Short Communication - Volume 3 - Issue 2
Gender Disparity in the Management of Diabetes Among Residents of Sabon Gari Local Government Area of Kaduna State, Nigeria
Ibrahim Oladayo M1*; Yusuf T1; Rasheed Y2; Sunday Abraham M3
1Department of Human Physiology, Ahmadu Bello University, Zaria, Nigeria.
2Department of Chemical Pathology, Ahmadu Bello University Teaching Hospital, Zaria, Nigeria
3Department of Human Anatomy, Ahmadu Bello University, Zaria, Nigeria.
Received Date : Feb 20, 2023
Accepted Date : Mar 24, 2023
Published Date: Mar 31, 2023
Copyright:© Ibrahim Oladayo M 2023
*Corresponding Author : Ibrahim Oladayo M, Department of Human Physiology, Ahmadu Bello University, Zaria, Nigeria.
Email: musava@ymail.com
DOI: Doi.org/10.55920/2771-019X/1407
Abstract
Gender has been shown to play a major role in the level of management of diabetes mellitus (DM) especially in this part of the world. This study therefore looked into the possibility and level of difference in the management of the condition among patients resident in Sabon Gari Local Government Area (LGA) of Kaduna State, Nigeria. The number of diabetic patients recruited for the study was 250 (aged 35 and above), comprising of 135 and 115 female and male patients respectively. A total of 5mL of blood was taken from the subjects after 10 hour fasting, out of which 3mL was centrifuged and the separated serum analysed for glucose. The remaining 2mL was analysed immediately for glycated haemoglobin (HbA1C). Samples were collected over a period of eight months after which comparison of parameters between both genders was done in order to determine extent of diabetes management. There was a significant difference between the parameters of the female diabetic patients (Mean Fasting Blood Glucose, FBG = 189±82.30mg/dL; Mean HbA1C = 8.5±3.18%) and those of the male diabetic patients (FBG = 223±89.00mg/dL; Mean HbA1C = 9.8±3.39%). The glycaemic markers were significantly lower (though still within the diabetic range) among the female patients as compared with the male patients. Conclusively, the female patients had their diabetes better managed and controlled than their male counterparts
Introduction
Diabetes mellitus (DM) is a worldwide problem that plagues the modern day society. The prevalence of DM is on the increase in many countries of the world, including Nigeria where about 6% of the entire population (12 million people) live with the condition (Uloko et al., 2018). Several hospitals across Nigeria provide treatment and management regimen for diabetic patients (Okoronkwo et al., 2016). However there is evidence of the possibility of gender-dependent disparity in the level of management of the condition (Sacks et al., 2017). Furthermore, Kotila et al., 2018 suggested the possibility of different causes of gender disparities in the management of diabetes and concluded that there is need to further study the gender disparities in the epidemiology of Type 2 DM. Skipping medication in effort to prevent hypoglycaemia, which is said to occur more in men (Huang et al., 2021), has been pointed out to play a major role in under-management of diabetes (Onyenekwe et al., 2019). This study was therefore set up to investigate these claims and determine which gender has DM undermanaged, and requiring more attention among diabetic patients in Sabon Gari LGA of Kaduna State, Nigeria, and a probable reason why it is so.
METHODS
Study Site Sabon gari LGA of Kaduna State, Nigeria is located between latitudes 11o 06’ and 60o 00’ North of the Equator and longitudes 7o 43’ and 59o 00’ East of the Greenwich Meridian. The major city located in this LGA is Zaria (Department of Geology, Sabon-Gari, Kaduna, Nigeria, 2022). The population of Sabon Gari LGA is 393,300 (National Population Commission, 2016).
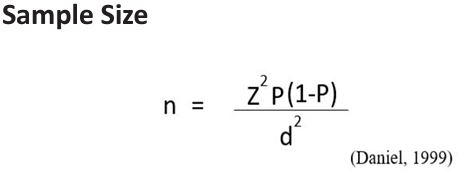
Where: n = Sample size, Z = Z statistic for a level of confidence (for the level of confidence of 99%, Z’s value is 2.59), P = Expected prevalence or proportion (expressed in proportion of 1 instead of percentage), d = Precision (expressed in proportion of 1 instead of percentage).
Choosing a prevalence of 10% (Edo and Akhuemokhan, 2012) at 99% confidence interval, the expected prevalence P = 10% (or 0.1) and Precision = 5% (or 0.05), (Naing et al., 2006). Substituting for the values in the equation, at least 241 subjects should be used. Two hundred and fifty (250) subjects were eventually used for the study comprising of 135 female and 115 male diabetic patients.
Informed Consent and Ethical Approval
The study was approved by the Ethical Committee on Human Research of Ahmadu Bello University, Zaria with the Approval No: ABUCUHSR/2017/002. Informed consent was also obtained from individual participant.
Data Collection and Analysis
Information (age, personal, lifestyle and medical history) about each subject was collected via questionnaire, and a similarity between all subjects was established. Blood samples were collected from subjects after 10 hours of fasting. 5mL of blood sample (each) was collected via venepuncture. Where 3ml of the blood was transferred from syringe into plain bottles, and
Table 1: Comparing the mean values of glycated haemoglobin (HbA1c) between both genders
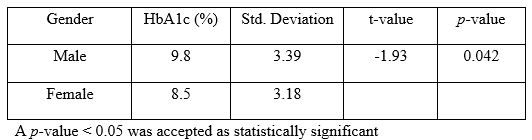
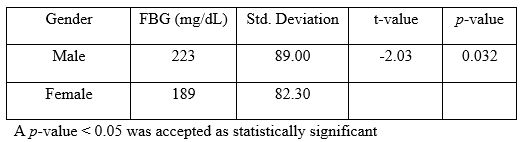
Table 2: Comparing the mean values of Fasting Blood Glucose (FBG) between both genders
centrifuged at 4000 rpm for 10 min. The serum was then analysed for FBG. The remaining 2ml was transferred into EDTA bottles and analysed for glycated haemoglobin (HbA1C) using the colorimetric analysis method. Results were presented as mean ± SD and data was analysed using independent student's T-test. SPSS version 24 was the software used.
Results
The mean values of HbA1c and fasting blood glucose (FBG) was compared between both genders (Tables 1 and 2 respectively). It can be observed that the mean HbA1c for the male patients (9.8±3.39%) was significantly higher than the mean HbA1c for the female patients (8.5±3.18%) as seen in Table 1, with a p-value of 0.042. Similarly, the mean FBG for the male patients (223±89.00mg/dL) was significantly higher than the mean FBG for the female patients (189±82.30mg/dL) as seen in Table 2, with a p-value of 0.032. It is also noted that the standard deviation within each gender is similar and not too different from the other gender.
Discussion
After ascertaining a similarity in the age-range and socioeconomic livelihood of all subjects, it was observed that a diabetic patient that is a woman is likely to have her condition better managed than a diabetic patient that is a man. Schroeder et al., 2014 suggested that observed gender differences in the management of diabetes might be due to varying strictness in the usage of diabetes medication among the two gender groups. In contrast, uniformity in lifestyle of both genders in this study rules out the possibility of forgetfulness in using medication by a gender due to being “too busy”. However, in a study by Heald et al., 2017, corroborated by Kawamoto et al., 2017 in another study, it was found that the use of diabetic medication is negatively associated with HbA1c in men but positively associated with HbA1c in women which might account for the significantly higher HbA1c observed among male diabetic patients in this study. However, the blood glucose of the male diabetic patients was also significantly higher suggesting that other factor(s) such as irregularity in clinic attendance might be responsible for the relatively poorly-managed diabetes observed among the male patients other than negative association of medication with HbA1c. Physical activity, sickle cell trait and other haemoglobin variants are also factors that have been identified as responsible for the gender differences in diabetes management (Navarro-Peternella et al., 2016; Editorial, 2017). Innovations in increasing diabetes knowledge and health behaviour change have generally been recommended for patients (Siddique et al., 2017) and especially for female patients. Even though it is the male diabetic patients that have their diabetes more poorly managed in this study, the recommendation by Siddique et al., 2017 can assist in bridging the observed gender disparity in diabetes management. Tella et al., 2021 also concluded in their review that diabetes self-management education can serve as a means to address the needs of diabetic patients in Nigeria. This is in concomitance with the findings of this study that suggests that the poor management of diabetes among male patients could be to inadequate knowledge about diabetes management or sheer nonchalance in attending clinic or in caring for themselves.
Conclusion
This study further confirms the existence of gender disparity in the management of diabetes in Nigeria or some part of Nigeria and recommends some steps that can be taken in checking these disparities.
Case presentation
- Daniel WW. Biostatistics: a foundation for analysis in the health sciences. Seventh ed. New York, USA: John Wiley & Sons; 1999.
- Department of Geology, Sabon-Gari, Kaduna, Nigeria, 2022. www.findlatitudeandlongitude.com.
- Editorial (2017): Sex disparities in diabetes: Bridging the gap. Lancet Diabetes Endocrinology, 5:839.
- Edo AE and Akhuemokhan K. (2012). Relationships between hemoglobin A1c and spot glucose measurements in Nigerians with type 2 diabetes mellitus. Nigerian Journal of Clinical Practice, 15:23-6.
- Heald AH, Anderson SG, Cortes GJ, Cholokova V, Narajos M, Khan A, et al. (2017). Hypoglycaemia in the over 75s: Understanding the predisposing factors in type 2 diabetes (T2DM). Primary Care Diabetes, 17:30123-7.
- Huang, S.H., Huang, P.J., Li, J.Y., Su, Y.D., Lu, C.C. and Shih, C.L. (2021). Hemoglobin A1c Levels Associated with Age and Gender in Taiwanese Adults without Prior Diagnosis with Diabetes. International Journal of Environmental Research and Public Health, 18:3390.
- Kawamoto R, Ninomiya D, Kasai Y, Senzaki K, Kusunoki T, Ohtsuka N, et al. (2017). Interaction between gender and uric acid on haemoglobin A1c in community dwelling persons. Journal of Endocrinology Investigation, 41(4):421-429.
- Kotila, T., Charles-Davies, M.A., Afolabi, R. and Adeleye, J. (2018). The Effect of Age, Gender and Haemoglobin Variants on Glycated Haemoglobin. International
- Naing L, Winn T, and Rusli BN. (2006). Practical issues in calculating the sample size for prevalence studies. Archives of Orofacial Sciences, 1:9-14.
- National Population Commission, 2016. www.citypopulation.de.
- Navarro-Peternella FM, Torquato Lopes AP, Oliveria de Arruda G, Teston EF and Marcon SS. (2016). Differences between genders in relation to factors associated with risk of diabetic foot in elderly persons: A crosssectional trial. Journal of Clinical and Translational Endocrinology, 6:30-6.
- Okoronkwo IL, Ekpemiro JN, Onwujekwe OE, Nwaneri AC, Iheanacho PN. (2016). Socioeconomic inequities and payment coping mechanisms used in the treatment of type 2 diabetes mellitus in Nigeria. Nigerian Journal of Clinical Practice, 19(1):104-9.
- Onyenekwe, B.M., Ekenechukwu, E.Y., Chidinma, B.N., Christian, I.O., Chidiebere, V.U. and Kingsley, O.O. (2019). Diabetes Mellitus in adult Nigerians: patients’ characteristics, laboratory profile, practices and management outcome. Intenational Journal of Research in Medical Sciences, 7(10):3844-3853.
- Sacks DB, Bebu I, Lachin JM. (2017). Refining measurements of Haemoglobin A1c. Clinical Chemistry, 63:1433-5.
- Schroeder EB, Bayliss EA, Daugherty SL, Steiner JF. (2014). Gender differences in incident diabetes. Women Health Issues.; 24:e61-8.
- Siddique, K.B., Islam, M.S., Banik, P.S. and Rawal, L.B. (2017). Diabetes knowledge and utilization of healthcare services among patients with type 2 diabetes mellitus in Dhaka, Bangladesh. BMC Health Services Research, 17:586
- Tella EE, Yunusa I, Hassan JH, Chindo IA, Oti VB (2021) Prevalence, Contributing Factors and Management Strategies (Self-Management Education) of Type 2 Diabetes Patients in Nigeria: A Review. International Journal of Diabetes and Clinical Research, 8:148.
- Uloko AE, Musa BM, Ramalan MA, Gezawa ID, Puepet FH, Uloko AT, et al. (2018). Prevalence and risk factors for diabetes mellitus in Nigeria: a systematic review and meta-analysis. Diabetes Therapy, 9(3):1307–16.

