Case Report - Volume 3 - Issue 1
Perioperative anaesthetic management in post Fontan adult patient with kyphoscoliosis for transsphenoidal resection of pituitary tumour
Jyoti Kanwat1*; Bhanupreet Kaur2; Gopal Krishan Jalwal3; Inderpreet Singh4; Deepa Yadav5
1Assistant Professor, Department Of Anaesthesia, Aiims Bathinda, Punjab, India.
2Senior Resident, Department Of Anaesthesia, Aiims Bathinda, Punjab, India.
3Assistant Professor, Department Of Anaesthesia, Aiims Bathinda, Punjab, India.
4Junior Resident, Department Of Anaesthesia, Guru Gobind Singh Medical College And Hospital, Faridkot, Punjab, India.
5Senior Resident, Department Of Anaesthesia, Rajasthan University Of Health Sciences, Jaipur, Rajasthan, India.
Received Date : Dec 21, 2022
Accepted Date : Jan 14, 2023
Published Date: Feb 05, 2023
Copyright:© Jyoti Kanwat 2023
*Corresponding Author : Jyoti Kanwat, Assistant Professor, Department of Anaesthesia, Aiims Bathinda, Punjab, India.
Email: gopikanwat@gmail.com
DOI: Doi.org/10.55920/2771-019X/1366
Abstract
Pituitary macroadenomas are most common suprasellar tumours in adult. Trans sphenoidal approach is commonly used for tumour resection. We report a case of forty four year old female who had undergone fontan palliation procedure at age of 19 years with pulmonary stenosis, thoracic khyphoscoliosis and pulmonary artery hypertension at present who presented for excision of tumor. Along with general concerns of pituitary patient was nebulised with bronchodilators, milrinone, encouraged spirometry, lung protection strategies were used for ventilation and hemodynamic stability maintained. Multi system involvement poses challenge to anaesthetists as it demands management and care of all the involved systems.
Keywords: Perioperative; anaesthestic; pituitary macroadenoma; kyphoscoliosis; fontan.
Introduction
Pituitary macroadenomas are the most common suprasellar tumours in adults. Pituitary tumours in particular make a multidisciplinary team approach necessary for good perioperative and postoperative management of the patient. It further imposes challenges when a patient has multisystem involvement. We are reporting successful anaesthetic management of a middle-aged woman posted for transsphenoidal pituitary tumour resection with status post Fontan palliation and now having severe pulmonary stenosis with moderate kyphoscoliosis and pulmonary arterial hypertension.
Case Report
A 44-year female, presented with chief complaints of blurring of vision (bitemporal site) and supraorbital pain for one month. She was diagnosed with pituitary macroadenoma and posted for transnasal trans-sphenoidal removal of the tumour. Previously, this patient underwent an extracardiac fontan procedure for Double Inlet Left Ventricle at the age of 19 years. Since then the patient was on the tablet acenocoumarol 2 mg regularly and with no signs and symptoms of cyanotic heart disease at present. Dyspnea (NYHA class II) was present and her metabolic equivalent of the task score (METS) was 4 with moderate perioperative cardiac risk.
General physical examination was unremarkable. Cadiovascular system examination showed a surgical scar. On auscultation, grade 2 murmur in the pulmonary area was present. Electrocardiogram (ECG) showed right ventricular hypertrophy with right axis deviation and non-specific ST-T changes. Echocardiography (ECHO) showed post-op extracardiac Fontan status for single ventricle physiology-Double inlet left ventricle with- severe pulmonary stenosis (SV-DILV-PS) with normal left ventricular function at present but raised pulmonary artery pressure. Moderate degree of thoracic kyphoscoliosis (Cobb’s angle 28 degree) was present. Chest x-ray showed cardiomegaly, sternal wiring, thoracolumbar kyphoscoliosis with mediastinal shift to the right (Figure 1). Preoperative pulmonary function tests revealed moderate restrictive pattern. Complete blood count, liver, kidney function test, urine routine, blood sugar, serum cortisol and thyroid function tests were normal. Prothrombin Time (PT)/International normalised ratio (INR) was 2.57. The patient was advised to repeat INR daily and switch to low molecular weight heparin from warfarin when INR<= 1.5. Magnetic Resonace imaging (MRI) scan has been done for pituitary macroadenoma localisation (Figure 2A,B).
Patient was adviced nill per oral 8 hours prior to surgery. Incentive spirometry encouaraged. Nebulisation with ipratropium, budesonide and milrinone at 1mg/ml (to reduce pulmonary artery pressure) was done. The morning dose of low molecular heparin was omitted and INR repeated on the day of surgery. The patient was counselled about postoperative nasal packing and mouth breathing.
Patient was brought to the operation theatre. Antibiotic prophylaxis was given to prevent infective endocarditis and systemic infection. Standard ASA monitors were attached. Right radial artery cannulated for intra-arterial blood pressure monitoring. In addition Bispectral Index (BIS), urine, temperature and CVP monitoring were used. Premedication was done with injection glycopyrrolate 0.2 mg, midazolam 1 mg, palonosetron 0.075 mg. Patient was induced with injection. fentanyl 150 mcg, etomidate 25 mg, cisatracurium 12 mg and intubated with endotracheal tube size 7.5 mm. The oropharynx was packed with saline-soaked gauze. After intubation, lumbar drain was inserted in the lateral position. Anaesthesia was maintained with oxygen and air (50:50) mixture along with desflurane to maintain BIS between 40 and 60. Infusion of propofol (25-75mcg/kg/min), cisatracurium (2 mcg/kg/min), fentanyl(0.5-1mcg/kg/min) and hydrocortisone (50mg eight hourly) was maintained throughout the surgery. CVP was maintained between 12-16cm of water by intraoperative fluid therapy and urine output was also adequate. Injection paracetamol (1 gram) and continuous fentanyl infusion used for analgesia. Arterial blood gas done towards end of surgery and were within normal limits. At the end of the surgery, the patient has reversed with glycopyrrolate 0.4 mg and neostigmine 2.5 mg and extubated smoothly ( esmolol bolus 90 sec before extubation) when fully awake. Post operativelythe patient was shifted to the neuro ICU. Repeat ECHO and cardiac evaluation was done. Early ambulation and resumption of anticoagulation therapy was advised. Post operative course remained uneventful and patient was discharged successfully on the post-op day seven.
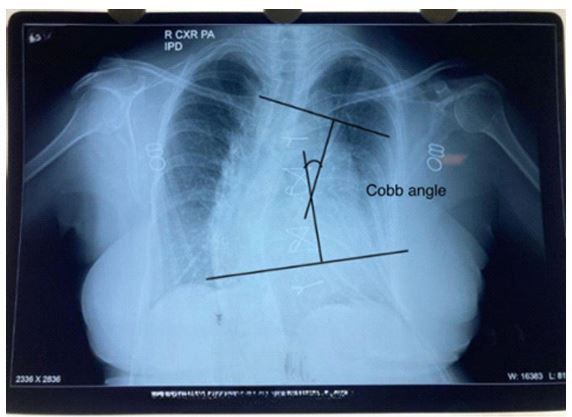
Figure 1: Chest x ray showing sternal wiring and thoracic khyphoscoliosis.
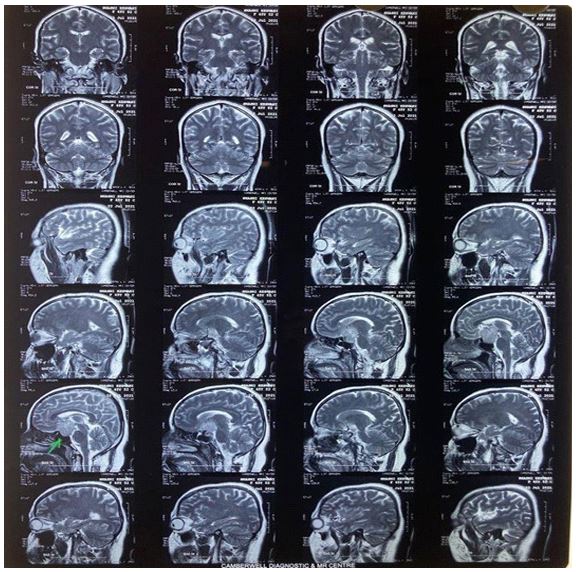
Figure 2A: Mri images (saggital section) showing pituitary macroadenoma.
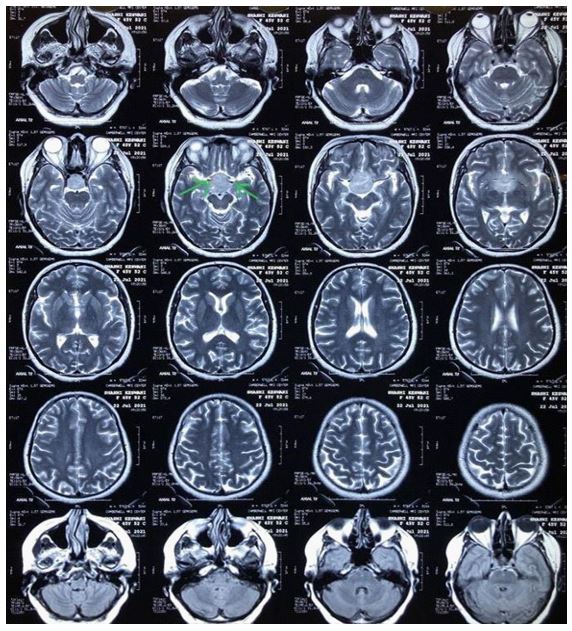
Figure 2b: Mri image showing tumour encasing bilateral internal carotid arteries
Discussion
Pituitary adenoma represents 10% to 25% of all intracranial neoplasms and its prevalence is 16.7% in the general population [1]. The transsphenoidal approach is the most commonly used because it has minimal surgical trauma and blood loss but sitting posture has increased risk of air embolism. The aim of the anaesthetic technique regarding pituitary tumours remains perioperative hemodynamic stability, maintenance of normal intracranial pressure, provision of smooth surgical conditions like ‘lax brain’, maintenance of adequate cerebral blood and oxygen supply, metabolic homeostasis, rapid emergence and smooth recovery from anaesthesia on completion of surgery [2]. Invasive blood pressure monitoring, glucocorticoid replacement, anticonvulsant prophylaxis along with glycemic control were also important intraoperatively. During the valsalva maneuver for CSF leaks, depth of anaesthesia kept high and monitored by BIS [3]. Nasal obstruction due to nasal packing is explained to the patient prior [4]. Fast recovery from anaesthesia is vital because early neurological assessment is required as it can disclose serious surgical complications hence we used fentanyl, a short-acting opioid. For the smooth emergence from anaesthesia and hemodynamic stability, we used esmolol injection. Dyson et al have documented the use of esmolol before extubation to prevent haemodynamic response [5]. Long term follow up of the patients with endocrinologists to assess their hormonal status is mandatory. In post-op, patient monitoring and management are done by a multidisciplinary team in ICU.
Our patient had a moderate degree of kyphoscoliosis. Long-standing kyphoscoliosis causes restrictive lung disease and raised pulmonary artery (PA) pressure [6]. We used milrinone (selective pulmonary vasodilator) nebulisation to control PA pressure preoperatively. It has been used over the past many years for this purpose [7]. Incentive spirometry, deep breathing exercise, nebulisation with milrinone, lung -protective ventilatory strategies were used for optimisation of respiratory status.
Fontan procedure was first described by Fontan and Baudet in 1971 [8]. Fontan repair is usually done at the age of 18 months to 4 years but our patient underwent Fontan repair at the age of 19 years because of the unavailability of a surgical facility in India. Now a days it is common to see the post-Fontan status patient for elective and emergency procedures due to improved surgical and anaesthetic techniques. Fontan patients are particularly at risk of recurrent hypoxia, arrhythmia, ventricular dysfunction and venous air embolism during the peri and post-operative period [9]. We aimed to maintain cardiac output, pulmonary vascular resistance, avoidance of air embolism, avoidance of any factors that depress myocardium and increase pulmonary vascular resistance like hypoxia, hypothermia, acidosis, pain, increase in intrathoracic pressure or excessive peep [10]. For induction etomidate was used because of its cardio-stable properties as it preserves myocardial contractility, PVR, and vascular tone [11]. A high concentration of inhalational anaesthetics is avoided because it causes myocardial depression so we used a low concentration of inhalational agent along with opioid infusion to maintain a cardio-stable environment. Proper post-operative monitoring and follow up with cardiologists and resumes of anticoagulants are important in the post-op period.
Conclusion
A thorough understanding of post-Fontan physiology, kyphoscoliosis, cardio-respiratory optimisation and management of its associated complications are important for successful patient outcomes. The advancement of surgical techniques, anaesthetic and medical management has improved the survival of patients with multiple system involvement
References
- Melmed S. Pathogenesis of pituitary tumors. Nat. Rev. Endocrinol. 2011; 7(5): 257-266.
- Horvat A, Kolak J, Gopčević A, Ilej M, Gnjidić Z. Anesthetic management of patients undergoing pituitary surgery. Acta Clin Croat. 2011; 50: 209-16.
- Jane JA Jr, Thapar K, Kaptain GJ, Maartens N, Laws ER Jr. Pituitary surgery: Transsphenoidal approach. Neurosurgery. 2002; 51: 435-42.
- Nemergut EC, Dumont AS, Barry UT, Laws Er. Perioperative management of patients undergoing transsphenoidal pituitary surgery. Anesth Analg. 2005; 101(4): 1170-81.
- Dyson A, Isaac PA, Pennant JH, Giesecke AH, Lipton JM. Esmolol attenuates cardiovascular responses to extubation. Anesth Analg. 1990; 71: 675-8.
- Huang SW, Wu CL, Lin CC, Hung CL, Kuo LK, Weng YL, et al. Effect of long term intermittent nocturnal non-invasive positive pressure ventilation on patient with severe kyphoscoliosis and hypoxaemia. BMJ Case Rep. 2009; 2009: bcr08.2008.0737. [PMID: 21686653; PMCID: PMC3029826 DOI: 10.1136/bcr.08.2008.0737].
- Buckley MS, Feldman JP. Nebulized milrinone use in a pulmonary hypertensive crisis. Pharmacotherapy. 2007; 27: 1763-6.
- Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax. 1971; 26(3): 240-8.
- Piran S, Veldtman G, Siu S, Webb GD, Liu PP. Heart failure and ventricular dysfunction in patients with single ventricle or systemic right ventricles. Circulation. 2002; 105: 1189-94.
- McClain CD, McGowan FX, Kovatsis PG. Laparoscopic surgery in a patient with fontan physiology. Anesth Analg. 2006; 103: 856-8.
- Sprung J, Ogletree-Hughes ML, Moravec CS. The effects of etomidate on the contractility of failing and nonfailing human heart muscle. Anesth Analg. 2000; 91(1): 68-75.

