Case report - Volume 3 - Issue 2
Refractory Multifocal Coronary Artery Spasm : Case report and literature review focusing on the treatment
Mahmoud A1; Ali T2*; Ali El S3; Mahmoud K1
1Cardiology fellows at Lebanese university, Lebanon.
2Cardiologist at Al Zahraa hospital university medical center, Lebanon.
3Head of the cardiology department at Al Zahraa hospital university medical center, Lebanon
Received Date : Feb 20, 2023
Accepted Date : Mar 22, 2023
Published Date: Mar 29, 2023
Copyright:© Ali T 2023
*Corresponding Author : Ali T, Cardiologist at Al Zahraa hospital university medical center, Lebanon.
Email: alitfayli1900@gmail.com
DOI: Doi.org/10.55920/2771-019X/1405
Abstract
Background: Coronary vasospasm refers to when a coronary artery suddenly undergoes either complete or sub-total temporary occlusion. Though it has long been regarded to be benign, patients with coronary spasm may present with myocardial infarction, malignant arrhythmias and even sudden cardiac arrest. Spontaneous severe multivessel spasm, mimicking severe obstructive coronary artery disease remains a challenge in medical practice .Thus, high index of suspicion is crucial for diagnosis and timely management.
Case presentation: We describe a 42-year-old woman with recurrent acute coronary syndrome due to CAS in different coronary arteries.
Conclusions: This report highlights the importance of routine use of intracoronary nitroglycerin during coronary procedure in order to exclude the possibility of coronary spasm. And it is equally important to resolve uncertainty about the best strategy to deal with refractory and intractable coronary spasm.
Keywords: Multivessel coronary artery spasm; Refractory coronary spasm; Acute coronary syndrome; Intracoronary nitroglycerin.
Abbreviations :
ACS : Acute coronary syndrome
CAD : Coronary artery disease
CAS : Coronary artery spasm
CCB : Calcium channel blockers
LAD : Left anterior descending artery
MACE : Major adverse cardiac event
NSTEMI : Non ST elevation myocardial infarction
PCI : Percutaneous coronary intervention
VSA : Vasospastic angina
Introduction
Vasospastic angina, which was previously referred to as Prinzmetal or variant angina, is a clinical entity characterized by episodes of rest angina that promptly respond to short-acting nitrates and are attributable to coronary artery vasospasm (1).
The diagnosis of diffuse multifocal spasm can be quite challenging and it could be easily mistaken for diffuse coronary artery disease , leading to unnecessary interventions.
Long-term survival of CAS patients is believed to be good, especially in those who respond well to treatment. However, predictors of poor prognosis include the presence of underlying coronary atherosclerosis, spasm of multiple coronary arteries, refractory cases despite intensive treatment and severe attacks associated with myocardial ischemia, and /or life-threatening arrhythmias (2).
We report a case of complex form of coronary artery spasm occurring in a middle-aged women characterized by severe life-threatening attack, refractory to optimal conventional medical therapy and affecting multiple coronary arteries simultaneously.
Case presentation
A 42-year-old women non smoker , very well educated presented to our emergency department for the onset of an acute severe retrosternal chest pain irradiated to the left arm lasting about 4 h. She had history of well controlled asthma on a combination of Beclometasone and Formoterol (Inuvair) . She denied any history of hypertension , diabetes , dyslipidemia or any others cardiovascular risk factors .There was no history of illicit drugs or alcohol abuse and no family history of premature CAD or aortic disease.
Two years prior to this presentation, she reported admission to another hospital where she was critically ill , in severe distress and she underwent PCI to her proximal LAD . Since that time , she was placed on ASA 80 mg daily , Atorvastatin 40 mg daily and diltiazem 60 mg twice daily .
On admission, the patient appeared ill , with persistence of moderate chest discomfort. She was afebrile , the pulse was 85 b.p.m., the blood pressure 150/90 mmHg in both arms and the oxygen saturation 97% while she was breathing ambient air.
Her physical examination was unremarkable and no clinical signs of heart failure were present.
Laboratory investigations drawn on arrival showed that high-sensitivity Troponin I levels were increased ( 3.896 ng/mL, reference range <0.015 ng/mL) , others important factors such as complete blood count (CBC), blood sugar (BS), total cholesterol , creatinine , electrolytes , prothrombin time (PT), partial thromboplastin time (PTT), and international normalized ratio (INR) were at normal levels.
A urine drug screen revealed no evidence of benzodiazepines, opiates , cocaine or its metabolites.
A 12-lead electrocardiogram showed diffuse ST-segment depression with hyperacute T wave in leads II, III, aVF, and V2 through V6
Based on the previous findings , the diagnosis of ACS-NSTEMI was made and patient was admitted to the Cardiology unit .
Urgent coronary angiography revealed a very tight stenosis 99% at the mid left anterior descending artery just at the exist of the previous stent with almost complete obliteration of the proximal RCA ( Figure 1A,1B) . However, after administration of intracoronary nitroglycerine, a complete recover of vessels patency was noted, and a diagnosis of epicardial spasm was made (Figure 1C,1D). Due to the complete resolution of intracoronary narrowing and angiographically no evidence of residual stenosis or haziness , intracoronary imaging was not performed .
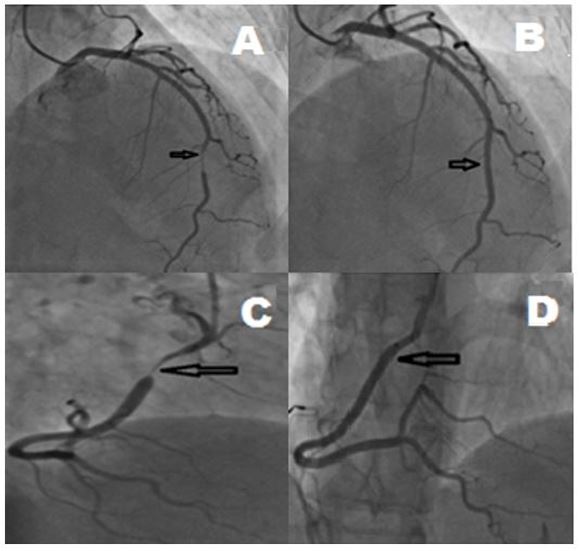
Figure 1: Coronary angiogram of the patient, Panel A: Left coronary injection, significant narrowing of the left anterior descending artery in distal part (arrows). Panel B: The left anterior descending artery after administration of intra coronary nitroglycerin (arrows). . Panel C: Right coronary injection, narrowing of right coronary artery in proximal part (arrows) . Panel D : The right coronary artery after administration of intra coronary nitroglycerin (arrows).
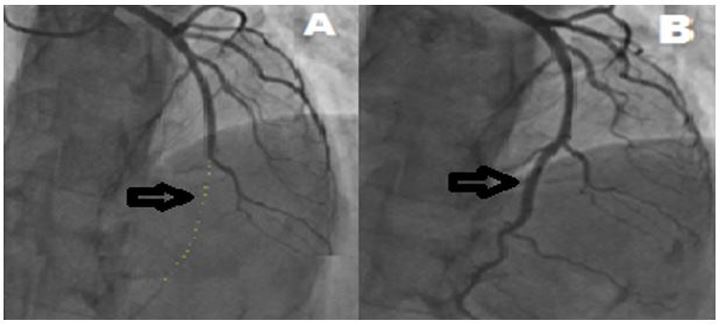
Figure 2: Coronary angiogram of the patient, Panel A: Left coronary injection, subocclusive stenosis 99% ( TIMI Flow 1) (arrows). Panel B: The left anterior descending artery after administration of intra coronary nitroglycerin (arrows).
Unfortenately we were unable to procure the angiograms performed prior to her PCI but we assume that the native anatomy was probably similar to that seen prior to the nitroglycerin injection on the current angiogram.
Pre-discharge echocardiography revealed no regional wall motion abnormalities and normal valves .
The patient remained stable throughout her hospital stay and was discharged home 3 days later on a regimen of ASA 80 mg daily , Atorvastatin 20 mg daily , diltiazem 240 mg daily before sleep , and long acting isosorbide mononitrate 30 mg daily planning a clinical follow-up at 3 months.
However, 2 months later, the patient came back to the emergency department of our institution with recurrent chest pain and dyspnea arising 3 h before arrival. Her initial vitals were unremarkable. Her initial ECG performed in triage, showed normal sinus rhythm with hyperacute T wave changes in V2-V6; Her laboratory data were unremarkable except for a mildly elevated troponin-I ( 0.093)
Repeat coronary angiography showed a subocclusive stenosis 99% ( TIMI Flow 1) at the distal LAD ( Figure 2A) , again after the intracorobary injection of nitroglycerin , the lesion disappeared completely ( Figure 2B).
Thyroid function, vasoactive intestinal peptides, and urinary catecholamine levels were all normal. No primary cause for vasospasm was discovered.
The patient was discharged with complete relief of her symtomps on a regimen of a regular oral ASA 80 mg daily , Atorvastatin 20 mg daily , diltiazem 360 mg daily before sleep , long acting isosorbide mononitrate 60 mg daily and nicorandil 20 mg twice daily (3).
Discussion
Spontaneous coronary artery vasospasm is described as a transient narrowing or occlusion of an artery. It is a rare type of angina called variant angina pectoris (or Prinzmetal’s angina) which was first described in 1959. It occurs most often when the person is resting , typically at night during sleep and mainly in younger age (4).
Coronary artery spasm may be triggered by emotional stress, exposure to cold, cocaine use, or heavy smoking… and although the underlying pathophysiological mechanisms are still largely unclear, autonomic nervous system, endothelial dysfunction, chronic inflammation, oxidative stress, and smooth muscle hypercontractility are mostly involved (5), (6).
Coronary artery spasms are usually brief , temporary and benign . However, they can potentially lead to further heart complications, such as a myocardial infarction, malignant arrhythmias and even sudden cardiac death in severe forms (7).
Multivessel coronary spasm is very uncommon , and easly it could be mistaken for diffuse obstructive atherosclerotic disease especially among patients with multiple cardiovascular risk factors or those who are unstable upon presentation.Therefore it might be result in unnecessary revascularization such as PCI or even coronary artery bypass grafting (CABG) , so it is imperative to diagnose this condition correctly.
There are some cases reports in the literature where unifocal or/and multifocal coronary artery vasospasm was mistaken for obstructive diffuse atherosclerosis and therefore unnecessary invasive procedures were performed (8) (9).
Therefore we suggest routine administration of intracoronary nitroglycerin during diagnostic coronary angiography in all patients with coronary stenosis or obstructions to better evaluate the extent of coronary disease and to prevent unnecessary procedures.
Refractory vasospastic angina is when angina continues despite being on a combination of a maximum dose of two medications (usually CCB and nitrate). When this occurs, and due to the lack of clear guidelines, unconventional treatment modalities based on expert opinion may be employed for symptomatic relief (10).
In our case severe coronary spasm persist despite using a high dose of CCB, long acting nitrate and statin. Nicorandil was an effective salvage therapy added with no relapse over 12 months.
The conventional management of vasospastic angina involves lifestyle changes, use of established pharmacological therapies, avoidance of aggravating factors and possibly the use of percutaneous coronary intervention (PCI) for associated fixed obstructive CAD. In some patients with refractory vasospastic angina, these therapies have limited efficacy, so that alternate approaches are warranted.
It is well established that lifestyle intervention plays an important role in terms of improving symptoms and decreasing attacks in patients who are suffering from VSA . Smoking cessation is imperative in patients with VSA , giving that smoking is strongly associated with endothelial dysfunction leading to coronary spasm. A lot of published tials has been shown that smoking cessation is highly advisable to prevent recurrent angina especially if it is associated with aerobic exercise training (11), (12).
It is also crucial to avoid all VSA precipitating factors , such as : mental stress and psychological factors ( 13) , alcohol ingestion ( 14), taking into consideration that the literature is a little bit conflicting because episodes of VSA have also been reported to be alleviated by alcohol consumption and aggravated during alcohol withdrawal ( 15) and the use of pharmacological molecules, such as cocaine , ephedrine and sumatriptan , ergonovine, ergotamine, amphetamines and marijuana etc.) ( 16) , some chemotherapy agents such 5FU and environmental factors such as cold water , valsalva maneuver , hyperventilation, …
Pharmacotherapy of Vasospastic Angina :
A. Calcium channel blockers
- Calcium channel blockers is aimed at blocking the slow calcium currents that are responsible for electrical activation and contraction of smooth muscle cells.
- Calcium channel blockers (CCB) are highly effective for suppression of vasospastic angina (VSA) attacks and actually they are recommended as a first-line treatment in newly diagnosed VSA , preferentially to be given at night because VSA is known to exhibit circadian variation with an early morning peak ( 17).
- Several studies have compared the effectiveness of CCBs (both dihydropyridine and non-dihydropyridine) in reducing angina frequency . Either dihydropyridine or non-dihydropyridine CCBs can be proposed, depending on patient characteristics and predictable adverse effects. However, according to some trials , the ACS incidence rate was significantly lower in the users of the amlodipine and benidipine . Also others trials has been shown that benidipine has significantly the most beneficial prognostic effects as compared to amlodipine , nifedipine or diltiazem .( 18) .
- The combination of dihydropyridine or non-dihydropyridine CCB can be used in severe case.
- High-dose calcium channel blockers possess the most evidence , with respect to decreasing angina incidence , frequency and duration ( up to 20 mg of amlodipide , 420 mg of diltiazem and 100 mg of nifedepine …) ( 19).
B.Nitrates
- Nitrates in addition to calcium channel blockers are the mainstays of medical therapy for vasospastic angina.
- Nitrates have a direct relaxant effect on vascular smooth muscles resulting in the dilation of coronary vessels .
- Several randomized trials comparing the effect of long-acting nitrates alone or in combination with CCBs demonstrated that nitrates are an effective treatment for reducing the frequency of angina in patients with VSA episodes, although their efficacy in reducing MACE is not evident and the need for increasing nitrate doses every time to induce a given antispastic effect owing to nitrate tolerance. ( 20 ) .
- Long-acting nitrates should be proposed in addition to CCBs to prevent vasospastic episodes while short acting nitrates are utilised only during acute episodes
- A recent data demonstrated that the long- term use of nitrate therapy was associated with increased risk of endothelial dysfunction leading to increased risk of adverse cardiac events in VSA patients ( 21 ).
C.Aspirine
- Theorically , the use of low doses of aspirin are known to block thromboxane A2, which is implicated in coronary artery spasm, but the value of traditional low-dose aspirin, especially if not associated with atherosclerotic CAD, may be disputed.. However high-dose aspirin (more than 325mg daily) was reported to exacerbate coronary spasms by blocking the production of prostacyclin, which is a potent endogenous vasodilator ,
- Currently available evidence suggests that low-dose aspirin is not effective in shrinking major adverse cardiovascular events in VA patients, particularly in those with no epicardial CAD ; but in the other hand , lower doses of aspirin may avoid the menace of clinically significant coronary spasms. ( 22 ), ( 23).
D.Statin
- In the absence of obstructive CAD there is conflicting evidence for the clinical benefit of statin therapy in patients with vasospastic angina (VSA) . In a prospective, randomized study, we showed that the addition of fluvastatin at 30 mg/day to conventional medical therapy with calcium‐channel blockers (CCBs) for 6 months significantly reduced acetylcholine (ACh)‐provoked coronary spasm in VSA patients free of coronary organic stenosis ( 24 ).
- And based on more recents trials and meta-analysis , we conclude that statin therapy not only prevents the progression of coronary atherosclerotic plaque formation, but also seems to suppress coronary spasm through improvement of endothelial function and, consequently, reduces the likelihood of cardiovascular events in patients with coronary spasm ( 25), ( 26 ).
E.Nicorandil
- Nicorandil exert anti-spastic properties via activation of nitric oxide (NO) signalling pathways, triggering vascular smooth muscle cell relaxation .In the Guidelines for diagnosis and treatment of Patients with vasospastic angina of the Japanese Circulation Society, both long-acting nitrates and nicorandil are classified as Class IIa agents for the treatment of coronary spasm.
- The usual starting dose of nicorandil is 10 mg twice daily (5 mg for patients susceptible to headache). This dosage can be uptitrated to 20 mg or a maximum of 40 mg twice daily.
- Nicorandil should not be used as monotherapy. It is an add-on therapy for refractory VSA. And we still need more evidence about its efficacy in treating VSA ( 27) ( 28).
F.Alpha 1-adrenergic receptor antagonists
- The rho kinase pathway has an important role in the pathogenesis of coronary spasm and its inhibition has been shown to acutely alleviate severe coronary vasospasm, as well as prevent spasm in patients with vasospastic angina ( 29).
- Given the Paucity of clinical trial on the efficacy and safety of beta-adrenergic receptor antagonists in treating and preventing VSA , the benefit of these drugs remains unclear. However , if well tolerated , alpha1-adrenergic receptor antagonists can be proposed in patients who respond poorly to calcium channel blockers/ nitrates ( 30) ( 31).
- Fasudil is a rho kinase inhibitor that is only available in Japan at present.
Although vasospastic angina usually responds well to treatment with calcium antagonists and/or nitrates , there have been anecdotal case reports of refractory vasospastic angina resistent to intensive treatment with high doses of calcium antagonists and nitrates.
The management of chronic refractory vasospastic angina is largely empirical , with cases reports suggesting the following strategies to be effective :
- high-dose CCBs (verapamil or diltiazem 960 mg/day and/or nifedipine 100 mg/day)
- higher tolerated dose of long acting nitrate
- Nicorandil
- antiadrenergic drugs, including guanethidine and clonidine ( 32)
- fasudil
- corticosteroid ( 33)
When coronary spasm persist despite optimal medical treatment , a invasive approach may represent an alternative treatment :
- selective PCI
- left stellate ganglion blockade ( sympathectomy)
- coronary artery bypass grafting with cardiac denervation
- ICD implantation
Information on late clinical outcome after stenting is limited , some small trials found an icreased risk of restenosis following angioplasty while others trials demontrasted similar results to those without a propensity to spasm . Nevertheless , a more randomized trials should be done before coronary stenting can be recommended for drug refractory CAS. ( 34)
Coronary artery bypass grafting (CABG) has been used in the past but with unfavorable outcomes ( very high incidence of graft failure via competitive flow from the native artery).
The use of an implantable cardioverter defibrillator with aggressive medical treatment has been reported to be effective in CAS patients who are survivors of cardiac arrest as secondary prevention ( 35) while to date , there is no recommendations for ICD implantation as primary prevention.
Sympathetic denervation remains a promising therapeutic approach for severe refractory CAS . Only few cases with dramatic good outcome are reported in litareture ( 36).
Conclusion
In general, patients with coronary spastic angina have a good prognosis , however multiple coronary artery spasms might cause more significant myocardial ischemia and lethal arrhythmia as compared to single coronary artery spasm and should always be treated with the utmost caution (37). Thus , there is an unmet need for further research to help better define the molecular pathways responsible and develop more effective treatments for CAS (38).
Our case highlights the importance of identifying possible coronary artery spasm in daily clinical practice by administration of adequate doses of intracoronary nitroglycerin during coronary procedure in order to avoid inappropriate coronary intervention .
Conflict of interest
None declared.
Case presentation
- Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. 1959;27:375–388. [PubMed] [Google Scholar].
- Park SH,Choi BG,Rha SW,Kang TS, The multi-vessel and diffuse coronary spasm is a risk factor for persistent angina in patients received anti-angina medication. Medicine. 2018 Nov; [PubMed] [Google Scholar].
- Beltrame et al., “The who, what, why, when, how and where of vasospastic angina,” Circulation Journal, vol. 80, no. 2, pp. 288–311, 2016. [PubMed] [Google Scholar].
- Hillis LD, Braunwald E. Coronary-artery spasm. N Engl J Med. 1978;299:695–702. [PubMed] [Google Scholar]
- Yasue H, Kugiyama K. Coronary spasm: clinical features and pathogenesis. Intern Med. 1997;36:760–765. [PubMed] [Google Scholar]
- Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation. 2011;124:1774–1782. [PubMed] [Google Scholar]
- Hung MJ, Cheng CW, Yang NI, Hung MY, Cherng WJ. Coronary vasospasm-induced acute coronary syndrome complicated by life-threatening cardiac arrhythmias in patients without hemodynamically significant coronary artery disease. Int J Cardiol. 2007;117:37–44. [PubMed] [Google Scholar]
- Hazlyna Kamaruddin Julian Gunn Coronary artery spasm: mimicry, misdiagnosis and misfortune http://dx.doi.org/10.1136/bcr-2014-204519 BMJ journal [PubMed] [Google Scholar]
- Slavich and R. S. Patel, “Coronary artery spasm: current knowledge and residual uncertainties,” IJC Heart & Vasculature, vol. 10, pp. 47–53, 2016.View at: Publisher Site | Google Scholar
- Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51:2–17. [PubMed] [Google Scholar]
- Hung MY, Hsu KH, Hung MJ. et al. Interaction between cigarette smoking and high-sensitivity C-reactive protein in the development of coronary vasospasm in patients without hemodynamically significant coronary artery disease. Am J Med Sci. 2009;338:440–446. [PubMed] [Google Scholar]
- Sugiishi M, Takatsu F. Cigarette smoking is a major risk factor for coronary spasm. Circulation. 1993;87:76–79. [PubMed] [Google Scholar]
- Puja K. Mehta, Aneesha Thobani, and Viola Vaccarino, . Coronary Artery Spasm, Coronary Reactivity and Their Psychological PMC 2019 [PubMed] [Google Scholar]
- Fernandez D, Rosenthal JE, Cohen LS, Hammond G, Wolfson S. Alcohol-induced Prinzmetal variant angina. Am J Cardiol. 1973;32:238–239. [PubMed] [Google Scholar].
- Pijls N.H.J. · van der Werf T. Prinzmetal’s Angina Associated with Alcohol Withdrawal. Cardiology 1988;75:226–229 https://doi.org/10.1159/000174376[PubMed] [Google Scholar].
- Pitts WR, Lange RA, Cigarroa JE, Hillis LD. Cocaine-induced myocardial ischemia and infarction: pathophysiology, recognition, and management. Prog Cardiovasc Dis. 1997;40:65–76. [PubMed] [Google Scholar]
- Waters DD, Miller DD, Bouchard A, Bosch X, Theroux P. Circadian variation in variant angina. Am J Cardiol. 1984;54:61–64. [PubMed] [Google Scholar]
- Kazuhiko Nishigaki, Yukiko Inoue; Yoshio Yamanouchi, Hidenori Urata, Hiroaki Shimokawa, Shinya Minatoguchi .Prognostic effects of calcium channel blockers in patients with vasospastic angina--a meta-analysis .Circulation journal , volume 74-2010 [PubMed] [Google Scholar]
- Eun Kim1, Sang-Ho Jo2 , Seung Hwan Han3, Kwan Yong Lee4, Sung Ho Her.Comparison of calcium-channel blockers for long-term clinical outcomes in patients with vasospastic angina Korean J Intern Med. 2021 Jan; 36(1): 124–134. [PubMed] [Google Scholar]
- Takahashi, T. Nihei, Y. Takagi et al., “Prognostic impact of chronic nitrate therapy in patients with vasospastic angina: multicentre registry study of the Japanese coronary spasm association,” European Heart Journal, vol. 36, no. 4, pp. 228–237, 2015[PubMed] [Google Scholar]
- Daiher and T. Munzel, “Organic nitrate therapy, nitrate tolerance, and nitrate-induced endothelial dysfunction: emphasis on redox biology and oxidative stress,” Antioxidants & Redoxx Signaling, vol. 23, pp. 899–942, 2015. [PubMed] [Google Scholar]
- A Young Lim , Seung-Hyuk Choi Clinical implications of low-dose aspirin on vasospastic angina patients without significant coronary artery stenosis; a propensity score-matched analysis international journal of cardiology, 2016[PubMed] [Google Scholar]
- Ji YoungPark Seung Kanhaiya . Impact of low-dose aspirin on coronary artery spasm as assessed by intracoronary acetylcholine provocation test in Korean patients Journal of Cardiology 2012 [PubMed] [Google Scholar].
- Yasue H, Mizuno Y, Harada E, Itoh T, Nakagawa H, Nakayama M, Ogawa H, Tayama S, Honda T, Hokimoto S, Ohshima S, Hokamura Y, Kugiyama K, Horie M, Yoshimura M, Harada M, Uemura S, Saito Y. Effects of a 3‐hydroxy‐3‐methylglutaryl coenzyme A reductase inhibitor, fluvastatin, on coronary spasm after withdrawal of calcium‐channel blockers. J Am Coll Cardiol. 2008;51:1742–1748. [PubMed] [Google Scholar]
- H. Piao, M. H. Jeong, Y. Li et al., “Benefit of statin therapy in patients with coronary spasm-induced acute myocardial infarction,” Journal of Cardiology, vol. 68, no. 1, pp. 7–12, 2016. . [PubMed] [Google Scholar]
- Ishii, K. Kaikita, K. Sato et al., “Impact of statin therapy on clinical outcome in patients with coronary spasm,” Journal of the American Heart Association, vol. 5, p. e003426, 2016. . [PubMed] [Google Scholar]
- C. Kaski, “Management of vasospastic angina?Role of nicorandil,” Cardiovascular Drugs and Therapy, vol. 9, no. S2, pp. 221–227, 1995. [PubMed] [Google Scholar]
- Jason M. Tarkin & Juan Carlos Kaski Vasodilator Therapy: Nitrates and Nicorandil Cardiovascular Drugs and Therapy volume 30, pages367–378 (2016) [PubMed] [Google Scholar]
- Hung MJ, Cherng WJ, Hung MY. et al. Increased leukocyte Rho-associated coiled-coil containing protein kinase activity predicts the presence and severity of coronary vasospastic angina. Atherosclerosis. 2012;221:521–526. [PMC free article] [PubMed] [Google Scholar]
- Masumoto A, Mohri M, Shimokawa H, Urakami L, Usui M, Takeshita A. Suppression of coronary artery spasm by the Rho-kinase inhibitor fasudil in patients with vasospastic angina. Circulation. 2002;105:1545–1547. [PubMed] [Google Scholar]
- R Jay Widmer Lilach O Lerman Amir Lerman The Rho(ad)-kinase for individualized treatment of vasospastic angina European Heart Journal, Volume 39, Issue 11, 14 March 2018 [PubMed] [Google Scholar]
- Frenneaux M, Kaski JC, Brown M, Maseri A. Refractory variant angina relieved by guanethidine and clonidine. Am J Cardiol 1988; [PubMed] [Google Scholar]
- Takagi S, Goto Y, Hirose E, Terashima M, Sakuragi S, Suzuki S, et al. Successful treatment of refractory vasospastic angina with corticosteroids: Coronary arterial hyperactivity caused by local inflammation? Circ J 2004; 68: 17–22; [PubMed] [Google Scholar].
- Tsung O Cheng Percutaneous coronary intervention for variant angina: balloon vs. Stent. Catheterization and cardiovascular interventions 2020[PubMed] [Google Scholar].
- Sueda and H. Kohno, “Optimal medications and appropriate implantable cardioverter-defibrillator shocks in aborted sudden cardiac death due to coronary spasm,” Internal Medicine, vol. 57, no. 10, pp. 1361–1369, 2018[PubMed] [Google Scholar].
- Abbate A, Hamza M, Cassano AD, Melchior R, Roberts C, Grizzard J, et al. Sympathectomy as a treatment for refractory coronary artery spasm. Int J Cardiol 2012
- Walling A, Waters DD, Miller DD, Roy D, Pelletier GB, Théroux P. Long-term prognosis of patients with variant angina. Circulation. 1987;76:990–997. [PubMed] [Google Scholar]
- Miwa K, Fujita M, Sasayama S. Recent insights into the mechanisms, predisposing factors, and racial differences of coronary vasospasm. Heart Vessels. 2005;20:1–7. [PubMed] [Google Scholar].

