam El Ouali 2023
*Corresponding Author : Ibtissam El Ouali, Emergency Department, Ibn Sina University Hospital of Rabat, Morocco.
Email: ibtissam.elouali94@gmail.com
DOI: Doi.org/10.55920/2771-019X/1349
Abstract
This report emphasizes the relevance of MRI in non-resolving inflammation post-covid-19 vaccination in a 63-year-old female. In this patient, clinical examination was suggestive of septic arthritis confirmed by biology and MRI, which demonstrated cartilaginous damage and an extension of the infection to the bone. Therapeutical possibilities and prevention techniques are described and substantiated with a brief review of post-vaccinal arthritis cases in the literature. This report aims to delineate the utility of early MRI performance in persistent joint inflammation and the different possibilities available to the patient for optimal management at the early stages of the disease.
Keywords: Shoulder; Septic arthritis; vaccination; MRI.
Abbreviations: MRI: Magnetic Resonance Imaging; CT: Computed Tomography; IV: Intra-Veinous.
Introduction
Septic arthritis of the gleno-humeral joint is more common in the elderly and immune compromised [1], and post vaccination arthritis has been reported few times [2]. Our case draws attention to the importance of MRI, in case of an insidious onset of symptoms, or persistent pain or inflammation after an episode of vaccination. This imaging modality has been increasingly used to evaluate soft tissue, synovial reaction and marrow changes. It allows early detection of complication, especially osteomyelitis. A combination of T1-weighted, T2-weighted, short-tau inversion recovery, and post contrast T1-weighted fat-suppressed sequences are most helpful to set the diagnosis. The therapeutic decision consists of a combination of antibiotics, surgery and physical rehabilitation.
Clinical Presentation
A 63-year-old female patient with no history presented to the ER for sub acute inflammatory pain in the right shoulder, associated with fever and chills two weeks after receiving the covid-19 vaccination in the right arm. Clinical examination objectified signs of skin inflammation and a limited active and passive motion of the right shoulder, with spontaneous external drainage of pus. Biochemistry assessment revealed an increase in C-reactive protein (60 mg/l) and an elevated erythrocyte sedimentation rate (100 mm/h) with associated hyperleukocytosis (130x109/l). Plain radiograph showed glen humeral joint narrowing, erosion of the humeral head and soft tissue swelling (Figure 1). For a better assessment, a shoulder MRI 1,5 tesla was then performed and demonstrates cartilaginous damage and areas of osteolysis of the humerus on T1 weighted images with enlarged reactive axillary lymph nodes, marked bone edema and joint effusion as shown in T2w images (Figure 2). We note as well the presence of multiple fluid out pouchings enhancing peripherally after gadolinium administration resembling abscesses, and an associated synovitis and sub deltoid bursitis (Figure 3). These lesions present a discrete restriction on diffusion sequences. GRE sequence shows no sign of hemorrhage (Figure 4). This presentation is consisted with a shoulder osteoarthritis. The aspiration of the shoulder joint had brought purulent liquid consisting of altered neutrophils, direct examination was negative but microbiological culture confirmed the presence of staphylococcus aureus.
The patient then was immediately hospitalized. Treatment comprised intravenous antibiotics (Ampicillin) for two weeks, pain-relieving posture, analgesic and surgical drainage was done through tidal irrigation to remove the infectious discharge. Therapy switched to oral administration for two months with favorable evolution of clinical and biological inflammation but persistence of slight limitation of joint mobility. The patient was addressed then to physical rehabilitation.
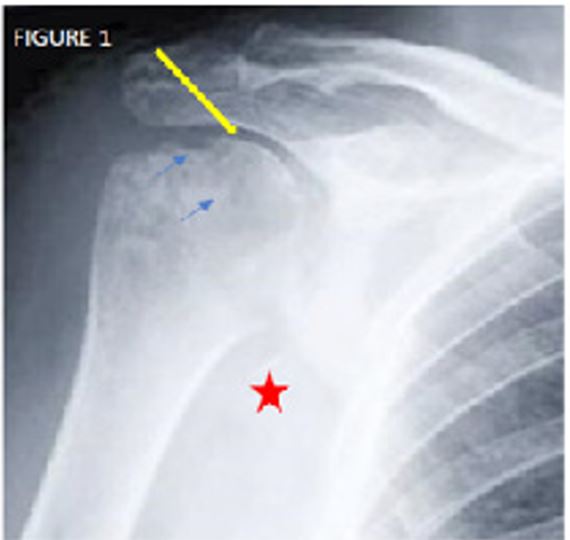
Figure 1: Anteroposterior x-ray of the right shoulder shows narrowing of the glenohumeral joint space (thick arrow), heterogenous humeral head with epiphyseal erosions (arrows) and soft tissue thickening (star).
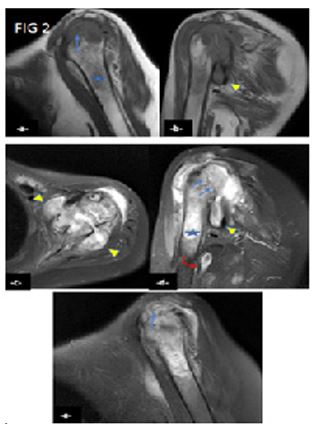
Figure 2: MRI of the left shoulder joint on T1W sagittal (a), coronal (b), T2W axial (c), coronal (d) and sagittal (e) images showing areas of osteolysis in the epiphyseal-metaphyseal regions, cartilaginous and subchondral erosions (arrows), subchondral and pericapsular edema signal demonstrating low T1 and high T2 signal (star), Synovial fluid outpouching with distension of axillary recess (arrows head) giving similar appearance to abscesses. We note also a marked gleno-humeral joint effusion, enlarged axillary lymph nodes (curved arrow) and soft tissues thickening.
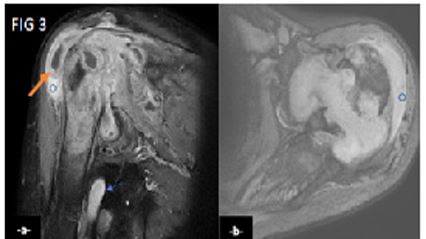
Figure 3: T1 weighted post contrast on coronal (a) and axial (b) images showing markedly thickened and enhancing synovium (thick arrow), small sub deltoid bursitis (circle), pericapsular and lymph nodes enhancement (arrow).
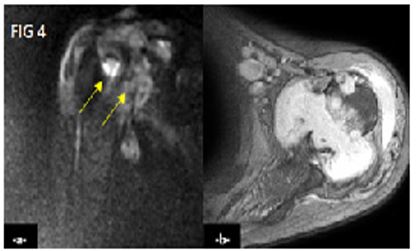
Figure 4: Diffusion weighted image (a) shows discrete restriction (arrows) andaxialT2* sequence (b) shows no signs of hemorrhage.
Discussion
Septic arthritis is an orthopedic condition involving the shoulder in 8 to 21% of cases [3]. It mostly affects immunocompromised patients with co-morbidities as demonstrated in literature [1]. However, several cases of septic shoulder have been described throughout history following a routine vaccination, and more recently, following the covid-19 vaccination [4-5], where only two reported cases were about septic joints [6-7], whereas the four other patients presented with either an inflammatory or an autoimmune reaction to the vaccine [3,5,8]. Severe complications can occur, such as osteomyelitis, adhesive capsulitis and osteonecrosis the mortality rate may reach 11.5% of patients with septic arthritis of the shoulder [9].
Anterior injection of the deltoid, especially in thinner patients, exposes to a high risk of inadvertent subacromial bursal and glenohumeral joint penetration. The synovium is a well-vascularized structure with no limiting basement plate, and this allows easy access by bacteria [10]. Once bacteria are inoculated in the joint space, the low fluid shear allows it to adhere to joint structures andproliferate [11], generating an acute cascade of inflammatory reaction and the pathogens are eliminated [12]. However, if the infection is not resolved due to a defected immune system, the high levels of cytokines produced by the immuno-regulatory cells may result in joint effusion that increases intra-articular pressure, which prevents blood and nutrients from reaching and supplying the joint, leading to synovium and cartilage destruction. Permeation of synovial stroma by a dense perivascular inflammatory infiltrate increases synovial thickness. The increased vascularity owing to vasodilation and angiogenesis, and increased permeability of inflamed blood vessels are responsible forsynovial enhancement due to synovial hyper vascularity and peri synovial edema seen in MRI.
Septic arthritis diagnosis consists of a series of physical and biological examination. However, when a deep joint is affected, shoulder joint in our case, the patient can be paucisymptomatic and clinical findings can be nonspecific making the diagnosis even more challenging. In that case, we resort to imaging.
Plain radiograph may be normal in the very early stage of the disease. Otherwise, it shows a narrowing of the joint space due to cartilage destruction in the acute phase, destruction of the subchondral bone on both sides of a joint. And, if left untreated, reactive juxta-articular sclerosis or even ankylosis.
Ultrasound shows joint effusion, a thickened and hyper vascularized synovium on Color Doppler. And sometimes, it can be used to guide aspiration. CT features are similar to those on radiographs with a better assessment of osseous lesions. MRI is sensitive and more specific for early changes as early as 24H after the onset of infection [13]. It helps as well rule out differential diagnosis and evaluating osseous, cartilaginous and soft tissue lesions. The major findings comprise joint effusion in 70% of cases, synovial thickening and synovial enhancement after IV administration of gadolinium, associated with peri synovial and soft tissue edema on T2W implying a high correlation with the clinical findings in patients with septic joint [14]. These findings can be present in all stages of septic shoulder.
Fluid out pouching is also seen and results from fluid dissection from the joint due to continuous pressure, presenting a similar appearance with abscess [15]. MRI demonstrated bone marrow reactive edema which is seen as hypointense in T1w and hyperintense in T2w images and help distinguish it from associated osteomyelitis, where edema is larger, confluent and more diffuse causing a blurring in bone marginson T1W images [16], which becomes clearer after contrast administration. This aspect is referred to as the “ghost sign” [17]. Diffuse marrow edema and cyst formation indicate and advanced stage of septic arthritis and predicts a bad prognosis even after arthroscopic debridement [18]. MRI has its limitation as some findings may lead to over diagnosis, such as synovial enhancement without joint effusion, which can be present in 23% of healthy joints [16]. The use of thin needles of 16mm is recommended in adults less than 60 kg receiving a vaccination in the deltoid and any abnormal sign within the first 24 hours, pain or shoulder joint dysfunction, should raise suspicions of septic arthritis [4]. Early initiation of intravenous therapy is highly recommended to control the infection. The choice of antibiotics depends on the most probable pathogen in each health institute. Recommended duration of intravenous (IV) therapy, varies from two to six or seven weeks [19-20]. However, literature gives evidence for short-course IV therapy efficiency (seven days) [21] and longer-term treatment for patients who failed to respond to the shorter regimen. Aspiration guided by ultrasound helps decompress and provide clinicians with culture sample to identify the pathogen(s).
Arthrotomy and arthroscopy are two procedures used for surgical debridement of osteochondral fragments and areas of osteomyelitis. They also provide specimens in case of non-conclusive joint fluid aspiration results. Moreover, arthrotomy showed better clinical and radiological improvement compared to aspiration [22]. Any delay in septic arthritis management can causean irreversible joint damage within 48 hours of the onset of infection and result in important sequela, especially osteonecrosisdue to increase in intra-articular pressure which compromises blood circulation.
Conclusion
A relatively high rate of reoperation, morbidity, and mortality has been associated with septic arthritis of the shoulder. Accurate diagnosis relies mainly on imaging findings, especially MRI that provides the surgeon with the best assessment of soft tissue, cartilage and bone, which allows a prompt and proper treatment, thereby, preventing complications like septic shock and osteomyelitis. Most importantly, a proper intramuscular injection technique is mandatory to avoid such severer infections.
Acknowledgement: I would like to express my gratitude to my professors and all the colleagues who participated in the completion of this work.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest: The authors declare no conflict of interest.
Author’s Contributions:
Ibtissam EL OUALI: Conception of the work, design of the work and acquisition of data.Drafting the work.
Chirihane AYADI: Acquisition of data.
Sara HABIB CHORFA: Acquisition of data.
Laila JROUNDI: Revising the work critically for important intellectual content.
F.Z LAAMRANI: Revising the work critically for important intellectual content and final approval of the version to be published.
References
- Menge TJ, Boykin RE, Byram IR, Bushnell BD. A comprehensive approach to glenohumeral arthritis. South Med J. 2014; 107(9): 567-573.
- Bodor M, Montalvo E. Vaccination-related shoulder dysfunction. Vaccine. 2007; 25(4): 585-587.
- Chokan Baimukhamedov, Shosaid Makhmudov, Aliya Botabekova. Seropositive rheumatoid arthritis after vaccination against SARS‐CoV‐2 infection, International Journal of Rheumatic Diseases. 2021; 24(11): 1440-1441.
- DeRogatis MJ, Parameswaran L, Lee P, Mayer TG, Issack PS. Septic Shoulder Joint After Pneumococcal Vaccination Requiring Surgical Debridement. HSS J. 2018; 14(3): 299-301.
- Unal Enginar A. Arthritis following COVID-19 vaccination: report of two cases. Int Immunopharmacol. 2021; 101:108256
- Massel DH, Haziza S, Rivera S, Mohile N, Subhawong TK, Hernandez VH. Septic Arthritis of the Shoulder After SARS-CoV-2 Pfizer Vaccination: A Case Report. JBJS Case Connect. 2021; 11(3). [DOI: 10.2106/JBJS.CC.21.00090].
- Wireko FW, Khalafalla S, Jamshidi T, et al. Septic and Crystal-Induced Arthritis (Pseudogout) Post-COVID-19 Vaccination. Cureus. 2022; 14(4): e23902.
- An QJ, Qin DA, Pei JX. Reactive arthritis after COVID-19 vaccination. Hum Vaccin Immunother. 2021; 17(9): 2954-2956.
- Assunção JH, Noffs GG, Malavolta EA, Gracitelli M. Lima A, et al. Septic arthritis of the shoulder and elbow: one decade of epidemiological analysis at a tertiary referral hospital. Revista brasileira de ortopedia. 2018; 53(6): 707-713.
- Goldenberg DL. Septic arthritis. Lancet . 1998; 351: 197-202.
- Shirtliff ME, Mader JT. Acute septic arthritis. Clinical Microbiology Reviews. 2002;15: 527-44.
- Koch B, Lemmermeier P, Gause A, Wilmowsky H, Heisel J, Pfreundschuh Ml. Demonstration of interleukin-1 beta and interleukin-6 in cells of synovial fluids by flow cytometry. European Journal of Medical Research. 1996; 1: 244-8.
- Tehranzadeh J, Wang F, Mesgarzadeh M. Magnetic resonance imaging of osteomyelitis. Crit Rev Diagn Imaging. 1992; 33: 495-534.
- Hopkins KL, King LCP, Bergman G. Gadolinium-DTPA-enhanced magnetic resonance imaging of musculoskeletal infectious processes. Skeletal Radiol. 1995; 24: 325-330.
- Ledermann HP, Morrison WB, Schweitzer ME. MR image analysis of pedal osteomyelitis: distribution, patterns of spread, and frequency of associated ulceration and septic arthritis. Radiology. 2002; 223: 747-755.
- Michael Karchevsky, Mark E. Schweitzer, William B. Morrison, and J. Antoni Parellada. MRI Findings of Septic Arthritis and Associated Osteomyelitis in Adults. American Journal of Roentgenology. 2004; 182(1): 119-122.
- Lim W, Barras CD, Zadow S. Radiologic Mimics of Osteomyelitis and Septic Arthritis: A Pictorial Essay. Radiol Res Pract. 2021; 9912257.
- Goetti P, Gallusser N, Antoniadis A, Wernly D, Vauclair F, Borens O. Advanced septic arthritis of the shoulder treated by a two-stage arthroplasty. World J Orthop. 2019; 10(10): 356-363.
- Peltola H, Vahvanen V. Acute purulent arthritis in children. Scand J Infect Dis. 1983; 15: 75-80.
- Lavy CB, Thyoka M. For how long should antibiotics be given in acute paediatric septic arthritis: a prospective audit of 96 cases. Trop Doct. 2007; 37: 195-7.
- Vinod MB, Matussek J, Curtis N, Graham HK, Carapetis JR. Duration of antibiotics in children with osteomyelitis and septic arthritis. J Paediatr Child Health. 2002; 38: 363-7.
- Smith SP, Thyoka M, Lavy CB, Pitani A. Septic arthritis of the shoulder in children in Malawi: a randomised, prospective study of aspiration versus arthrotomy and washout. J Bone Joint Surg [Br]. 2002; 84(B): 1167-72.

