Case Report - Volume 3 - Issue 1
An insidious onset of Eosinophilic granulomatosis with polyangiitis: A case report
Righetti G1*; Genovese A1; Montinaro A2; Mastroianni F1
1U.O.C. Medicina Interna, Ospedale F.Miulli, Acquaviva Delle Fonti, Italy.
2U.O.C. Nefrologia, Policlinico di Bari, Italy.
Received Date : Jan 28, 2023
Accepted Date : Feb 20, 2023
Published Date: Feb 22, 2023
Copyright:© Giulia Righetti 2023
*Corresponding Author : Giulia Righetti, U.O.C. Medicina Interna, Ospedale F.Miulli, Acquaviva Delle Fonti, Italy.
Email: g.righetti@miulli.it
DOI: Doi.org/10.55920/2771-019X/1379
Abstract
Abstract: Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare small-vessel vasculitis, often associated with MPO p-ANCA (myeloperoxidase–perinuclear–anti-neutrophil cytoplasmic antibody) positivity. It is often difficult to diagnose.
Case description: A 73-year-old man went to the emergency room for asthenia and fever. In the anamnesis he reported nasal polyposis. For several months the patient had constitutional symptoms; blood tests showed increased indices of inflammation and anaemia. The patient was admitted to Internal Medicine. Blood culture,urine culture and specific blood chemistry tests for oncohaematological diseases were normal. In the absence of signs of infection, after resolution of the fever, the patient was discharged. After two weeks, he returned to the emergency room due to the reappearance of fever; blood tests showed hypereosinophilia, worsening of renal function. An electromyography showed the presence of mononeuritis multiplex. Specific blood chemistry tests were carried out: positive p-ANCA were found. Clinical and laboratoristic findings indicated the presence of EGPA; he also underwent a renal biopsy, that confirmed the diagnosis. Therapy was carried out with Corticosteroids and Cyclophosphamide; after two weeks blood test showed a rapid decreasement of creatinine values. On discharge the patient was afebrile; subsequent infusions of cyclophosphamide were scheduled.
Conclusions: EGPA is a rare and heterogeneous disease. The onset is often insidious, and require a careful differential diagnosis. Early diagnosis is important because it allows early treatment.
Keywords: Systemic vasculitis, anti-neutrophil cytoplasmic antibody-associated vasculitis, ANCA, EGPA
Introduction
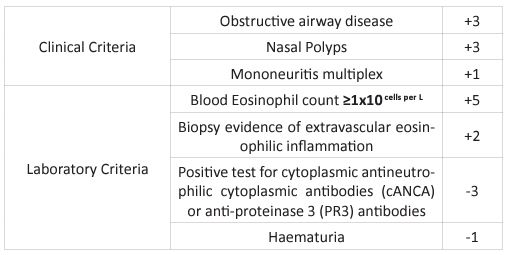
Eosinophilic granulomatosis with polyangiitis (EGPA) is a small-vessel vasculitic disease that can present with positive MPO p-ANCA (myeloperoxidase–perinuclear–anti-neutrophil cytoplasmic antibody). It is a rare condition that is often difficult to diagnose. Asthma, nasal polyposis, blood and tissue eosinophilia, and vasculitic inflammation defined a condition that has remained complex and heterogeneous. EGPA is part of the anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis syndromes (AAV). ANCA are identified in ∼40% of patients [1]. Immunofluorescence assays show a perinuclear pattern of ANCA. In most cases of EGPA, ANCA is directed against MPO rather than PR3 [2]. It is one of the rarest AAV, with an incidence of 0.8–4 per million persons and a prevalence of around 8.1–22 per million persons [3]. The 2022 American College of Rheumatology/European Alliance of Associations classification criteria is a validated tool used to assist in diagnosing EGPA [4] (Table 1). It is applied to patients who have a confirmed diagnosis of a small- or medium-vessel vasculitis; a score ≥6 is needed for a diagnosis of EGPA. Due to its low prevalence and limited epidemiological data, it remains challenging to diagnose and treat EGPA. We present the case of a 63-year-old man to whom EGPA with predominantly renal engagement has been diagnosed, characterized by a particularly insidious onset.
Case Description
A 73-year-old man, gardener by profession, with a previous chronic exposure to phos-phoric organs and pesticides, arrived in the department of Internal Medicine after access to the emergency room for intense asthenia, loss of appetite and weight loss of about 10 kg in two months. In the anamnesis, the patient did not report any particular pathologies, with the exception of nasal polyposis surgically treated about two months earlier. Diagnosis of first aid was: suspected intoxication with phosphoric esters. For sev-eral months the patient had constitutional symptoms, with fever and walking disorders with postural insta-bility and muscle pain in both lower limbs, associated with paraesthesia.
Blood tests showed increased indices of inflammation and anaemia. Blood tests performed in the emergency room showed iron deficiency anemia (Haemoglobin 7.5 mg/dl) reticulocytes 2.5%, mild renal impairment (creatinine 1.4 mg/dl) and increased inflammation indices (ESR 90 mm/h, RCP 18 mg/dL, D-dimers 4000). The patient was admitted to Internal Medicine to carry out the necessary investigations. During hospitalization, the patient presented fever; peak febrile blood culture and urine culture were normal. In the suspicion of an oncohaematological disease, specific blood chemistry tests were carried out: protein electrophoresis, serum and urinary immunofixation, tumor markers (CEA, CA 19.9, CA125, CA 15.3, alphafetoprotein, LDH, Jak2) were normal. Beta 2 microglobulin was slightly increased. Immunological lymphocyte subset typing was also performed showing activation of NK and CD8+ lymphocites.
An ultrasound of the abdomen was also performed to rule out splenomegaly; the examination did not show any abnormalities. In the suspicion of an oncological origin of the weight loss and inappetence, a total body CT was also performed, which showed presence of bilateral pleural effusion and hydronephrosis in the right kidney, in the absence of suspected abdominal or chest injuries. Subsequently the dosage of the Free light k and lambda chains in serum and urine was carried out, resulting increased but with preserved ratio. At the same time, steroid therapy was administered with gradual improvement of the clinical conditions. In the absence of signs of infection or oncohaematological pathology and after resolution of the fever, the patient was discharged with low-dose corticosteroid therapy with an indication to suspend the therapy after one month, and an indication to repeat the blood tests after two months. After two weeks, however, the patient returned to the emergency room due to the reappearance of asthenia and fever and the worsening of his general clinical conditions. Blood tests showed a persistently increased ESR (125 mm/h), neutrophilic leuko-cytosis, hypereosinophilia, further increase in beta 2-microglobulin, worsening of renal function (serum cre-atinine 3.9 mg/dl), increased ferritin, anaemia (haemoglobin 7.8 mg/dl), and marked iron deficiency. A gas-troscopy was performed which highlighted hyperemic gastritis. During hospitalization, the patient com-plained of worsening paresthesia in the lower limbs and burning pain sensation; an electromyography was therefore performed which showed the presence of mononeuritis multiplex.
Therefore, in the suspicion of a systemic vasculitis complicated by neuropathy, specific blood chemistry tests were started, with the search for autoantibodies (p-ANCA, c-ANCA): positive p-ANCA (MPO) were in fact found. The presence of hypereosinophilia, the history of nasal polyposis and the finding of a mononeuritis multiplex on electromyography, in association with asthenia and steroid-responsive fever, indicated the pres-ence of a systemic vasculitis, therefore confirmed by the positivity of specific autoantibodies (p-ANCA). In consideration of the serious renal involvement demonstrated by the constant worsening of serum creati-nine levels and the reduction of the glomerular filtration rate, the patient also underwent a renal biopsy. Histological examination on the biopsy showed one in seven glomerulus in global sclerosis, diffuse ischemic phenomena, segmental area of fibrinoid necrosis of the flocculus in one glomerulus and diffuse interstitial infiltrate containing numerous plasma cells and eosinophilic infiltrate with severe tubulitis and glomerular capillaritis; diffuse endothelial swelling (Figures 1, 2, 3 and 4).
After biopsy therapy was carried out with high dose corticosteroids (intravenous methylprednisolone 500 mg for three days, therefore 1 mg/kg of body weight) and Cyclophosphamide 1000 mg one shot. After one week blood test showed a marked improvement in laboratory parameters, with a rapid decreasement of creatinine value, until normalization after four weeks. On discharge the patient was stable, afebrile, autono-mous in walkings and movements. Subsequent infusions of cyclophosphamide and periodic blood tests were scheduled, according to validated schemes for the treatment of ANCA-associated vasculitis [5,6].
After two months of therapy blood tests showed normal values of hemoglobin, sodium, potassium and in-flammation indices, decreased creatinine; mild lymphopenia. The patient is currently about to undergo the fourth infusion of cyclophosphamide on an outpatient basis at the internal medicine and immunology day service of our hospital, is clinically stable, is independent in walking, and he periodically performs rheumatological outpatient checks; he discontinued steroid ther-apy with no evidence of disease exacerbations.
Table 1: The American College of Rheumatology/European Alliance of Associations eosinophilic granulomatosis with polyangiitis classification criteria (2022).
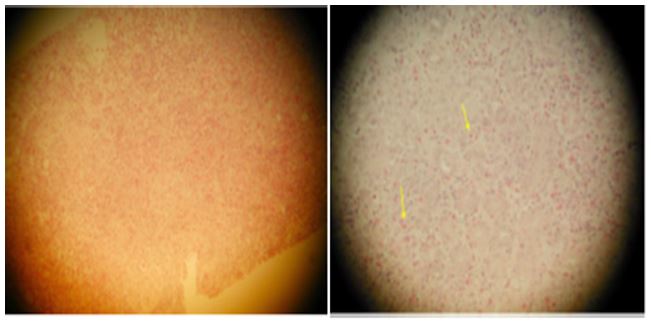
Figures 1 and 2: Hematoxylin Eosin: Interstitial infiltrate at small and large magnifications, rich in eosino-phils (cells with eosinophilic cytoplasm with eosinophilic granules, indicated by the arrow).
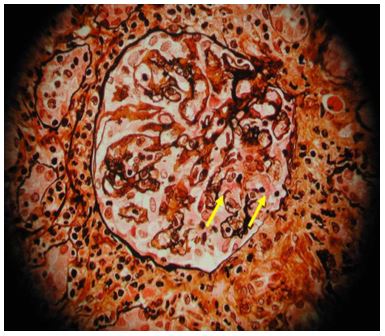
Figure 3: Silver Stain: Glomerulus with minute segmental area of fibrinoid necrosis (indicated by the arrow and rupture of the glomerular basement membrane). The fibrin is colored bright red.
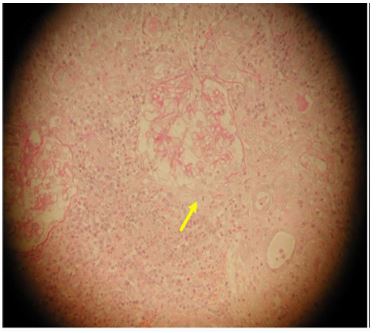
Figure 4: Periglomerular interstitial infiltrate, with rupture of Bowman's capsule in a glomerulus (arrowed). PAS staining.
Conclusions
EGPA remains a rare but complex and heterogeneous disease. In the future, outcomes may improve through early diagnosis, updates in classification criteria and the use of biologic agents (7). The onset of the disease is often insidious, with non-specific constitutional symptoms that require a careful differential diagnosis. Early diagnosis is important because it allows early treatment. Corticosteroids remain effective in inducing remission and maintenance of it, but their long-term side-effects can be deleterious. It is therefore necessary to set up as soon as possible a steroid-sparing immunosuppressive therapy. A deeper understan-ding of the pathophysiology of EGPA and its subgroups will support the development of personalised treat-ments in order to ensure effective treatment for the patients.
References
- Fagni F, Bello F, Emmi G. Eosinophilic granulomatosis with polyangiitis: dissecting the patho-physiology. Front Med (Lausanne). 2021; 8: 627776. doi:10.3389/fmed.2021.627776
- Austin K, Janagan S, Wells M, et al. ANCA associated vasculitis subtypes: recent insights and fu-ture perspectives. J Inflamm Res. 2022; 15: 2567–2582. doi:10.2147/JIR.S284768
- Mohammad AJ. An update on the epidemiology of ANCA-associated vasculitis. Rheumatology (Oxford). 2020; 59: Suppl. 3, iii42-iii50. doi:10.1093/rheumatology/keaa089
- Grayson PC, Ponte C, Suppiah R, et al. American College of Rheumatology/European Al-liance of Associations for Rheumatology classification criteria for eosinophilic granulomatosis with polyangiitis. Ann Rheum Dis. 2022; 81: 309-314. doi:10.1136/annrheumdis-2021-221794
- De Groot K, Afu D, Savage CO. EUVAS (European vasculitis study group). The value of pulse cyclo-phosphamide in ANCA-associated vasculitis: meta-analysis and critical review. Nephrol Dial Trans-plant. 2001; 16 (10): 2018-27
- Dhaygude A, Griffith M, Cairns T, McLean A, Palmer A Taube D. Prolonged treatment with low-dose intravenous pulse cyclophosphamide may reduce rate of relapse in ANCA-associated vasculitis. Nephron Clin Pract. 2004; 97 (4): c154-9.
- Laurino S, Chaudhry A, Booth A, Conte G, Jayne D. Prospective study of TNFalpha blockade with adalimumab in ANCA-associated systemic vasculitis with renal involvement. Nephrol Dial Trans-plant. 2010; 25 (10): 3307-14.

