Case Report - Volume 3 - Issue 2
Choroidal granuloma as an initial manifestation of systemic tuberculosis: A case report
Hala El B*; Yahya S; Taha B; Lalla O Ch
Ophthalmology A Departement, Hopital des spécialités, Rabat, Morocco.
Received Date : Feb 13, 2023
Accepted Date : Mar 07, 2023
Published Date: Mar 14, 2023
Copyright:© Hala El B 2023
*Corresponding Author : Hala El B, Ophthalmology A Departement, Hopital des spécialités, Rabat, Morocco.
Email: dr.elbelidi.hala@gmail.com
DOI: Doi.org/10.55920/2771-019X/1394
Abstract
Purpose:To describe the presentation and management of presumed ocular tuberculosis, successfully treated with anti-tubercular therapy alone.
Case report: Presumed tuberculous choroidal granuloma associated with serous retinal detachment healed after initiation of antituberculosis therapy without concomitant corticosteroid therapy.
Conclusion: Although corticosteroids are often used as add-on treatment for ocular tuberculosis, selected patients can be treated with anti-tuberculosis therapy alone with close follow-up.
Keywords: Ocular tuberculosis; choroidal granuloma; ATT; tuberculosis
Introduction
Tuberculosis (TB) is an infectious disease that primarily affects the lungs and rarely the eyes. Ocular tuberculosis (OTB) is a common cause of uveitis in North Africa and and can be challenging to definitively diagnose. Frequently, diagnoses of presumed OTB is based on a positive tuberculosis test, exclusion of other causes of uveitis, and careful consideration of the patient's history and fundus examination [1].
The most common presentation of OTB is posterior uveitis. The clinical phenotype of posterior uveitis in OTB includes choroidal nodules, choroidal granulomas, subretinal abscesses, serpiginous-like choroiditis and retinal vasculitis [2].
Choroidal tuberculoma is a rare form of OTB that raises both a diagnostic and a therapeutic challenges, especially when it occurs in the absence of other disease manifestations [3].
Case report
We report a case of a 50-year-old woman, she was seen in the emergency department with a one week history of decreased vision and pain in her left eye. Her medical history was noncontributory. The visual acuity measured by the Snellen chart was limited to 20/1000 in her left eye. The visual acuity in her right eye was 20/20. Ophthalmological examination of the left eye showed: 1+ cells in the vitreous, optic disc edema, an elevated nonpigmented mass that measured 3 disc diameters, superior and temporal to the optic disc (Figure 1(b)), and an exudative retinal detachment (Figure 2). The examination of the left right was normal. Fluoroscein angiography showed an early hypofluorescence of the choroidal lesion with late diffusion (Figure 1(d)). Chest CT and brain MRI were unremarkable. Orbit MRI showed an irregular left intraocular formation, 6mm thick, in high signal intensity on T1-weighted and low signal on T2, taking the macular and papillary region with infiltration of intra-conical retro septal fat, strongly enhanced after injection of gadolinium (Figure 3). Extensive uveitis laboratory testing were nonreactive or within normal limits. However, QuantiFERON-TB Gold test was positive. A diagnosis of presumed ocular TB was made, and she started a 6-month course of rifampin, isoniazid, pyrazinamide, ethambutol. The visual acuity in the left eye was 20/200 after 3 months of treatment, 20/40 after 6 months.
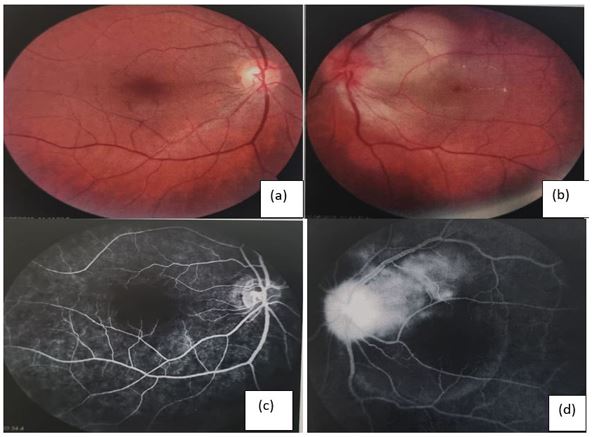
Figure 1: retinophotography of the right eye (a) and the left eye (b). Fluoroscein angiography of the right eye (c) and the left eye (d).
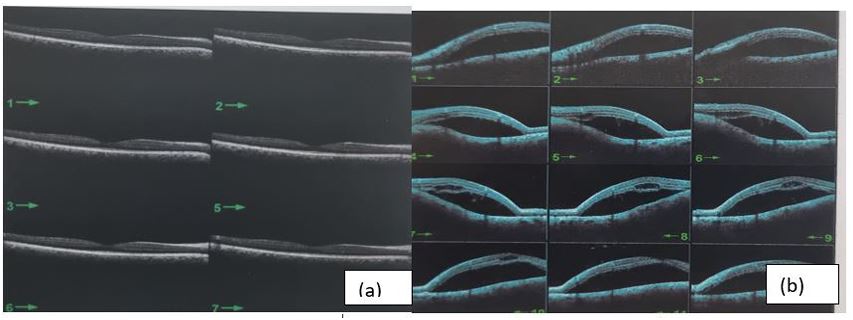
Figure 2 :SD-OCT of the right eye (a) and the left eye (b).
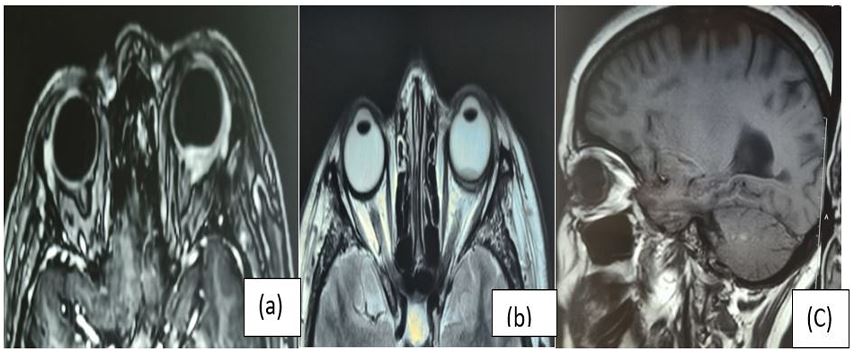
Figure 3: Orbit MRI showed an irregular left intraocular formation, 6mm thick, in high signal intensity on T1-weighted and low signal on T2 (b), taking the macular and papillary region with infiltration of intra-conical retro septal fat, strongly enhanced after injection of gadolinium (a).
Discussion
TB is an infectious disease caused by Mycobacterium tuberculosis. It is prevalent in developing countries, mainly in immunosuppressed individuals. Tuberculous granulomas have been described in HIV/AIDS and miliary tuberculosis, but also occur in immunocompetent patients. OTB is a rare event: it usually develops after hematogenous dissemination of the primary focus, but in rare cases it may also be secondary due to reactivation of bacilli [4]. The most common clinical presentation appears to be posterior uveitis, especially multiple choroidal nodules [5]. Less commonly, OTB may present as a single massive lesion measuring 4 to 14 mm in size at the posterior pole. Indocyanine green angiography has been recognized as the gold standard imaging modality for the diagnosis of choroidal granuloma [6]. Granulomas occupy the entire thickness of the choroidal stroma, remain hypocyanescent throughout the ICGA, and usually tuberculous granulomas detected on ICGA correspond to lesions seen on EDI-OCT. Invernizzi et al. showed that the measurement of choroidal granuloma with EDI-OCT can be used to monitor the response to therapy in patients with choroidal granuloma [7].
The differential diagnosis includes other ocular granulomatous inflammations. Solitary choroidal tuberculoma without systemic manifestations of TB presents a clinical challenge. Diagnosis of TB requires microbiological confirmation, which is impractical, so diagnosis is speculative and based on clinical and laboratory findings [8]. Treatment of OTB usually consists of anti-tuberculosis therapy (ATT) and corticosteroids. However, concomitant corticosteroid therapy may make it difficult to assess the effect of ATT alone on treatment response. In this case, the patient's choroidal lesions (suspected tuberculous granuloma) resolved significantly after ATT alone, supporting the original diagnosis [8]. Previous reports have also discussed the non-treatment of suspected OTB without corticosteroids. We conclude that treatment of suspected ocular tuberculosis with ATT alone can help confirm the diagnosis, if possible [9].
Conclusion
In most cases, the diagnosis of OTB is speculative due to the lack of definitive diagnostic evidence in microscopic or culture forms. In this setting, progressive or worsening inflammation after initiation of ATT presents a diagnostic challenge for the treating physician. In this case, different considerations could be drug resistance, misdiagnosis, or paradoxical responses. Each of these requires a different approach to management.
Declaration of Interest
The authors report no conflicts of interest
References
- Aksoy FE, Altan C, Basarir B. Multimodal imaging of a choroidal granuloma as a first sign of tuberculosis. Photodiagnosis and Photodynamic Therapy. 2019.
- Agrawal R, Gunasekeran DV, Grant R, et al. Collaborative ocular tuberculosis study (COTS)–1 study group clinical features and outcomes of patients with tubercular uveitis treated with antitu- bercular therapy in the collaborative ocular tuberculosis study (COTS)-1. JAMA Ophthalmol. 2017; 135(12): 1318-1327.
- Atul Arora , Deeksha Katoch , Sahil Jain , Simar Rajan Singh & Vishali Gupta. Yellow Subretinal Lesions following Initiation of Antituberculosis Therapy in A Tubercular Choroidal Granuloma: A Sign of Paradoxical Worsening?, Ocular Immunology and Inflammation. 2020.
- Salil Mehta, Remco PH Peters, Derrick P Smit & Vishali Gupta. Ocular Tuberculosis in HIV-infected Individuals, Ocular Immunology and Inflammation. 2020.
- Gupta V, Shoughy SS, Mahajan S, et al. Clinics of ocular tuberculosis. Ocul Immunol Inflamm. 2015; 23: 14-24.
- De Luigi G, Mantovani A, Papadia M, et al. Tuberculosis related choriocapillaritis [multifocal- serpiginous choroiditis]: follow-up and precise monitoring of therapy by indocyanine green angiography. Int Ophthalmol. 2012; 32: 55-60.
- Salman A, Parmar P, Rajamohan M, Vanila CG, Thomas PA, Jesudasan CAN. Optical coherence tomography in choroidal tuberculosis. Am J Ophthalmol. 2006; 142[1]: 170-172.
- AgrawalR, GunasekeranDV, GrantR, etal. Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the collaborative ocular tuberculosis study (COTS)-1. JAMA Ophthalmol. 2017; 135(12): 1318-1327.
- Hamade IH, Tabbara KF. Complications of presumed ocular tuberculosis. Acta Ophthalmol. 2010; 88(8): 905-909.

