Case Report - Volume 3 - Issue 2
A Retained Microcatheter Fragment in the middle cerebral artery: report of a rare complication
Matta Christian1*; Sleiman Joelle1; Sami Slaba2; Halim Abboud1
1Department of Neurology, Hotel-Dieu de France Hospital, Saint-Joseph University, Beirut, Lebanon
2Department of Radiology, Hotel-Dieu de France Hospital, Saint-Joseph University, Beirut, Lebanon.
Received Date : Feb 08, 2023
Accepted Date : Mar 01, 2023
Published Date: Mar 03, 2023
Copyright:© Christian Matta 2023
*Corresponding Author : Christian Matta, Saint Joseph University, HotelDieu de France Hospital, Blvd Alfred Naccache, Achrafieh, Beirut, Lebanon.
Email: Christianmatta18@gmail.com
DOI: Doi.org/10.55920/2771-019X/1387
Abstract
Mechanical thrombectomy is now a recommended treatment for large vessel occlusion in acute ischemic stroke. However, it is associated with a number of complications, which need to be minimized and effectively managed to maximize the benefits of thrombectomy. We describe an unusual and rare complication of microcatheter fracture after a successful thrombectomy for middle cerebral artery occlusion. Due to a lack of possibilities to remove it, we decided to manage it conservatively. Subsequently, the microcatheter fragment did not interrupt normal blood flow through the artery, and the patient has been doing well without neurological sequelae. Systematic reporting of such complications will aid in the design and development of thrombectomy devices in the future.
Background
The efficacy and safety of thrombectomy for acute large vessel occlusion have been demonstrated by several randomized studies and supported by class A, level 1 evidence [1]. The two accepted treatment options that can be used alone or in combination are stent retriever or aspiration thrombectomy [2, 3]. Although the use of the treatment is increasing worldwide, there are technical complications which include recanalisation failure, distal embolization to target or new vessel territory, risk of symptomatic or asymptomatic intracerebral hemorrhage and procedure-related complications [4].
We hereby describe a very rare and unique complication during aspiration thrombectomy procedure in a patient with acute ischemic stroke. The thrombectomy was complicated by fracture of the delivery microcatheter used during neurovascular intervention, which was retained as a foreign body in the middle cerebral artery (MCA). The purpose of presenting this case report is to describe this unusual complication that can not only lead to the failure of thrombectomy, but also leave a retained intraarterial thrombogenic micro catheter, which can potentially lead to complete arterial occlusion, clot propagation and stroke aggravation.
Case Presentation
A 50-year-old male with no known past medical history or medications presented to our emergency department with complete aphasia and right hemiplegia. History of present illness was as follows: the patient developed acute aphasia, and right hemiparesis noticed at work by his colleagues and he was transported to our department 60 minutes after detection. Physical findings were as follows: the height was 176 cm; body weight, 72 kg; blood pressure, 175/73 mmHg; heart rate, 78 bpm, irregular; body temperature, 36.8°C. The patient was suffering from right-sided weakness with complete aphasia and a National Institutes of Health stroke scale (NIHSS) of 16. His sugar level, prothrombin time and platelet counts were normal. Cardiac enzymes were normal with normal sinus rhythm ECG. Routine serum laboratory tests were within normal limits. Initial brain MRI and MRA showed acute anterior insula infarct on DWI without a visible acute hyper intense lesion on T2 Flair images and occlusion of the distal M1 segment of the left middle cerebral artery (MCA) (figure 1).
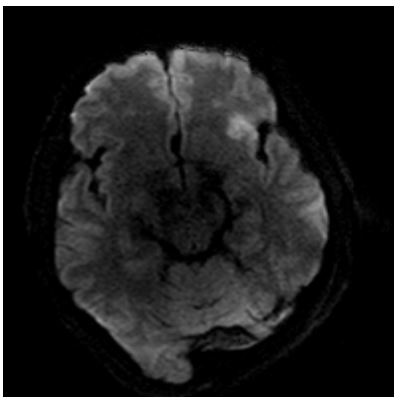
Figure 1: Axial diffusion weighted imaging (DWI) demonstrating diffusion restriction in the anterior part of the left insula (whitearrow).
We were not able to contact patient’s family to roll out contraindication to intra venous thrombolysis. Hence the patient was immediately transferred to the neurointerventional suite for endovascular treatment. General anesthesia was given as the patient was aphasic, and deemed unsuitable for the procedure under conscious sedation.
An 8 French (F) short sheath was inserted in the right femoral artery followed by the insertion of a 6 F 90 cm NeuronMax guide catheter (Penumbra, Alameda, USA). Initial stages of the procedure including navigation of the guide and intracranial support catheter into the internal carotid artery proceed without difficulty or obvious complications. The guide catheter was coaxially advanced over a 6 F Penumbra select catheter (Penumbra) into the left internal carotid artery. A diagnostic angiogram revealed occlusion of the proximal M1 Artery (Figure 2 a). Therefore, through the guide catheter located in the left cervical ICA, a micro catheter was navigated into the proximal MCA and occlusion was detected at M1 on angiography. Penumbra reperfusion catheter was navigated to the occluded region using Penumbra reperfusion catheter. Clot aspiration was done using the Penumbra Pump, and complete M1 recanilazation was achieved (figure 2 b).
While trying to retrieve the microcatheter, the distal part fractured spontaneously and remained stuck in M1. A follow-up control angiography showed a linear radiopaque foreign body identified in M1with T1C1 score 2 flow (figure 2c). Solitaire retrievers were used in an attempt to extract the wire. This strategy was unsuccessful.
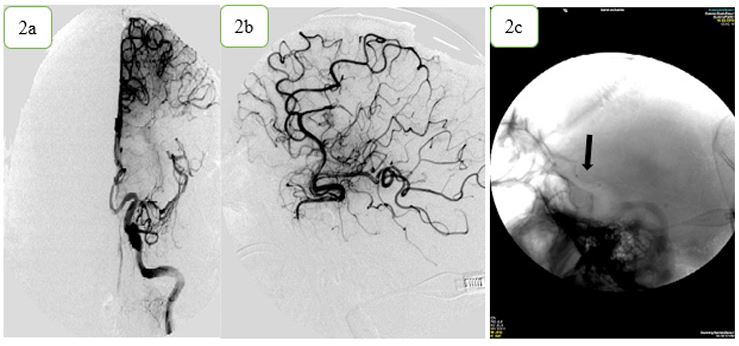
Figure 2: Cerebral angiogram shows a left MCA-M1 occlusion (2a), which was successfully recanalized with a 6 F Penumbra select catheter (2b). Control angiography shows a linear radiopaque foreign body identified in M1 (2c) (Black arrow).
On recognition of presence of foreign material in the MCA, our initial concern was to prevent MCA thrombosis. We therefore maintained the patient’s blood pressure relatively high to preserve adequate cerebral perfusion pressures, and gave an additional bolus of systemic heparin for adequate anticoagulation and prevention of clot formation on foreign materials.
Since no hemorrhagic changes were noted on head CT immediately after treatment and in consideration of the thromboembolic risk due to the entrapped microcatheter in vivo, the patient was subsequently managed with dual antiplatelet therapy and therapeutic heparinization. The patient was kept on mechanical ventilation and was transferred to neuro-intensive care unit. On the next day, routine non-contrast CT scan of the head was performed. Among ischemic changes, it showed a high metallic density located in the M1(MCA) with no hemorrhage (figure 3).
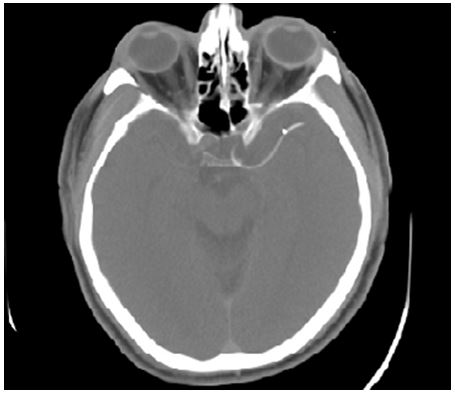
Figure 3: Non-contrast CT scan of the head shows a high metallic density located in the M1(MCA) with no hemorrhage (black arrow).
Transcranial duplex sonography showed normal left MCA blood flow (comparing with Right MCA).
The patient’s aphasia and right weakness gradually improved over the next 5 days. On post procedure day 8, the patient regained nearly normal speech and recovered his extremity weakness, having only residual mild clumsiness of the hand. Since he was suffering from continuous headache a brain CT showed small intracerebral hematoma in the frontal region, likely related to anticoagulation. Therefore, we decided to stop heparin and the patient was discharged home few days later on aspirin 100 mg daily and Plavix 75 mg/ day.
During the 3 months of post Mechanical thrombectomy follow-up, his outcome has been evaluated as modified Rankin scale (mRS) grade 0.
After the 12-month period, transcranial Doppler ultrasound shows normal flow velocity in both MCA. the patient continued aspirin 100 mg daily and was able to safely discontinue Plavix.
Discussion
Endovascular stroke treatment is an emergency neuro interventional procedure in which the main goal is the rapid recanalisation of the large vessel occlusion, as safely as possible. With growing evidence, the frequent use of Mechanical thrombectomy and concomitant complications is expected in the future. The most common complications related to endovascular therapy include: vessel injury, infection, device-related complications (vasospasm, arterial perforation and dissection, device detachment/misplacement); intracerebral hemorrhage; subarachnoid hemorrhage.
Here we report the cases of broken microcatheters in MCA artery. A multicenter case series estimated the rate of stent retriever detachment to be 0.66% in large-volume thrombectomy centers [5]. Stent detachment or fracture are classified into two main predisposing factors: Intrinsic factors related to structural features of the stent, device defects, the number of stent passes during the procedure and improper manipulation and usage; and extrinsic factors related to the nature and length of the thrombus or plaque; tortuous anatomy; arterial wall calcifications, and arterial stenosis [4, 6].
Upon microcatheter detachment, the treatment option will depend on an evaluation of the risks and benefits of recovering the detached stent.
The treatment options include: to leave the stent in place if there were no blood flow obstruction but intravascular foreign bodies can cause thromboembolic events and can also move and damage a vital organ or blood vessel, to retrieve the detached device by using a second device or by adopting a surgical approach for the extraction of the detached stent [4].
M.Teksam et al described a retained neurointerventional microcatheter fragment in the anterior communicating artery aneurysm in multi-slice computed tomography angiography. The fragment of microcatheter did not obstruct and did allow blood flow through the catheter fragment into the distal artery, avoiding neurological sequelae [7].
In our case, it is unclear why the the microcatheter fractured. One of the possible reasons could have been entrapment or over rotation of the distal tip of the catheter that produces a high tensile stress to the distal part [8]. Another possible reason for the catheter breaking may have been the production error of the microcatheter. However, whatever the mechanism was, we were unable to remove the stuck wire, believing that further forceful pulling could be disastrous. The obstruction did not cause any neurological complications and subsequent cerebral images showed conserved blood flow in the MCA. Given the probable endothelial damage, use of antiplatelets therapy with acetyl salicylic acid and a clopidogrel were used for one-year period to reduce the risk of stent and artery thrombosis.
In conclusion, we have experienced extremely rare complications from retained intravascular microcatheter after neurovascular procedures. If a fracture device cannot be removed, it might be better to leave it in the artery. Close radiographic follow-up with dual antiplatelets for one year is mandatory to observe any late migration of the retained microcatheter and to prevent any artery thrombosis.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article
References
- Powers WJ, Derdeyn CP, Biller J, et al. 2015 AHA/ASA Focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke 2015; 46: 3020-3035.
- Vargas J, Spiotta A, Fargen K, et al. Long term experience using the ADAPT technique for the treatment of acute ischemic stroke. J Neurointervent Surg 2017; 9: 437-441.
- Wong J, Telischak N, Heit J, et al. E-083 Acute stroke intervention for large vessel occlusion with combined stent retriever and suction thrombectomy (Solumbra technique): a retrospective analysis of 85 patients. J Neurointervent Surg 2016; 8(Suppl. 1): A86-A86.
- Balami JS, White PM, McMeekin PJ, et al. Complications of endovascular treatment for acute ischemic stroke: prevention and management. Int J Stroke. 2018; 13: 348-361.
- Masoud H, Nguyen TN, Martin CO, Holloway WE, Ambekar S, Yavagal DR, et al: Inadvertent stent retriever detachment: a multicenter case series and review of device experience FDA reports. Interv Neurol. 2016; 4(3-4): 75-82.
- Woodhouse JB, Uberoi R. Techniques for intravascular foreign body retrieval. Cardiovasc Intervent Radiol. 2013; 36: 888-97.
- Teksam, A. McKinney & C. L. Truwit. A Retained Neurointerventional Microcatheter Fragment in the Anterior Communicating Artery Aneurysm in Multi‐slice Computed Tomography Angiography, Acta Radiologica. 2004; 45(3): 340-343.
- Lotan C, Hasin Y, Stone D, Meyers S, Applebaum A, Gotsman MS: Guide wire entrapment during PTCA: a potentially dangerous complication. Cathet Cardiovasc Diagn. 1987; 13: 309-312

