Case Report - Volume 3 - Issue 1
Hepatic perfusion disorder secondary to superior vena cava compression: A case report
Banao M1*; Zakariaa I2; Mahdar I3; Laoudiyi D4; Chbani K5; Salam S6
1Medical Doctor, Resident In Tird Year Of Radiology BP, Morocco.
2Medical Doctor, Residentin Fourth Year Of Radiology, Morocco.
3Medical Doctor, Resident In Second Year Of Radiology, Morocco.
4Medical Doctor, Associate Professor. Morocco.
5Medical Doctor, Professor Of Highereducation, Morocco. 6Medical Doctor, Professor Of Highereducation. Chief Of Pediatric Department Of Radiology, Morocco.
Received Date : Dec 14, 2022
Accepted Date : Jan 09, 2023
Published Date: Jan 30, 2023
Copyright:©Banao M 2023
*Corresponding Author : Banao M, Pediatric radiology departement, university ospital center of casablanca, Morocco.
Email: mayabano@gmail.com
DOI: Doi.org/10.55920/2771-019X/1361
Abstract
The aim of this work is to describe the hepatic perfusion abnormalities related to the portacaval shunt during the superior vena cava syndrome through an illustrative clinical case. We will then describe the different anastomoses that lead to these perfusion disorders as well as the other anastomoses involved in the vena cava syndrome.
Keywords: Vena cava; superior vena cava syndrome; hepatic perfusion; portosystemic shunts.
Abbreviations: SVC: Superiorvena Cava; CVC: Collateralvenous Circulation ; TABC: Brachiocephalicvenoustrunk; PDC: Contrast.
Introduction
Obstruction of the superior vena cava is most often secondary to a malignant disease lymphoma, bronchopulmonary cancer, secondary mediastinal adenopathies) which leads to compression or invasion of the superior vena cava; or to thrombosis on a central catheter. To overcome this obstacle, several networks of venous collaterals and anastomoses are engaged to ensure venous return to the right atrium. One of these collaterals, the portacaval anastomosis, is responsible for a characteristic hepatic perfusion disorder that we will illustrate with the case of a child who presents a mediastinal mass compressing the SVC. We will then discuss the other shunts that can be used to ensure venous return to the right atrium.
Case report
We report the case of 13 year-old, with no prior medical history, presenting signs of Superior Vena Cava Syndrome for over 3 weeks (dyspnea, cough, facial puffiness and palpebral edema), with evidence on clinical examination of turgidity of the jugular veins with thoracic collateral venous circulation. The chest X-ray showed enlargement of the upper mediastinum. Thoracic CT showed an 89x85x80 mm anterior mediastinal tissue process, compressing the SVC and the innominate vein responsible for dilatation of the azygos system, internal mammary veins with peri-vertebral CVC. This process also involves the ascending aorta and exerts a mass effect on the pulmonary artery trunk and right atrium. During the thoracic-CT scan,the upper abdominal imagesdemonstrated intense contrast enhancement of IV hepatic segment. Abdominal ultrasound was immediately performed to look for the abnormality of the IV hepatic segment, the ultrasound showed no abnormality.
The liver was then explored on CT, with acquisitions before and after contrast injection at arterial, portal and delayed phases. This allowed to demonstrate an intense and early triangular subcapsular contrast enhancement of the II and IV segments at the arterial phasewhich disappeared at the portal and delayed phases. Biopsy results of the mediastinal mass concluded to a lymphoma.

Figure 1: Thoracic CT scan performed after injection of iodinated PDC (mediastinal window). Anterior mediastinal mass compressing the superior vena cava with absence of opacification of the brachiocephalic veins.
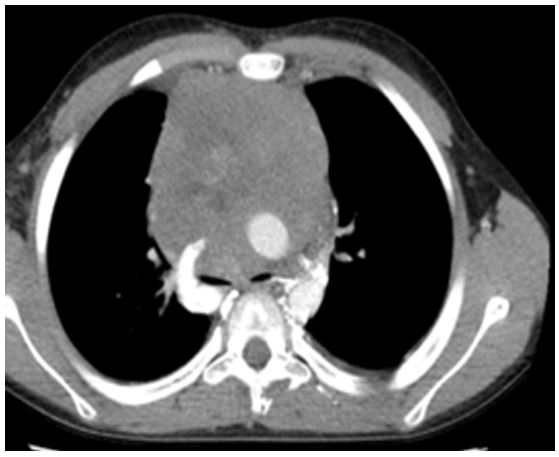
Figure 2: Thoracic CT scan aftercontrast administration (mediastinal Windows) demonstratingenlargement of the azygos system withperivertebralcollateral circulation.
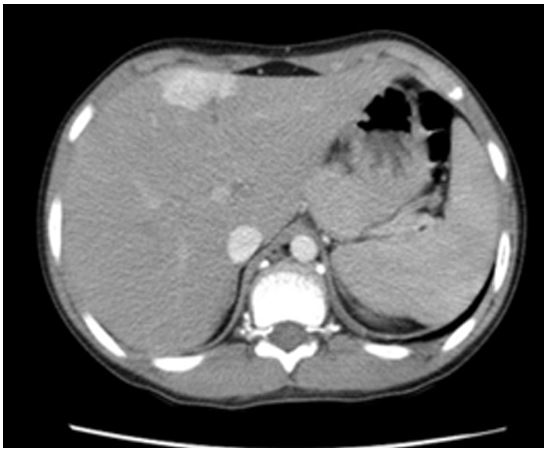
Figure 3: Abdominal CT scan performed after injection of contrast at arterial phase (30 seconds). Contrast enhancement of the II and IV segments
Discussion
The hepatic contrast enhancement found in the case of our patient is called the "hot spot sign", it is explained by the presence of portacaval shunting pathways through the trans-diaphragmatic pathway. The blood flow follows communications developed between branches of the right internal thoracic vein and the inferior diaphragmatic branches, it then follows trans-diaphragmatic routes and, after a hepatic trans-capsular passage, reaches the portal venous network, the hepatic veins and the inferior vena cava. The fluid that irrigates the circuit: branches of the internal thoracic vein-transdiaphragmatic and then transcapsular branches and then intrahepatic portal branches is in fact contrast product that is little or not diluted by blood, and is diverted directly after its injection.
Several other bypass routes are also developed in the superior vena cava syndrome, in order to bring blood back to the right heart:
- Cavocavalanastomosis: between portions of the superior vena cava or between the superior and inferior vena cava. These anastomoses borrow several systems: azygos venous system and spinal venous plexuses (intra- and peri- spinal), internal thoracic veins - epigastric veins tributary to external iliac veins, external thoracic veins - superficial abdominal subcutaneous veins tributary to internal saphenous veins, mediastinal veins, peri-esophageal veins.
- Anastomoses between the superior vena cava system and the pulmonary venous system. They are made through the pulmonary vein-bronchial vein-azygos system.
- Portacaval anastomoses: They are rare in superior vena cave syndrome, perform bypass routes between the superior cave system and the inferior vena cava via the portal system and then a transhepatic route. They are always associated with cavocaval anastomoses. These portacaval anastomoses are: the peri-esophageal routes, the cava-anterior thoracic veins-phrenic veins-hepatic capsule-gate system route (trans-diaphragmatic routes), the cava-anterior thoracoabdominal parietal veins-para-umbilical vein route (para-umbilical routes).
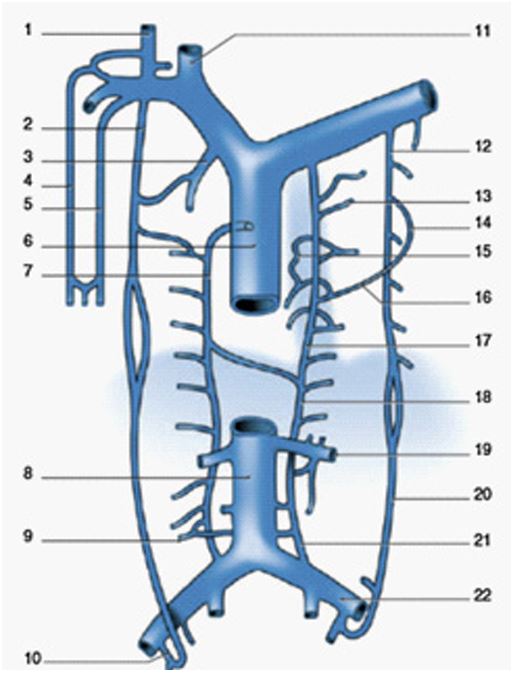
Figure 4: System of anastomosis between superior and inferior vena cava: 1.External jugular vein; 2.Right internal thoracic vein; 3.Right internal mammary vein; 4.Cephalic vein; 5.Basilic vein; 6.Superior vena cava; 7.Greater azygos vein; 8.Inferior vena cava; 9.Lymphatic vein; 10.Right internal saphenous vein junction; 11. Right internal jugular vein; 12.Left internal thoracic vein; 13.Posterior intercostal vein; 14.Anteriorintercostal vein; 15.Esophageal vein; 16.Posterior intercostal vein; 17.Accessory hemiazygos vein; 18.Hemiazygos vein; 19.Left renal vein; 20.Epigastric vein; 21.Ascending lumbar vein; 22.left common iliac vein.
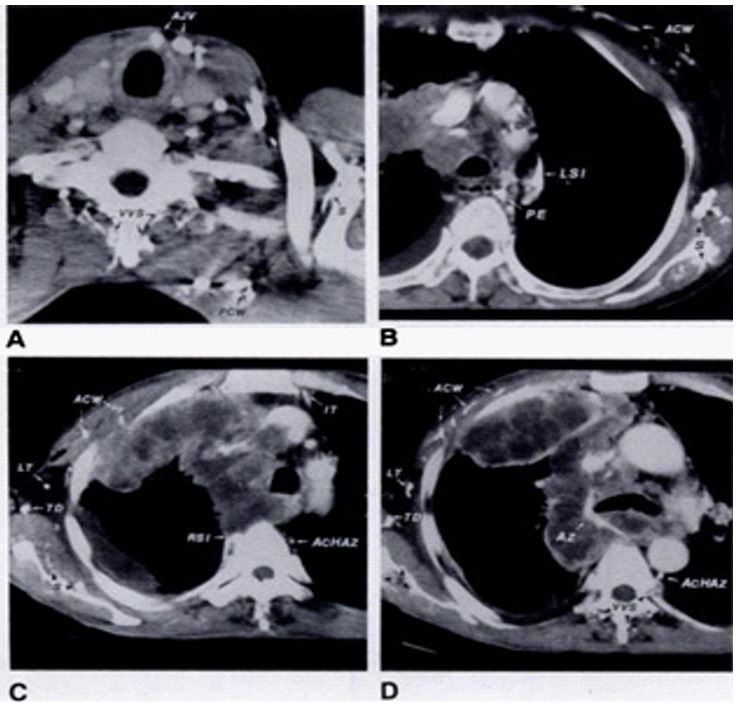
Figure 5: -A--D, Transverse CT scans from two patients with lung cancer (.4 and B) and a patient with malIgnant mesothelioma (C and 0) show various collateral pathways. AcHAz = ac- cessory hemlazygos vein, ACW = veins in ante- nor chest wall, MV = anterior jugular vein, Az = azygos vein, IT = internal thoracic vein, LSI = left superior intercostal vein, LT = lateral theracic vein, PCW = veins in posterior chest wall, PE = periesophageal vein, RSI = right superior intercostal vein, S = veins around scapula, TD = thoracodorsal vein, WS = vertebral venous system.
Conclusion
Hepatic portacaval shunt contrast in superior vena cava syndrome is a rare phenomenon. The visualization of this characteristic hepatic contrast enhacncement associated with dilatation of the azygos system, peri- and intra-vertebral veins, and thoracic or abdominal collateral circulations should lead to a search for thrombosis or obstruction of the superior vena cava.
References
- Charrada-Ben, Farhat L et al. Hepatic perfusion disorders secondary to superior vena cava thrombosis: about 3 cases.
- Baba Y et al. Altered flow dynamics of intravascular contrast material to the liver in superior vena cava syndrome: CT findings.
- Dahan H et al. Cavoportal collateral pathways in vena cava obstruction : imagingfeatures AJR. 1998; 171: 1405-1411.
- Grayet D et al. Systemic-to-pulmonary venous shunt in superior vena cava obstruction revealed on dynamic helical CT AJR. 2011; 176: 211-213.
- Jallaguier A et al. Varices oesophagiennes secondaires à une thrombose cave supérieure J Radiol 2008 ; 89 :1761-1763.
- M Arsicot et al. Endovascular curative treatment of superior vena cava syndrome, case study of the Touraine experience.journal des maladies vascular. 2012; 37: 118-123.
- Kim et al. AJA. 1993: 161.

