Case Report - Volume 3 - Issue 1
A Case of IgG4-Related disease presenting with sclerosing mesenteritis
Dilnaz Alam; Priyanjali Pulipati*; Syed Ali Husain
Department of Internal Medicine, Trinity Health Oakland/ Wayne State University, 44405 Woodward Ave, Pontiac, Michigan, USA, 48341.
Received Date : Nov 23, 2022
Accepted Date : Dec 31, 2022
Published Date: Jan 21, 2023
Copyright:© Priyanjali Pulipati 2023
*Corresponding Author : Priyanjali Pulipati, Department of Internal Medicine, Trinity Health Oakland, Michigan, USA.
Email: Priyanjali.pulipati@trinity-health.org
DOI: Doi.org/10.55920/2771-019X/1354
Abstract
Background: Immunoglobulin G4 (IgG4) related disease is a relatively new disease characterized by inflammation, fibrosis, and eventually sclerosis. It has a tendency to form a mass in the affected organs and may be easily misdiagnosed as malignancy. Sclerosing mesenteritis (SM) is a rare presentation of IgG4-RD.
Case Report: We present a case of an 82-year-old female who presented with chronic, intermittent abdominal pain associated with nausea and vomiting. Computed tomography (CT) of the abdomen showed a mesenteric mass with regional lymphadenopathy concerning for malignancy. She underwent excision of the mass. Biopsy of the mass showed sclerosing mesenteritis with IgG4 infiltration with a final diagnosis of IgG4-RD sclerosing mesenteritis. She was discharged with an outpatient follow up with a rheumatologist and was eventually started on prednisone.
Conclusion: SM is rare presentation of IgG4-RD. Serum IgG4 levels are only elevated in two thirds of the patients. The gold standard for diagnosis is via histopathological examination of affected tissue. Early diagnosis and treatment can prevent fibrosis of the tissues.
Keywords: IgG4 related disease; sclerosing mesenteritis; cancer mimic.
Abbreviations: IgG4: Immunoglobulin G4; IgG4-RD: Immunoglobulin G4- related disease; SM: sclerosing mesenteritis; CT: computed tomography.
Introduction
IgG4-related disease (IgG4-RD) is a rare multi-system, autoimmune disease first described in 2003 [1]. It causes chronic inflammation, obliterative phlebitis and fibrosis in the pancreas, salivary glands, and intraperitoneal and retroperitoneal structures. It tends to form a mass in the affected organs and thus can mimic malignancies. IgG4-RD may or may not be associated with high serum IgG4 levels. Diagnosis is via biopsy and histopathological examination of the affected tissue. Sclerosing mesenteritis (SM) refers to a benign, idiopathic, primary inflammatory, and fibrotic process affecting the mesentery and is a rare presentation of IgG4-RD. Our case described below is of an 82-year-old female, who underwent a biopsy of suspected abdominal malignancy and was eventually diagnosed with IgG4-RD after histopathologic examination of tissue.
Case Presentation
An 82-years-old Caucasian woman with a significant medical history of diabetes mellitus type 2, essential hypertension, and ischemic cardiomyopathy reported intermittent, vague, right lower quadrant abdominal pain for the last 4 months. She had multiple urgent care and emergency room visits with similar complaints. She had an extensive workup including upper and lower gastrointestinal endoscopies, and an abdominal and pelvis computed tomography scan about 2 months ago which did not reveal any underlying cause of her abdominal pain. She was treated empirically with pantoprazole, polyethylene glycol, and dicycloverine for her symptoms. She also had a history of maxillary sinus mass which was resected about 20 years ago. However, she was unsure about the biopsy result, and there was no previous record.
On her current presentation, she came with severe, right lower quadrant abdominal pain, 10/10 in intensity, sharp in character, and associated with nausea and non- bloody vomiting. Initial blood work-up was unremarkable except for a high sedimentation rate of 109 and C-reactive protein of 2.24. Abdominal x-ray showed a partial small bowel obstruction. CT of the abdomen and pelvis showed 2-3 mesenteric masses with large mesenteric lymph nodes, concerning for possible malignancy. The most likely differentials were carcinoid tumor, lymphoma, or secondary metastatic tumors based on radiological findings. This prompted a general surgery consultation. She underwent a diagnostic laparoscopy and an exploratory laparotomy which revealed bulky mesenteric masses with dense reaction and involution of small bowel loops. About 120 cm of the small bowel and large mesenteric nodes were resected and sent for biopsy. Her postoperative course was uneventful and she reported complete resolution of her abdominal symptoms. The biopsy report was suggestive of sclerosing mesenteritis with storiform fibrosis and IgG4 infiltration suggesting a diagnosis of IG4-related sclerosing mesenteritis. The patient was discharged from the hospital 9 days after the surgery and was referred to a rheumatologist outpatient. Further workup at the rheumatologist’s office showed normal IgG4 levels. She was offered prednisone, however, she refused to take any treatment.
On post-op day 25, she presented to the emergency room again for similar lower quadrant abdominal pain. Repeat CT abdomen and pelvis showed no evidence of bowel obstruction, residual nodular calcification within the root of the mesentery, and new calcified soft tissues nodular lesion in the mesentery of right lower quadrant. After a discussion with her rheumatologist, she agreed to start prednisone 20 mg. At her one-month follow-up, she reported improvement and no clinical signs of flare-ups.
Discussion
The IgG4-related disease is a rare autoimmune disease characterized by chronic inflammation and sclerosis. It was first identified after autoimmune pancreatitis, which is associated with elevated IgG4 levels, was observed to be associated with extrapancreatic manifestations [1]. Previously recognized conditions like Mickuliz’s syndrome and Riedel’s thyroiditis are now thought to be a part of the IgG4-RD spectrum [2]. IgG4 production is controlled primarily by type 2 helper cells (Th2) [3]. The exact etiology and pathological mechanism are unknown. It is hypothesized that the IgG4 immunoglobulin may itself cause damage to the seeding tissue or that it may be elevated due to an unidentified antigen. Interestingly, a study showed that most patients with autoimmune pancreatitis have antibodies for Helicobacter pylori due to molecular mimicry [4]. This gave rise to a hypothesis that antibodies against bacterial antigens might result in autoimmunity due to molecular mimicry. Antibodies to self-antigens such as galectin-3, annexin- A11, laminin-511, and prohibitin have also been identified in IgG4-RD [5].
Although the epidemiology has not been clearly established, Asian men between 50-and 70 years of age might be more susceptible [6]. In Japan, the annual incidence was estimated to be 0.28-1.28 per 100,000 [7]. It is unclear if a similar epidemiology applies to all populations. Although there are no guidelines available for the diagnosis of IgG4-RD a Japanese consensus group in 2011 established criteria for diagnosis. A 2020 revised comprehensive diagnostic (RCD) criteria is shown in (Table 1) [8]. Only 50-67% of IgG4-RD patients have high serum IgG-4 levels [9]. It is also questionable if IgG4 levels may be used as an indicator of disease severity when elevated. The mainstay of treatment for IgG4-RD is steroids. The Japanese consensus recommends prednisone at a dose of 0.6mg/kg/day for 2-4 weeks. Azathioprine, mycophenolate, and methotrexate may also be used as steroid-sparing agents. For patients with refractory disease, rituximab can be the drug of choice. It is important to start treatment early before fibrosis sets in.
IgG4-RD is known to tend to form masses in its affected organs but cases of sclerosing mesenteritis in IgG4-RD are rare. Though SM is benign, the disease is a debilitating condition due to the high risk of recurrence and local mass effects. Only around 43 cases of IgG4-RD associated SM were identified in a literature search as of April 2022. Like in our case, most patients presented with abdominal pain. The diagnosis is challenging as SM usually mimics a tumor mass on imaging. The final diagnosis of the mass mainly relies on histopathological findings of the surgical or endoscopic biopsy specimen. Most patients in the cases of IgG4-RD and SM responded drastically to surgical excision and steroids.
Table 1: 2020 revised comprehensive diagnostic (RCD) criteria.
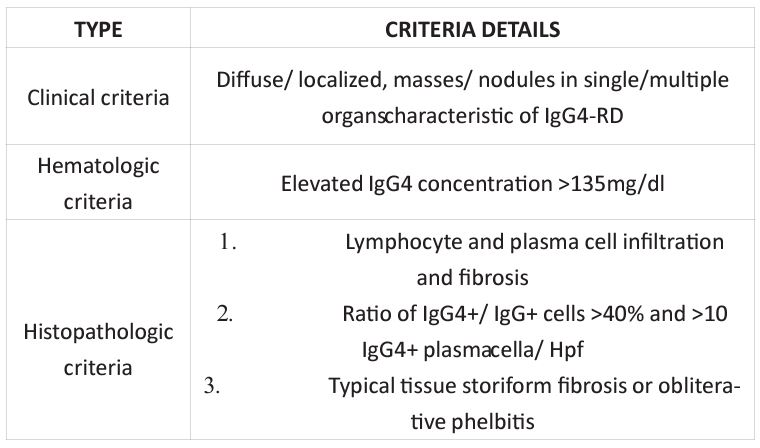
Diagnosis:
Definite: Clinical + Hematologic + Histopathologic criteria Probable: Clinical + Histopathologic criteria
Possible: Clinical + Hematologic
Conclusion
Sclerosing mesenteritis is a rare presentation of IgG4-RD. It may present as a mass which may lead to a misdiagnosis of malignancy. The gold standard for diagnosis is via tissue specimen and histopathological diagnosis. Treatment may involve surgical excision and treatment with steroid or steroid-sparing agents. If refractory, can be treated with rituximab. Early diagnosis and treatment are important to avoid fibrosis.
Declaration of interest: None.
Funding: None.
Acknowledgments: None.
References
- Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38: 982-4.
- Pieringer H, Parzer I, Wöhrer A, et al. IgG4- related disease: an orphan disease with many faces. Orphanet J Rare Dis. 2014; 9: 110.
- Aalverse RC, Stapel SO, Schuurman J, et al. Clin Exp Allergy. 2009; 39: 469-477.
- Culver EL, Smit W, Evans C, et al. Helicobacter Pylori as a Microbial Antigen in IGG4-Related Disease. Journal of Hepatology. 2016; 64: S644.
- Lanzillotta M, Mancuso G, Della-Torre E. Advances in the diagnosis and management of IgG4 related disease. BMJ. 2020; 369: m1067.
- Lang D, Zwerina J, Pieringer H. IgG4-related disease: current challenges and future prospects. Ther Clin Risk Manag. 2016; 12: 189-99.
- Uchida K, Masamune A, Shimosegawa T, et al. Prevalence of IgG4-related disease in Japan based on Nationwide Survey in 2009. Int J Rheumatol. 2012; 2012: 358371.
- Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012; 22: 21-30.
- Wallace Z, Stone J, Deshpande V, et al. Igg4-related disease: baseline clinical and laboratory features in 125 patients. Ann Rheum Dis. 2015; 74: 851-1851.

