Case Report - Volume 3 - Issue 2
Valsalva retinopathy during childbirth:A case report and literature review
Hala El B*; Yahya S; Taha B; Lalla O Ch
Departement of Ophthalmology, Hopital des spécialités, Rabat, Morocco.
Received Date : Feb 13, 2023
Accepted Date : Mar 08, 2023
Published Date: Mar 15, 2023
Copyright:© Hala El B 2023
*Corresponding Author : Hala El B, Departement of Ophthalmology A, Hopital des spécialités, Rabat, Morocco.
Email: dr.elbelidi.hala@gmail.com
DOI: Doi.org/10.55920/2771-019X/1395
Abstract
Purpose: To describe the presentation and the management of valsalva retinopathy during pregnancy.
Case report: A case of 30 years-old pregnant female with 36 weeks of gestation, presented with history of a sudden decrease in vision in her right eye during the labor. A clinical diagnosis of valsalva retinopathy was made based on clinical findings, laboratory test and imaging studies. Her right visual acuity had spontaneously increased with no active medical intervention.
Conclusion: Pregnancy is known to be a risk factor for valsalva retinopathy, and it should be considered in any pregnant woman who presents with sudden onset of painless vision loss preceding the onset of exertion. The prognosis for patients with valsalva retinopathy is generally promising.
Keywords: Valsalva retinopathy, pregnancy.
Introduction
Valsalva retinopathy is a specific form of retinopathy characterized by pre-retinal, subhyaloid, sub internal limiting membrane or vitreous haemorrhage [1]. It may occur unilateral or bilateral. It happens due to a sudden rise in intrathoracic or intra-abdominal pressure, which is transmitted to the perifoveal superficial retinal capillaries causing in their rupture a hemorrhagic detachment of the internal limiting membrane [2,3]. It is often encountered in young and middle-aged people who present with sudden diminution of vision which can vary from a subtle scotoma to total vision loss [4]. Pregnancy is known to be a risk factor for valsalva retinopathy. We hereby report a case of Valsalva retinopathy in a pregnant woman during her labor [5].
Case report
A 30-years-old pregnant woman at 36 weeks of gestation, experienced a sudden visual loss and floaters in her right eye during the labor. Her previous medical history was unremarkable. Her best corrected visual acuity was 20/20 in the left eye and hand motion at one meter in the right eye. Anterior segment examination was unremarkable. Pupil reactions were normal. Dilated fundus examination of the right eye revealed an enlarged pre-retinal subhyaloid hemorrhage in the macula (Figure 1). The patient had a spontaneous vaginal delivery. Blood pressure, full blood count, coagulation profile, fasting blood sugar and sickle cell tests were within normal limits. Additional tests for a hypercoagulable state and autoimmune diseases were negative. A clinical diagnosis of valsalva retinopathy was made and it was decided to observe the patient. Follow-up at one month, two, three and four month later revealed improvement in the best corrected visual acuity, with complete resolution of the macular hemorrhage.
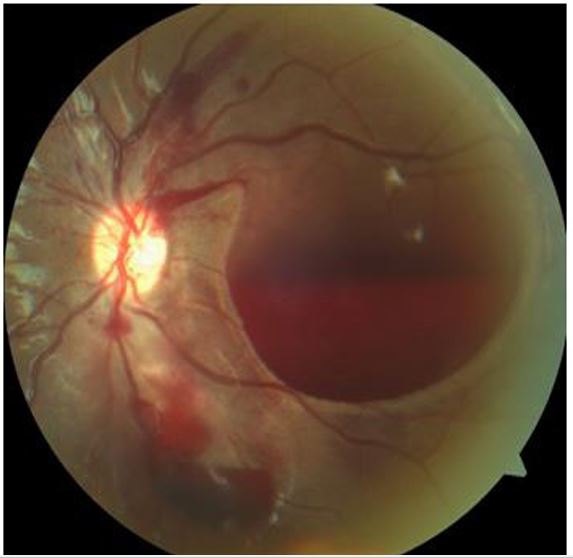
Figure 1: Retina fundus photographs of the right eye. An enlarged (3–5 disc diameters) preretinal hemorrhage located in the macula.
Discussion
Pregnancy is known to bring with it multiple hormonal, immunological, and hematological changes that increase the risk of bleeding and valsalva retinopathy. In addition, an enlarged uterus increases intra-abdominal pressure and compresses the veins, leading to increased pressure in the veins, further increasing the risk and the intensity of valsalva manoeuvers [2].
We identified only fifteen reported cases of valsalva retinopathy in pregnant women in the scientific literature. Five cases occurred due to vomiting [6,7,8], one case during defecation [9], two cases with a history of constipation [2,10], one case with a history of lifting heavy objects [10], one case after several coughs [11] and one case during yoga [12]. And only two cases of valsalva retinopathy occurred during labour [13,14]. All but two patients subsequently had natural vaginal delivery without ophthalmic complications [9,11]. Three authors report that they treated patients with Nd:YAG laser vitrectomy, which successfully resolved the bleeding [11,13,15]. One patient with bilateral valsalva retinopathy underwent pars vitrectomy [16]. All other patients received conservative treatment.
Treatment options for this condition include observation, neodymium:YAG (Nd:YAG) laser vitrectomy, and pars vitrectomy [2,13]. The choice depends on the size and the location and of the bleed. If the hemorrhage is smaller than the diameter of the disc, it resorbs spontaneously within a short period of time; therefore conservative treatment is generally recommended. In patients with major bleeding, spontaneous absorption of the bleeding may take longer, sometimes months. This may lead to permanent visual impairment due to changes in macular pigmentation, formation of the macular hole and epimacular membrane, or from toxic damage to the retina due to chronic exposure to hemoglobin or iron [17,18,19]. In these cases, it is recommended to use a Nd:YAG laser to direct the trapped blood through the focal opening into the vitreous cavity where it will be absorbed more quickly. It should be noted that laser therapy drainage is not possible in the case of coagulated premacular hemorrhage. Another point to be aware of is that being close to the retinal surface poses additional risks for laser treatments. This may include macular hole, retinal detachment, epiretinal membrane formation [18,21]. In this situation, vitrectomy is more effective and safer than other treatments for dense premacular hemorrhage. El-Defrawy et al. reported a conservative approach to retinal hemorrhage in pregnant women [20].
There is still much debate about the ideal timing to recommend intervention in this situation. There is also no general consensus on the optimal obstetric and anesthetic management of these pregnancies. Whether natural vaginal delivery might exacerbate bleeding remains controversial [22]. Possible interventions may include elective caesarean section to prevent progression by limiting venous pressure. There is no evidence that caesarean section is necessary. Natural vaginal delivery probably does not increase the risk of recurrent bleeding. Another factor to consider is that general anesthesia increases intraocular venous pressure, as hypercapnia and hypoxia cause retinal vasodilation [9,23]. Extubation can also cause a marked increase in venous pressure, followed by coughing [9]. It has also been shown that epidural anesthesia can be associated with preretinal hemorrhage by increasing cerebrospinal fluid pressure, it can increase retinal vein pressure[9,23].Our patient had normal vaginal delivery as recommendation by her obstetrician.
The prognosis for patients with valsalva retinopathy is generally promising. This situation just requires careful observation [24]. Vision usually returns to normal over time [21,23,24,25]. Some of these patients may experience poor vision due to the toxic effects of premacular hemorrhage on retinal pigment epithelium or epiretinal membrane formation.
Conclusion
Our case report highlights that valsalva retinopathy should be considered in any pregnant woman who presents with sudden onset of painless vision loss preceding the onset of exertion. The etiology of valsalva retinopathy in pregnancy is not limited to the triggers mentioned in the literature, but can also be caused by fairly innocuous behaviors.
References
- Chapman-Davies A, Lazarevic A. Valsalva retinopathy. Clin Exp Optom 2002; 85: 42-5
- Al-Mujaini AS, Montana CC. Valsalva retinopathy in pregnancy. J Med Case Reports 2008, 2: 101
- Rennie CA, Newman DK, Snead MP, Flanagan DW. Nd:YAG laser treatment for premacular subhyaloid hemorrhage. Eye (Lond). 2001; 15: 519-24
- 4 . Ulbig MW, Mangouritsas G, Rothbacher HH, Hamilton AM, McHugh JD. Long term results after drainage of premacular subhyaloid hemorrhage into the vitreous with pulsed Nd: YAG laser. Arch Ophthalmol. 1988; 116: 1465-9
- Conway MD, Peyman GA, Recaseus M. Intravitreal tPa and SF6 promote clearing of premacular subhyaloid hemorrhages in shaken and battered baby syndrome. Ophthalmic Surg Lasers 1999; 30: 435-41
- Callender D, Beirouty ZAY, Saba SN. Valsalva haemorrhagic retinopathy in a pregnant woman. Eye. 1995; 9: 808-9.
- Ramskold LAH. Valsalva retinopathy secondary to hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol. 2012; 162(1): 118-9.
- Tara F, Sharifi M, Hoseini E. Valsalva retinopathy in pregnancy: a case report. BMC Res Notes. 2015; 8: 67.
- Chidley KE, Law R, Vanner RG. Caesarean section following a recent retinal haemorrhage. Anaesthesia. 1998;53:483-5.
- Deane JS, Zaikas N. Letter to the Editor. Eye. 1997; 11: 137-43.
- Dağlioğlu MC, Coşkun M, Ilhan N, Tuzcu EA, Ari M, Ayintap E, Ilhan O. Posterior Hyaloidotomy by Nd:YAG Laser Application in a Patient with Postpartum Depression Caused by Valsalva Retinopathy. Case Rep Ophthalmol. 2013; 4(1): 64-8.
- El-Khayat AR. Valsalva haemorrhagic retinopathy in pregnancy after yoga. BMJ Case Rep. 2017; 2017: bcr2017221099.
- Ladjimi A, Zaouali S, Messaoud R, Ben Yahia S, Attia S, Jenzri S, Khairallah M. Valsalva retinopathy induced by labour. Eur J Ophthalmol. 2002; 12: 336-8.
- Eneh A, Almeida D. Valsalva hemorrhagic retinopathy during labour: a case report and literature review. Can J Ophthalmol. 2013; 48(6): e145-7.
- Jayaprakasam A, Matthew R, Toma M, Soni M. Valsalva retinopathy in pregnancy: SD-OCT features during and after Nd:YAG laser hyaloidotomy. Ophthalmic Surg Lasers Imaging. 2011; 17: 42.
- Mutha V, Narde HK, Chandra P, Kumar A. Valsalva retinopathy following normal vaginal delivery: 'bilaterality a rarity'. BMJ Case Rep. 2018; 2018: bcr2018224781.
- De Maeyer K, Van Ginderdeuren R, Postelmans L, et al. Sub-inner limiting membrane haemorrhage: Causes and treatment with vitrectomy. Br J Ophthalmol. 2007; 91(7): 869-72.
- Xie ZG, Yu SQ, Chen X, et al. Macular hole secondary to Valsalva retinopathy after doing push-up exercise. BMC Ophthalmol. 2014; 14: 98.
- Ramsay RC, Knobloch WH, Cantrill HL. Timing of vitrectomy for active proliferative diabetic retinopathy. Ophthalmology. 1986; 93(3): 283-89.
- El-Defrawy H, Sallam A, McKechnie CJ, Zambarakji H. Valsalva retinopathy in pregnancy. Should we treat? JRSM Short Rep. 2011; 2: 45.
- García Fernández M, Navarro JC, Castaño CG. Long-term evolution of Valsalva retinopathy: A case series. J Med Case Rep. 2012; 6: 346
- Wickremasinghe SS, Tranos PG, Davey C. Valsalva haemorrhagic retinopathy in pregnant woman: Implications for delivery. Acta Ophthalmol Scand. 2003; 81(4): 420-22.
- Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972; 70: 298-313.
- Park SW, Seo MS. Subhyaloidhemorrhage treated with SF6 gas injection. Ophthalmic Surg Lasers Imaging. 2004; 35: 335-37.
- Goel N, Kumar V, Seth A, et al. Spectral-domain optical coherence tomography following Nd: YAG laser membranotomy in Valsalva retinopathy.Ophthalmic Surg Lasers Imaging. 2011; 42(3): 222-28.

