Clinical Image - Volume 3 - Issue 2
Lymphangioleiomyomatose Pulmonaire (lAM) : Typical CT image Thoracic
Mribat M*; El Adioui G; Moutassim N; Nassar I
Central Radiology Department, CHU Ibn Sina, Mohamed V University, Rabat, Morocco
Received Date : Feb 17, 2023
Accepted Date : Mar 15, 2023
Published Date: Mar 22, 2023
Copyright:© Mribat M 2023
*Corresponding Author : Mribat M ,Central Radiology Department, CHU Ibn Sina, Mohamed V University, Rabat, Morocco
Email: meriememribat@gmail.com
DOI: Doi.org/10.55920/2771-019X/1400
Clinical Image
Pulmonary lymphangioleiomyomatosis (LAM) is a rare lung disease characterized by interstitial proliferation of cells resembling dystrophic smooth muscle cells. It can occur sporadically or as part of a genetic disease; tuberous sclerosis of Bourneville.
This condition mainly affects young women of childbearing age, however it can occur after menopause [1].
LAM is characterized by progressive lung cystic destruction, frequently associated with renal angiomyolipomas. Patients with AML generally present with recurrent pneumothorax due to cyst rupture, or progressive dyspnea that progresses to chronic respiratory failure [2].
Imaging, in particular the high-resolution scanner, plays a key role in the diagnosis and follow-up of patients with AML. Typical appearance of LAM on the HR chest CT scan is characterized by the presence of multiple cysts (nb >10), rounded, with regular contours, whose size varies between 2 to 6 mm in diameter, with regular thin walls not exceeding 2mm in diameter. thickness [3,4] (Figure 1, 2). Cystic lesions are homogeneously and diffusely distributed within normal lung parenchyma (Figure1, 2).
A very discreet Interstitial Syndrome can be associated. The presence of nodules with well-defined contours is found in patients with tuberous sclerosis [5]. Infracentimetric mediastinal adenomegaly are frequent. The main complications to look for on the chest CT scan: pneumothorax and chylothorax. Chest CT is also performed as part of screening in patients with TSC looking for radiological signs of AML [6].
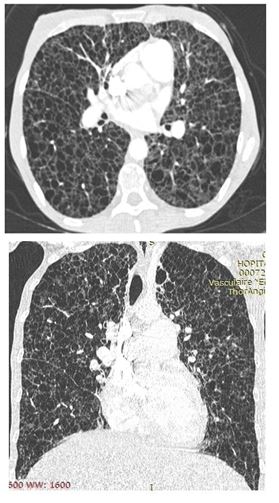
Figure 1 and 2: Chest CT; axial and coronal section; showing multiple diffuse cystic lesions in favor of pulmonary lymphangioleiomyomatosis.
AML should be differentiated from other cystic lesions of the lung, mainly histiocytosis X; which affects the smoking subject with a characteristic appearance on the scanner of a cyst of irregular lace shapes, predominant in the middle and upper lobe, but the distinction sometimes remains difficult in the advanced stage of the disease, and also with lymphocytic interstitial pneumonia (LIP) which is characterized by ground glass patches around the cysts, distributes around the bronchovascular sheaths. Although the chest CT scan may be compatible or characteristic of AML, the definitive diagnosis is based on the combination of clinico-radiological criteria and the histological confirmation obtained by lung biopsy or biopsy of a lymph node or lymphangiomyoma [6].
References
- Frognier R, Cottin V, Cordier JF. Women and interstitial lung diseases Eur Respir Mon 2003; 25167-25189.
- Urban T, Lazor R, Lacronique J, Murris M, Labrune S, Valeyre D, et al. Pulmonary lymphangioleiomyomatosis. A study of 69 patients. Groupe d’Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM “O” P) Medicine (Baltimore) 1999; 78: 321-337.
- Avila NA, Chen CC, Chu SC, Wu M, Jones EC, Neumann RD, et al. Pulmonary lymphangioleiomyomatosis: correlation of ventilation-perfusion scintigraphy, chest radiography, and CT with pulmonary function tests Radiology 2000; 214: 441-446.
- Muller N.L., Chiles C., Kullnig P. Pulmonary lymphangiomyomatosis: correlation of CT with radiographic and functional findings Radiology 1990; 175: 335-339.
- Franz DN, Brody A, Meyer C, Leonard J, Chuck G, Dabora S, et al. Mutational and radiographic analysis of pulmonary disease consistent with lymphangioleiomyomatosis and micronodular pneumocyte hyperplasia in women with tuberous sclerosis. Am J Respir Crit Care Med. 2001; 164: 661-8.
- Johnson SR, Cordier JF, Lazor R, Cottin V, Costabel U, Harari S et al. European Respiratory Society guidelines for the diagnosis and management of lymphangioleiomyomatosis (LAM). Eur Respir J. 2010.

