Research Article - Volume 3 - Issue 1
The management in dentistry of patients with hereditary angioedema due to c1-inhibitor deficiency
M Elbouhairi; K Kamlich; M Sidqui*
Faculty of dental medicine, Hassan ii university, casablanca, Morocco.
Received Date : Dec 13, 2022
Accepted Date : Feb 05, 2023
Published Date: Feb 14, 2023
Copyright:© M Sidqui 2023
*Corresponding Author : M Sidqui, Faculty of dental medicine of Casablanca, Abu al alaa zahar street 21100 b.p: 9157, Sultan sultan Casablanca, Morocco.
Email: m.sidqui@yahoo.fr
DOI: Doi.org/10.55920/2771-019X/1374
Abstract
Dental care is an important source of risk factors for patients with angioedema. In addition to the physical stress caused by dental care or surgery, psychological and emotional stress can be generated by dental care, as well as possible dental infections, a factor that aggravates trauma and stress (linked to pain).
A multidisciplinary management (dental surgeon, physician, hospital service in some cases) allows patients suffering from angioedema to be treated while limiting the risks of occurrence of edema. Depending on the patient's illness, history and the procedure to be performed, he or she may receive prophylactic treatment and, if necessary, inpatient or outpatient care. The type of management (office or hospital if necessary) will depend on the type of procedure planned (treatment or surgery), the patient's personal experience, the intensity of his attacks and his response to treatment. The patient must discuss this with his dental surgeon, a true relationship of listening and trust is then essential. The dental surgeon should not generalize and should keep in mind that hereditary angioedema is a chronic disease whose clinical evolution is capricious and difficult to predict. Although it is possible to reduce the risk of edema following dental care, it is impossible to eliminate this risk.
Today, dentistry involves us in a global medical vision of the patient. A precise interrogation and anamnesis are no longer enough. The dental surgeon must, by listening to the patient and by good communication with other health practitioners, define the patient's complete state of well-being: physical, psychological and moral. In the case of this pathology, the dental surgeon may be alerted by certain clinical signs and inform the physician who is likely to make a correct diagnosis. In such a context, the dental surgeon must be familiar with this rare but potentially life-threatening condition. He must, on the one hand, be able to propose an adapted management to each patient and, on the other hand, be able to detect the first signs of the occurrence of a crisis and take the adequate measures.
Introduction
Bradyk in angioedema (BAE), of which hereditary C1-inhibitor angioedema is a part, is a rare and potentially serious disease. It is a recurrent subcutaneous or submucosal edema caused by a quantitative and/or qualitative deficiency of the C1 inhibitor of complement (C1-INH). There are hereditary forms (HAE) and acquired forms (AOA).
From one individual to another, the attacks can be very different, but in the same individual, they often recur at the same place. The attacks are often preceded by prodromes, however the risk of mortality related to this disease is high in the absence of immediate treatment, particularly in the case of edema of the upper respiratory tract (laryngeal edema). Oral care is one of the triggers because of its traumatic and psychological nature. Edema can occur following surgical and conservative dental care including simple scaling.
Currently, hospital management of dental care is recommended, but according to a recent study, patients are mainly followed up in private dental practice. The hospital setting is often considered by patients to be a place for emergencies and can therefore be an additional stressor.
Nowadays, treatment in private practice is possible thanks to the availability of new molecules and to the evolution of the therapeutic scheme. However, this management is multidisciplinary and the implementation of a prophylaxis is necessary. It is important that this disease is known by dentists to allow them to propose all the therapies, in accordance with the acquired data of science, thanks to an adapted management of the patients carrying bradykinic angioedemas.
The aim of our work is to review this disease and its treatments, to inform dentists and to allow an adapted management of patients suffering from hereditary angioedema by C1 inhibitor deficiency for any oral act.
Hereditary angioedema (HAO)
Definition of the disease
Angioedema is a localized edema of sudden onset at the dermal-hypodermal or submucosal level. It is always transient but may last several days, disappearing without sequelae. The majority of angioedemas are non-allergic histamine associated or not with urticarial plaques and require only anti-histamine treatment. In rare cases (<1%), these are bradykinic angioedemas, in which case they require treatment in a Rare Disease Reference Center (RDC) of the Kinin Angioedema Reference Center (CREAK) network [1,2]. This is an orphan disease, belonging to the group of "rare diseases". C1-inhibitor deficiency or hereditary angioedema (HAE) is characterized by the occurrence of subcutaneous or submucosal edema, located anywhere in the body and particularly in the laryngeal and intestinal mucosa. These are non-allergic edemas favored by bradykinin. They are transient, lasting from 2 to 5 days, recurring but disappearing without sequelae. These angioedemas may be hereditary or acquired.
Unfortunately, there is no real data on hereditary angioedema (HAE) in the world. However, a national registry has existed for many years in which approximately 1200 cases have been recorded according to Dr. BOUILLET et al [3] (Internal Medicine, Grenoble University Hospital) and AMSAO1. It is estimated that between 1 in 10,000 and 1 in 50,000 people suffer from HAE [1,2].
Genetics
The disease is transmitted in an autosomal dominant fashion. Heterozygous forms are the most frequent: only two cases of homozygous patients have been identified in the world [3,4]. The mutation can be transmitted by one of the parents, himself a carrier of the mutated gene (75% of cases). The spontaneous mutation rate is about 25% de novo (without family history) [5]. More than 100 different mutations of the C1-inhibitor gene have been described [6]. There is an abnormality in the "p11, 2-q13" part of chromosome 11.
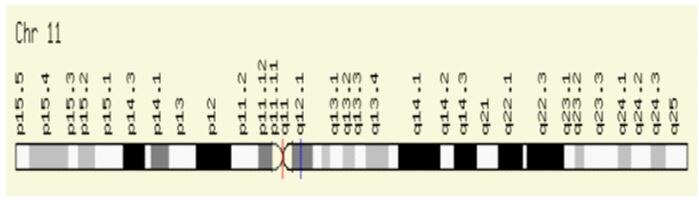
Figure 1: Chromosome 11 [7,8].
Epidemiology
All populations can be affected by hereditary angioedema (HAE), observations have been made in Anglo-Saxons, Armenians, North Africans, Danes, Swedes, Dutch, Israelites, Americans and Germans, without distinction of skin color (DU-THANH, 2011). No differences were noted between ethnic groups. The sex ratio is 1:1 [9]. The currently accepted prevalence of hereditary C1-inhibitor deficiency angioedema (AOHC1- INH) is about 1 per 50,000 inhabitants. The number of patients in France is estimated to be around 1500 cases [10].
Cause(s)
INH) deficiency or to an activation of the factor XII pathway of coagulation. There are various triggers for edema, the most common being even minor physical trauma [7]. Since attacks are often triggered locally, dental treatments are particularly dangerous because of the proximity of the airways. Psychological factors also play an important role in triggering. It is important to note that both factors, trauma and psychological factors, sometimes combine and even potentiate each other [7,9,10,11]. Although there is a correlation between attacks and hormonal factors, it is impossible to predict the role of menstruation, menopause or pregnancy, or the frequency and intensity of attacks in these patients. Each episode of abdominal pain during menstruation may pose a diagnostic problem (not knowing whether the patient is experiencing pain related to menstruation or an HAE attack). This hypothesis should be considered especially if it is a first episode in a patient with a family history of HAE [12,13,14,15].
In general, pregnancy seems to have a beneficial effect on the evolution of HAE, especially during the last two trimesters, but it can also be the cause of the revelation of the disease or be responsible for its aggravation. However, there is a paradox between the (traumatic) delivery and the frequent absence of oedema (resumption of HAE manifestations in the post-partum period). Thus, the evolution of HAE manifestations differs from one patient to another, but also within the same patient from one pregnancy to another.
Symptoms
The disease can occur at any age, including in children and adolescents. It consists of subcutaneous oedemas, of the color of the skin, or submucosal oedemas responsible for a sensation of tightness and painful tension. All areas of the integument can be affected: the face (lips, eyelids), extremities and genitals are frequent localizations [3,8,16]. Occasionally, they may be accompanied or preceded by an asymptomatic, non-pruritic, reticulated rash (erythema marginatum or reticulated erythema-like rash). When localized in the digestive mucosa, angioedema causes intense abdominal pain often associated with a sub-occlusive syndrome (nausea, vomiting). These recurrent episodes, without fever and without biological inflammatory syndrome, regress spontaneously in 48 to 72 hours [17,18].
When the edema reaches the upper airways (pharyngolaryngeal region, tongue), it can be life-threatening due to asphyxia, in the absence of appropriate treatment. The topography, intensity and frequency of attacks vary greatly over the course of a patient's life, from one patient to another and within the same family [19,20].
Triggering/Aggravating Factors:
Seizures are often spontaneous but can be triggered by physical trauma, including even minor medical procedures (e.g., dental work such as scaling) [18,20].
Other possible triggers are:
- Positive or negative emotions,
- Infections,
- Medication:
+Estrogens,
+Inhibitors of the bradykinin degradation pathway: angiotensin-converting enzyme (ACE) inhibitors, sacubitril valsartan (Entresto®), sartans, with potentiation when combined with mTOR inhibitors, gliptins or racecadotril.
+Thrombolytics [17,18].
Mortality
Upper airway attacks are fatal in 25% of cases in the absence of specific treatment [17,20].
Treatments
This is the current treatment regimen proposed for the management of patients with hereditary angioedema (HAE). A distinction is made between acute treatment of attacks, long-term chronic treatment, and short-term prophylaxis (e.g. before and after dental or surgical procedures) [21].
Prophylactic treatment
Prophylaxis should also be prescribed before urgent dental and surgical procedures and before childbirth. This consists of the use of Danatrol® 600 mg/d 10 to 15 days before the operation and/or
Berinert® 1 hour before the operation (20 U/kg). Berinert® must be available during the procedure (AYGOREN-PURSUN, 2009). Before certain trips, Danazol can also be prescribed, whose effectiveness begins several days after its introduction [21].
Background treatment
Long-term prophylaxis is in principle indicated if a patient has several criteria affecting quality of life, however each case requires individual assessment [9,10].
Danazol (or Stanazol) is most commonly used for chronic treatment. These attenuated androgens have the ability to increase circulating C1-INH levels. The side effects (virilization in women, liver disease, etc.) are dose-dependent, which is why the minimum effective dose is used, which differs from patient to patient, and the treatment requires annual liver monitoring. Depending on the clinical response Danazol will be used at a dose of 50 to 600mg/d. Use is possible only after contraindications have been eliminated [21].
Tranexamic acid is only used in cases of contraindication to attenuated androgens, for example in childhood. However, in some cases of non-histamine angioedema in which therapy has failed and the edema has been evolving for several months, the daily intake of tranexamic acid (1 g × 3/day) allows the disease to be controlled, sometimes with the total disappearance of the attacks. In these cases, investigations of the complementary system and C1inh were normal. The treatment requires annual hepatic and ocular monitoring [3].
Treatment of seizures
-Moderate seizures (3)
- Danazol (Danatrol®): 200 mg/8h
- Tranexamic acid (Exacyl®): 1 g/3h
-Treatment of severe/acute seizures [9,10].
Two treatments exist for the treatment of acute episodes.
-First, the administration of C1-INH, purified from human plasma (Berinert®). This is the emergency treatment for severe attacks, particularly laryngeal, abdominal or disabling skin attacks. It almost always stops the progression of the edema in a few minutes. The powder should be reconstituted with sterile water and injected or infused slowly intravenously [22].
This treatment is effective from the first 1/2 hour after injection (BERNSTEIN, 2008). However, it has limitations due to the fact that it is a blood-derived product. In addition, a relay by decreasing administration of Danazol is necessary (600mg/d for 8 days then 400mg/d for 8 days then 200mg/d for 8 days, then stop or resume the usual dose of Danazol if the patient was already treated) [21]. The other treatment for acute attacks (emergency treatment) is based on the use of Icatibant, a bradykinin B2 receptor antagonist via a 30mg subcutaneous injection from the age of 2 years [21].
Currently, a new molecule Ruconest is used, the active ingredient of which is conestat alfa, it is the first recombinant analogue of the human C1 esterase inhibitor (rhC1INH) produced by the recombinant DNA technique from the milk of rabbits transgenics. It is indicated for the treatment of acute attacks of angioedema in adults, adolescents and children (aged 2 years and older) with hereditary angioedema (HAE) due to C1 inhibitor deficiency esterase.
One vial of Ruconest powder for solution for injection contains 2100 units of conestat alfa, corresponding to 2100 units per 14 ml after reconstitution, i.e. a concentration of 150 units/ml. 1 unit of conestat alfa activity is defined as equivalent to the C1 esterase inhibitor activity present in 1 ml of normal plasma pool.
Important messages
-The management of hereditary angioedema requires regular follow-up by a CREAK referral physician. Patients should carry a rare disease care and emergency card and have emergency treatment available at home due to the potential severity of the disease.
-Treatments commonly used in histamine/allergic angioedema involving the VAS (antihistamines, epinephrine, and corticosteroids) are ineffective and their administration in HAE may delay specific management, increasing the risk of death.
-The clinical picture of HAE may be mistaken for a surgical emergency or even lead to a "blank" laparotomy.
Implications in dentistry
Proportion of patients followed in private practice
In recent years, more and more patients have been treated in private practices [18]. It has become necessary to evaluate the oral health care of these patients in France. For this purpose, a questionnaire was distributed through the Association des Malades Souffrant d'Angioedème (AMSAO), the only structure gathering patients with this rare disease in France.
The questions concerned different parameters: some are related to the disease (age of patients, forms, types of angioedema, age and circumstances of discovery, current treatments ), others are related to the experience of the patients in the sample in relation to oral care (information of the practitioners and their knowledge of the disease, difficulties for the patients to obtain oral care because of their pathology, place of care, possible prophylactic treatment, circumstances and localization of the attacks of AO due to care, patients wearing or requiring a dental prosthesis, information of the patients in the sample on the prevention of the oral diseases.
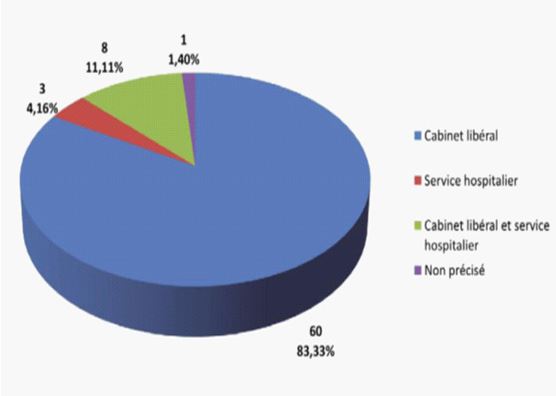
Figure 2: Locations of care (private practice, hospital setting) [18].
This study shows that 83% of patients are followed up in private practice, only 4% are followed up exclusively in the hospital, and 11% are followed up in both structures. We can therefore see that a very large number of patients with angioedema prefer to be followed up in private practice, hence the importance for the practitioner to know this disease [18].
According to LODI et al, out of 57 patients, some were treated by their attending dentist in town, others had recourse to general anaesthesia or hospitalization before dental treatment, only one case refused any treatment. The majority (86%) informed their dentist, 88% had a positive response from their dentist [23].
Angioedema attacks during dental treatment
The triggers for edema in these patients are not always easy to identify, as these edemas generally appear following trauma or stress, even if minimal, including oral care. Despite this laryngeal risk, the dental surgeon must manage these patients while limiting the risks. Dental surgeons must therefore be familiar with this rare but potentially life-threatening condition in order to be able to offer the patient a suitable multidisciplinary protocol [24].
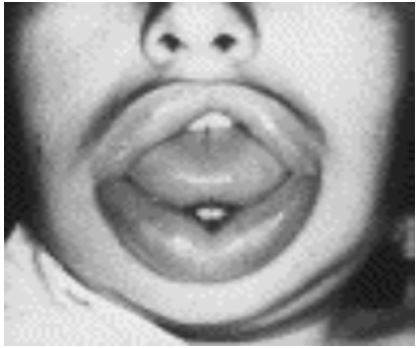
Figure 3: Edema of the lips and tongue in a 35 year old woman [24].
Location of the crisis
-Throat (34.61%),
-Lips (7.68%),
-Cheeks (19.23%),
-Face (30.76%). (18)
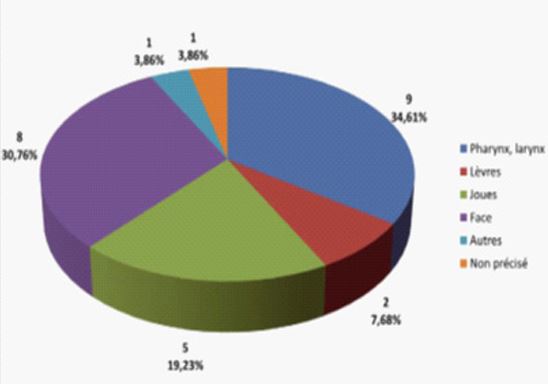
Figure 4: Location of angioedema [18].
Etiology of the crisis
Oral care is an important risk factor for patients suffering from AOB. This is mainly due to the physical stress caused by care or surgery, but also to the psychological and emotional stress that can be generated in many patients. In addition, there are infections of dental origin [18].
Oral surgery
According to LODI et al, 2001, out of 57 patients, half of the patients developed edema following dental care. The following figure shows the different types of care that would have triggered edema, following dental consultations [23].
-Surgery (60%)
-Anesthesia (24%)
-Conservative care (4%)
-No answer or no
-Recall (12%).
Figure 5: The different treatments that developed edema according to the patients included in the LODI et al. study [23].
According to the study on oral health care (2010), dental avulsions are the main cause of angioedema (46.2% in case of avulsion alone and 11.5% in case of avulsion associated with other treatments). Other surgical procedures (cystectomy, frenectomy...) were incriminated in 7.7% of cases. Thus, in 65.4% of cases, the occurrence of an OBE attack during oral care is generally attributed to surgical procedures. However, a simple injection for local anesthesia can also cause an OBE attack (7.7% of cases). However, during surgery or deep conservative care, local anesthesia is necessary and therefore constitutes an additional trauma [18].
Conservative care
It is true that seizures occur mainly after dental avulsion (46.2%), but also during conservative care (fillings, endodontic treatment, scaling, etc.) (19.2%). As mentioned above, a simple injection for local anesthesia can also cause edema, so it is preferable to perform as many conservative procedures as possible, taking into account the indications for local anesthesia. It is important to specify that the systematic use of local anaesthesia should be avoided, but that it remains indispensable depending on the type of treatment to be performed [18].
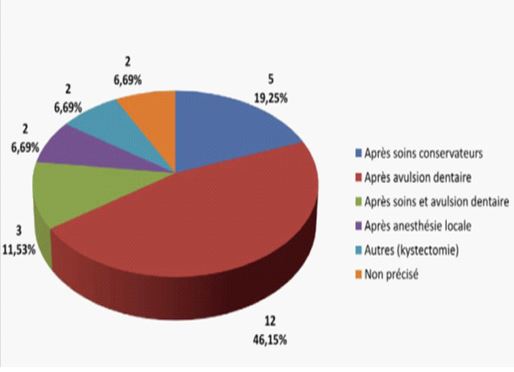
Figure 6: Aetiologies of the crisis [18].
Removable dental prostheses
It so happens that 22.2% of the patients wear a removable dental prosthesis. This is not a source of seizures (100%). Among the patients without dentures, only 3.6% would need removable dentures. Contrary to what one might suspect from its close and repeated contact with the gums, the use of removable dental prostheses does not seem to be contraindicated. However, their realization requires the taking of impressions and therefore the use of many materials. The dental surgeon will have to ensure, with great rigor, that the impression tray does not injure the gingival mucosa. The finish and adaptation of the prosthesis must be perfect to avoid any trauma [18].
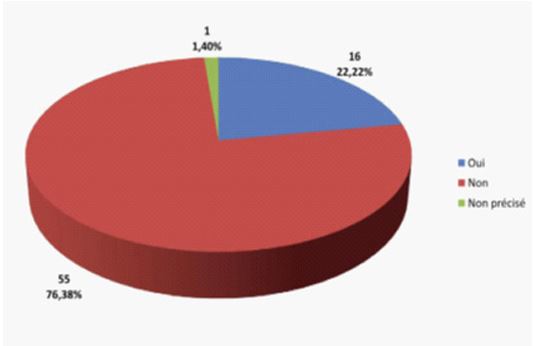
Figure 7: Proportion of patients with removable dentures [18].
Frequency
Slightly more than one third of patients (36%) have had an angioedema attack following dental treatment. The proportion of attacks that required hospitalization or emergency treatment was 46%. The edema mainly involved the pharynx and larynx (34.6% of cases) and the face (30.8% of cases) [18].
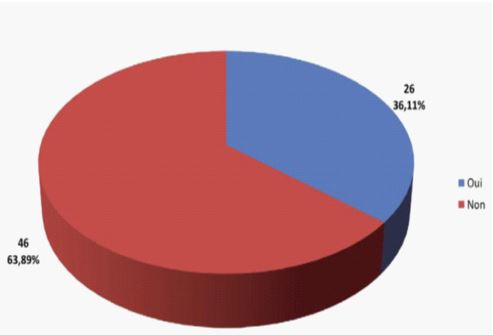
Figure 8: Proportion of patients who have ever had an angioedema attack [18].
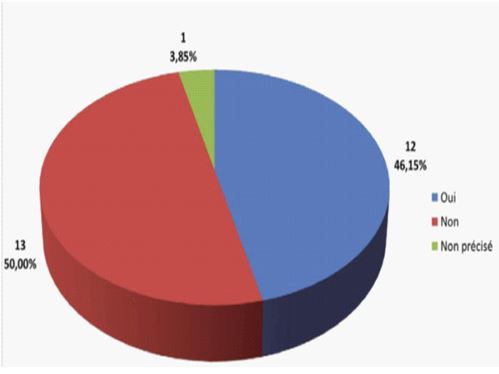
Figure 9: Proportion of attacks that required hospitalization or emergency treatment [18].
Dental care (extractions, conservative care, scaling, etc.) is a trigger for severe attacks and in particular laryngeal oedema, but does not occur systematically even after a dental extraction, as shown by MAEDA et al, 2003 [25]. In this study, only 2 out of 36 people had a seizure after dental extraction. However, there is a real relationship between dental extraction and laryngeal edema and one should never forget that there is a risk and take the necessary precautions [25].
Patient and practitioner information about the disease
General information
Dentists' knowledge of the disease
In 2010, a study on the evaluation of the oral health care of patients with OAH showed that 93% of the patients surveyed had informed their dentist of their disease. It should be noted that 88% of the practitioners were not aware of it. Despite this, 76% of the patients did not experience difficulties in obtaining dental care, compared to 22% who did [18].
Patient information
As mentioned earlier, the best way to avoid seeking dental care is good oral hygiene maintenance. In a study of oral health care for patients with OAH, only 60% of patients received oral health education and advice (brushing methods, use of dental floss, etc.) during their visit to the dentist, and only 50% were informed about the main causes of dental problems and periodontal disease [25]. However, 58% of patients feel the need to perform dental care [25] and 57% of patients think they are not sufficiently informed about the prevention of oral diseases [18].
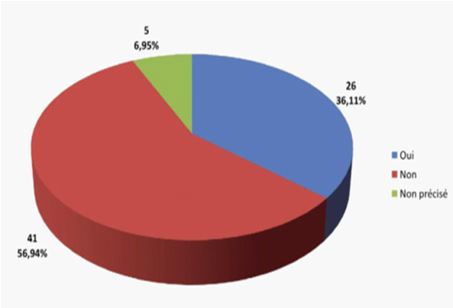
Figure 10: Proportion of patients who think they are sufficiently informed [18].
Management
Initial consultation
The Angioedema patient card
Patients deplore the lack of recognition of this pathology by the medical profession and by dental surgeons, which can have serious consequences. Indeed, in case of laryngeal edema, the prognosis is vital and it can be essential for the patient to have a recognized patient card that allows the doctor to ensure immediate appropriate management. Unfortunately, not all patients with angioedema have such a card. Currently, a card is available either through the AMSAO association (and then members have their referring physician fill it out), or through the referral center or the referring physician during the first consultation. This card includes several sections to guide the practitioner in his clinical approach. It includes recommendations in the event of an emergency, personal information about the patient (title, person to contact in the event of an emergency), medical information about the disease (date of diagnosis, type of deficiency, presence of background treatment, etc.) and the contact details of the patient's treating physicians and specialists [3,26].
The interview, a crucial step
During a first dental consultation it is essential to begin by questioning the patient, and it is even preferable to have the patient fill in a health questionnaire (to be dated and signed). It is also important to follow up any written health questionnaire with an oral questionnaire. If "angioedema" is mentioned, the practitioner should be challenged, and should ask for the patient's card (if he/she has one) or if he/she does not have a card, inquire about the following points.
-The type of disease (type I, II, III)
-Current treatment and background treatment
-Most frequently occurring clinical manifestations
-The current frequency (which can vary, as we have seen previously, according to the age of the patient and the frequency of attacks)
-The name of the referring physician.
Multidisciplinary care
It is therefore very important to contact the referring doctor as soon as possible or to contact specialists in this disease, in order to discuss the case and allow for the most appropriate treatment. This is a multidisciplinary approach [18].
This discussion should establish whether the treatment can be performed in the private dental practice or whether it must be performed in a hospital. This depends on the type of procedure planned (conservative care or surgery) and the patient's personal experience, the intensity of the attacks and the response to treatment. In both cases, the procedures must be scheduled and a precise protocol established [25].
In some cases, the patient may be unaware of his or her disease, so it is important for the practitioner to be able to detect and recognize signs of angioedema, allowing for a suspicion. These are essentially cases of de novo hereditary angioedema with mild attacks or never having worried, or acquired forms linked to the taking of specific drugs such as conversion enzyme inhibitors. The signs observed should be discussed with the patient's physician and tests should be considered to diagnose the disease.
The dental surgeon then has a real role in the diagnosis: in fact, the risk of developing edema following dental care is higher, so he can make the connection between dental care and edema [18].
What to do before any dental procedure or treatment
At present, the recommendations concerning dental care indicate hospital management. Indeed, given the laryngeal risk, the presence of a nurse, an anaesthetist, or a person trained to administer the intravenous C1-INH concentrate is recommended. However, according to the study evaluating the oral care of patients with OAH, private practice management is feasible for routine care (conservative care, scaling, fixed and removable prostheses) and, if possible, without local anesthesia [18].
It concerns patients who have few attacks and who respond well to prophylactic treatment. Although the risks appear to be lower in this case, an emergency procedure must be planned so that the patient can receive a specific treatment (C1-INH or icatibant) within a very short time [21].
Inpatient management is immediately necessary for patients who suffer from numerous seizures or who have had a seizure during dental care. This is especially important when surgery is planned [18].
The practitioner must also limit the risk of developing laryngeal edema by performing the least traumatic procedures possible, taking into account the prodromal signs, as well as the appearance of the disease in this patient (frequency, location, intensity of seizures).
Oral and dental prevention and angioedema
Motivating the patient to practice good oral hygiene remains essential. In order to avoid as much as possible the occurrence of AOB attacks in the dental office, it is important to insist on the prevention of oral diseases to limit the risk of caries and periodontal diseases. Indeed, if the patient has a rigorous hygiene and if he consults regularly, he normally avoids the "heavy" care as dental avulsions... Preventive advice would reduce the need for dental care (adequate brushing, dental floss, interdental brushes, mouthwash, and an annual visit to the dentist [18].
It starts at the first visit or even at every visit, because it is really important for the patient to understand the importance of good oral hygiene.
Scheduled intervention
Prophylactic treatment is necessary to prevent any severe edema or seizures that may be triggered during anesthesia or dental care.
-The different prophylactic treatments
The proportion of patients receiving prophylactic treatment prior to treatment is
56%. The following are mainly used:
- Danazol (60%) or tranexamic acid (10%),
- Danazol + tranexamic acid (6%).
- C1-INH concentrate is rarely used for prophylaxis (12%) [18].
-Prophylactic protocol
The patient must take Danatrol®: 600 mg/d (3 capsules per day) starting 7 to 10 days before the operation and continuing 5 days afterwards, then resume effective individual treatments. In children, 10 mg/kg [21]. If possible, perform a functional C1-INH assay for scheduled surgery or dental care; surgery will be possible if the level is greater than 50% of normal values.
Berinert® C1-Inhibitor Concentrate should be present in the anesthesia room or available near the site of the procedure. It is also recommended that a syringe of Firazyr® and standard resuscitation equipment be available in the procedure room. The availability of C1-inhibitor concentrate in sufficient dose must be checked before the procedure [26].
More and more studies propose an injection of Berinert® one hour before dental care:
According to [24], short-term prophylaxis was performed before 128 dental extractions in 48 of 171 patients. Only 16 of the 48 patients had 16 edematous episodes, including 9 patients in the face, 4 patients in the larynx (non-fatal) and 3 patients in both. In this study, 3 facial and 3 laryngeal edemas occurred despite prophylaxis with 1000 units of C1-INH concentrate.
However, a decrease in the occurrence of edema from 37.2% to 20.8% per patient and from 21.5% to 12.5% per location was observed following dental extractions. It should be noted that no side effects were observed following this prophylaxis. Prophylaxis with C1-INH concentrate therefore leads to a reduction in the number of edematous episodes at the facial and laryngeal levels following dental extractions in patients with hereditary angioedema due to C1-INH deficiency (BORK, 2011). C1-INH concentrate should therefore be considered for prophylaxis, especially in the context of surgery, but in theory it can be considered for all dental procedures [27].
Patients with the disease should be known to nearby emergency departments.It is important to be as non-traumatic as possible to reduce the risk of edema. The patient must know the mechanisms of his disease, recognize his symptoms, and know the good practices. He can then anticipate and better manage the various situations [26].
Lack of prophylactic treatment and crises
It is important to note that in 88% of cases, these attacks occurred when the patient had not received specific prophylactic treatment [18]. This means that 12% of the patients had a seizure following dental care, despite having received preventive treatment. (The preventive treatment was therefore probably insufficient or inappropriate).
The main reason for this lack of prophylaxis was lack of knowledge of the disease in half of the cases, the other reasons being various: 9% had never taken prophylaxis before, 4% had Exacyl available if necessary, 5% had no treatment available at the time, 4% thought that the background treatment was sufficient, 4% thought that it was impossible to have access to C1-INH concentrate before each treatment, 4% had forgotten to take a treatment [18].
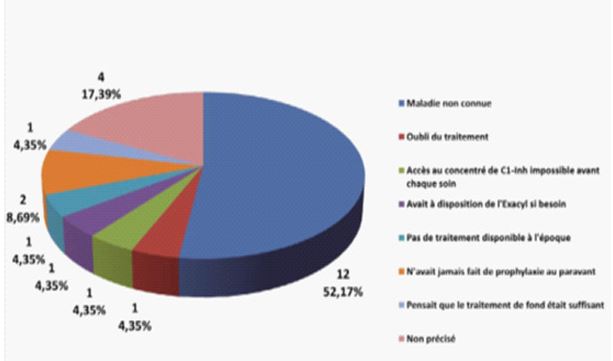
Figure 11: Reasons why the patient did not receive prophylaxis [18].
Unscheduled surgery
The patient must inform the anaesthetist and the practitioner of his or her illness and receive a C1-inhibitor concentrate (1000 U) in slow intravenous form at the time of induction of anaesthesia for urgent surgical procedures or 1 h before the procedure:
-500 U if patient < 50 kg
-1000 U if patient > 50 KG but <100k
-1500 U if > 100 kg.
The administration may be repeated in the hours following the procedure [28. In some cases, administration immediately after dental avulsion allows to avoid laryngeal edema without premedication before the procedure [25].
In dentistry, emergency procedures are mainly pulpitis (pulp inflammation), in which case it is very difficult to postpone treatment for 10-15 days in order to introduce prophylaxis. However, it is preferable to postpone the procedures and schedule them as soon as possible, thus allowing the prophylaxis protocol to be implemented [18].
Postoperative
If prophylaxis has been respected, the slightest suggestive symptom immediately following dental care may allow the practitioner to quickly recognize the occurrence of an angioedema attack (facial edema, laryngeal edema, severe abdominal attacks). This is important because it may occur in a patient who is unaware of his or her disease or who is suffering from a discrete form. It is also possible that the patient has forgotten to notify the practitioner. Dysphagia, discomfort in swallowing saliva, simple hoarseness and a decrease in voice that becomes weak or even inaudible, or wheezing should alert the dental surgeon and the physician and immediate emergency measures should be taken. Any edema of the face, which occurs during oral care, implies immediate measures (interruption of care, hospitalization for monitoring). In addition, any facial edema can potentially be accompanied by laryngeal edema [18].
If any of these signs are observed during the treatment session, the airway must be kept free with assisted ventilation and oxygen therapy if necessary, the patient must be referred immediately to a resuscitation unit (call the SAMU) and contact the doctor providing specialized care. Immediate therapeutic measures are then based on the rapid administration ofC1-INH concentrate (Berinert®) or icatibant (Firazyr®). Corticosteroids and anti-histamines are ineffective in this situation [21].
If no signs are observed during the treatment session, the edema may appear a few hours later, the latency period may be between 20 minutes and 30 hours. It is therefore important to have a postoperative surveillance (for example by a third person). This monitoring is preferably medical in the case of surgery [28].
Moreover, nowadays, according to the report of the Paris conference in 2011, patients are now advised to have Berinert® or Firazyr® at home, which allows for early treatment at the onset of the crisis. Patients have the right to self-administer these treatments. They can learn the necessary gestures in any reference center. Learning to inject the treatment oneself leads to more autonomy and freedom for the patient. There are also fewer delays between the onset of the crisis and the administration of the treatment, and therefore fewer hospitalizations. The repercussions on the patient's quality of life and mental health (depression, productivity, etc.) are therefore significant [29,30]. The Grenoble center has trained 45 patients in the last few months. Of 19 of them who needed an injection, 15 were self-administered. No patient went to the emergency room, which often avoids insecurity and stress. A single injection is sufficient in most cases. However, it is necessary to have several doses available, so that the product is always available at home (HAS: FIRAZYR).
The Grenoble center provides a protocol for self-injection. The presence of a third person (family or friend) is desirable. This person can inject in place of the patient if he or she does not feel able to do so, or be present after the injection, which allows the patient not to remain alone (possibility of discomfort due to stress or resulting from the crisis itself).
The injection is to be made in the abdominal region for icatibant. It must be slow, which minimizes local irritation. Redness and pain may occur at the injection site. They will disappear spontaneously (do not put anything on it).
Anxiety/stress and angioedema
Having the necessary products available at home or in the handbag in case of a severe attack, and learning the technical gestures for self-injection (intravenous or subcutaneous) contribute to making the patient autonomous and reduce his or her anxiety [11].
As the stress factor is important in the onset of this disease, it is recommended to reduce the patient's stress as much as possible and to use anxiolytics.
How to reduce the patient's stress level:
-Anxiolytics
Anxiolytics or minor tranquilizers are, as their name suggests, substances designed to combat anxiety and stress. They can cause drowsiness which makes them incompatible with precision activities (driving). They can induce dependence during prolonged treatment. In all cases, these medications, although they can be of great help from time to time, should not be used on a long-term basis.
There are different types of anxiolytics.
First of all, the benzodiazepines. They include LEXOMIL, LYSANXIA, TEMESTA, TRANXENE, VALIUM, or XANAX. These are the most commonly used anxiolytics, they produce very rapid effects. The side effects are relatively frequent: drowsiness, balance and memory problems, and above all, a significant risk of dependence when use lasts longer than 12 weeks. It is however preferable to use those with the shortest half-life.
Some anxiolytics are not part of the benzodiazepine family, for example hydroxyzine (ATARAX) is an anxiolytic of the antihistamine family. It can be used for anxiety, allergy and stress. Its side effects are similar to those of benzodiazepines. Its main advantage is the absence of dependence. Still among anxiolytics, we count meprobamate (EQUANIL), buspirone (BUSPAR), and captodiam (COVATINE). These last three are less used for different reasons, they are very different and have different properties and side effects [31].
Conclusion
The results of the study concerning the oral management of patients with angioedema show very different experiences. Angioedema can occur after surgical or conservative dental care. It seems important to note that many patients are treated primarily in private dental practices. Inpatient management is immediately necessary for patients who suffer from numerous attacks or who have had a previous severe laryngeal attack during dental care. This is especially important when oral surgery is planned.
It is the responsibility of the dental surgeon to manage these patients, while limiting the risks. To do so, it is important that he/she knows the disease and can propose an adapted multidisciplinary protocol to the patient. This discussion must establish, depending on the patient, whether the care can be performed in the private dental practice or whether it must be performed in a hospital. This depends on the type of procedure planned (conservative care or surgery) and the patient's personal experience, the intensity of the attacks and the response to treatment. In both cases, the procedures must be scheduled and a precise prophylactic protocol must be in place.
However, only half of the patients receive prophylaxis before dental work. More than a third of them have already had an angioedema attack following dental care, the prophylaxis being ignored often because of a lack of information from the patient or the dental surgeon. The practitioner may then have a key role in screening for the disease. The greatest risk is for patients who are unaware of their condition, as the first attack can be fatal. For oral surgery, the treatment is preferably carried out in a hospital and the prescription of a benzodiazepine-type anxiolytic before the procedure is recommended. Prevention is based on preparation protocols using danazol and/or tranexamic acid. C1-INH concentrate should be kept available in the treatment room, so that it can be administered in case of emergency. Some teams prefer to administer C1-INH concentrate systematically before each procedure.
In all cases, the necessary equipment for medical-surgical resuscitation (adrenaline, oxygen, intubation equipment, etc.) must be provided in the event that the patient has upper airway obstruction secondary to edema.
Treatment in a private dental practice is possible for routine care (conservative care, scaling, fixed and removable prostheses). Whenever possible, it is important to take into account the indications for local anesthesia. This management is for patients who have few attacks and respond well to prophylaxis. Even if the risks seem to be lower in this case, it is necessary to foresee during the planning of the care an emergency procedure so that the patient can receive a specific treatment (C1-INH or icatibant) in a very short time.
A complete and precise medical questionnaire allows us to learn about the manifestations of the disease in the patient. A true relationship of trust and listening must be established, and one must not hesitate to postpone a treatment session if the conditions are not favorable.
Protocol proposed in private practice:
- Possible prescription of an anxiolytic or implementation of different means to reduce stress (relaxation method, homeopathy...)
- Prescription of Danazol, from 10 days before to 48 hours after the operation (600mg/d or 3 capsules per day)
- And/or tranexamic acid for 48 hours, before and after the operation (3g/d or 6 tablets per day)
- Have C1-inhibitor (Berinert®) or Firazyr® available in the treatment room, which can be quickly administered in case of emergency by the patient or a third person.
- OR Administration of C1-INH concentrate prior to the procedure in certain cases (depending on the type of procedure and the manifestation of the disease in the patient). There is currently no consensus regarding the modalities of prophylactic treatments before oral care in these patients.
Contrary to what one might suspect, the use of removable dental prostheses does not seem to be contraindicated. However, their realization requires the taking of impressions and therefore the placing of many materials in the mouth. The dental surgeon will have to ensure, with great rigor, that the impression tray does not injure the gingival mucosa. The finish and adaptation of the prostheses must be perfect to avoid any trauma.
Finally, postoperative monitoring must not be neglected because edema can appear up to 48 hours after the treatment. This monitoring can be supported by a member of the patient's family. In order to avoid as much as possible the occurrence of AOB in the dental office, it is important to insist on the prevention of oral diseases to limit the risk of caries and periodontal diseases. Indeed, if the patient has a rigorous hygiene and if he/she consults regularly, he/she normally avoids "heavy" treatments such as dental avulsions.
Prevention should begin at the first visit. Prevention also includes patient education. In this area, 56.9% of patients consider that they are not sufficiently informed about the prevention of oral diseases. Therefore, regular check-ups with the attending dentist once or twice a year should be advised. The consultation will include:
A check-up of the pits and grooves and a possible sealing of deep grooves if necessary. -Retroalveolar control radiographs
-Supra- and subgingival scaling and cup polishing.
In general, patients suffering from angioedema are more receptive to this information since they know that their comfort of life depends on it. Indeed, many brochures are available to help patients better understand their disease. According to the president of AMSAO, "as soon as you have the right diagnosis, that you exchange with your doctor, that you have the treatment best adapted to your situation, and that you have learned to take care of yourself, you can live practically normally with this disease".
References
- Aygoren-Pursun E, Rusicke E, Martinez-Saguer I, Kreuz W. Acquired C1-Inhibitor Deficiency - Report of 18 Cases J. Allergy. Clin. Immunol. 2009; 123: S13.
- Dupond JL, Magy N, Gil H, Vuitton DA. L’oedème angioneurotique héréditaire: l’expérience du centre hospitalier universitaire de Besançon Rev. Fr. Allergol. 2001; 41: 276-277.
- Bouillet L, Mannic T, Arboleas M, et al. Hereditary angioedema: Key role for kallikrein and bradykinin in vascular endothelial-cadherin cleavage and edema formation J. Allergy Clin Immunol. 2011; 128: 232-234.
- Beltrami I, Zingale LC, Carugo S, Cicardi M. Angiotensin-converting enzyme inhibitor-related angioedema: how to deal with it. Expert Opin Drug Saf. 2006; 5 :643-9.
- Cicardi M, Pappalardo E, Duponchel C, Carugati A et al. Frequent de novo mutations and exon deletions in the C1inhibitor gene of patients with angioedema J. Allergy Clin Immunol. 2000; 106: 1147-1154.
- Wen L, Atkinson JP, Giclas PC. Clinical and laboratory evaluation of complement deficiency J. Allergy Clin Immunol. 2004; 113: 585-593.
- Nancey S, Andre F, Andre C, et al. Angioedema, Clinical and Biological Gastroenterology. 2001; 25: 896-904.
- Du-Thanh A, Raison-Peyron N, Guillot B. Bradykinin angioedema, Annals of Dermatology and Venereology. 2011 ; 138: 328-335.
- Frank MM. Complement disorders and hereditary angioedema J. Allergy Clin Immunol. 2010; 125: S262-S271.
- Frank MM, Lugar PL, Wu EY. Diagnosis and Treatment of an American Cohort of Patients with Hereditary Angioedema (HAE) Type III J. Allergy Clin Immunol. 2011; 127: AB102.
- Craig TJ, Levyr J, Wasserman RL. Efficacy of human C1 esterase inhibitor concentrate compared with placebo in acute hereditary angioedema attacks J. Allergy Clin Immunol. 2009; 124: 801-808.
- Caballero T, Bouillet L, Bork K, et al. European Consensus for Gynecologycal and Obstetric Management of Women with Hereditary Angioedema due to C1-Inhibitor Deficiency (HAE): Prehaeat J. Allergy Clin Immunol. 2007; 119: S12.
- Lambert H, Hennequin G, Stratzek J et al. Hereditary angioedema: two new family observations, Medical Annals of Nancy and the East. 1983.
- Laurent J, Lagrue G. Stratégie thérapeutique : un oedème angioneurotique héréditaire Gazette Médicale. 1987; 94: 12-13.
- Laurent J, Guinnepain MT. Les angio-oedèmes par déficit en C1 inhibiteur Revue Française d'Allergologie. 1997; 37: 585-594.
- Gompels MM, Lock RJ, Abinun M, et al. C1 Inhibitor deficiency : concensus document Clin. Exp. Immunol. 2005; 139: 379-394.
- Cicardi M, Levy RJ, Mc Neil DL, Li HH, Sheffer AL, et al. Ecallantide for the treatment of acute attacks in hereditary angioedema N. Engl. J Med. 2010; 363: 523-531.
- Chauvin T, Goichot B, Bui E et al. Evaluation of the oral care of patients with bradykinin angioedema Apropos of a survey of 72 patients. Med. Bucc. Chir. Bucc. 2010; 16: 67-77.
- Adams SJ, Ridley CM. Hereditary angioedema with easy bruising J. Roy. Soc. Med. 1984; 77: 522-524.
- Premetta MJ, Laudadio C, Craig T. Frequency and Types of Hereditary Angioedema Prodromes as Reported by Patients J. Allergy Clin Immunol. 2010; 125: AB165.
- Farkas H, Csuka D, Zotter Z et al. At-Home treatment of patients with acute attacks of hereditary angioedema with the bradykinin B2 Receptor-Antagonist Icatibant. J. Allergy Clin Immunol. 2011; 127: AB233.
- Klingebiel T, Rusicke E, Martinez-Saguer I, et al. Short-term prophylaxis with C1-inhibitor concentrate in patients with Hereditary angioedema prior to surgical procedures J. Allergy. Clin. Immunol. 2010; 125: AB164.
- Lodi G et al. Dental experience and self-perceived dental care needs of patients with angioedema Spec. Care. Dentist. 2001; 21: 27-31.
- Bork K, Staubach P, Witzke G. Prophylaxis with C1 Inhibitor Concentrate before Tooth Extractions in Patients with Hereditary Angioedema J. Allergy. Clin. Immunol. 2011; 127: AB265.
- Maeda S, Miyawaki T, Nomura S, Yagi T, Shimada M. Management of oral surgery in patients with hereditary or acquired angioedemas: review and case report Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003; 96: 540-3.
- Bouillet L, Boccon-Gibod I. L’angioedème héréditaire en question Phase 5. 2010; 40. ISBN: 978-2-35546-090-6.
- Atkinson JC, Frank MM. Oral manifestations and dental management of patients with hereditary angioedema J. Oral Pathol. Med. 1991; 20: 139-142.
- Rice S, Cochrane TJ, Millwaters M, Ali NT. Emergency management of upper airway angio-oedema after routine dental extraction in a patient with C1 esterase deficiency. Br. J. Oral Maxillofac. Surg. 2008; 46: 394-6.
- Rusicke E, Martinez-Saguer I, Klingebiel T, et al. Intraindividual and interindividual variations of symptoms in patients with hereditary angioedema J. Allergy Clin Immunol. 2007; 119: S312.
- Wilson DA, Castaldo AJ, Vernon MK, et al. Effect of Hereditary Angioedema: Health-Related Quality of Life, Depression, Productivity, and Social Consequences J. Allergy. Clin Immunol. 2009; 123: S142.
- Grima M. Les anxiolytiques Facult.Med. Strasbourg. Pharmaco. 2008.

