Case report - Volume 3 - Issue 2
Thromboembolism: An unusual way of tissue diagnosis of Squamous Cell Carcinoma of Lungs
Areeba S1; Sardar Hassan I2*; Abdur Raheem Ch3; Samid F4
1Faisalabad Medical University, Faisalabad, Pakistan.
2Department of Cardiovascular Diseases, Lahey Hospital, Burlington, MA.
3Geriatric Medicine, University of Texas Medical Branch, Galveston, TX.
4Department of Pulmonology, University of Oklahoma Health Sciences Center.
Received Date : Feb 21, 2023
Accepted Date : April 03, 2023
Published Date: Mar 27, 2023
Copyright:© Sardar Hassan I 2023
*Corresponding Author : Sardar Hassan I ,Department of Cardiovascular Diseases, Lahey Hospital, Burlington, MA.
Email: sardarhassanijaz@yahoo.com
DOI: Doi.org/10.55920/2771-019X/1408
Abstract
Lung carcinoma presents in multifarious ways from incidental imaging finding to respiratory or systemic symptoms secondary to local invasion or metastasis. We report an atypical presentation of lung cancer.
A 69-year-old male presented with sudden onset bilateral lower extremity weakness. He had cold bilateral lower extremity with no palpable pulses or Doppler signals in the lower extremity. A computed tomographic angiographic (CTA) scan revealed large thrombus in the infra-renal aorta and bilateral common iliac arteries with total occlusion. Bilateral endovascular thrombectomy along with fasciotomy was done. Immuno-histochemical staining of thrombectomy mass showed metastatic squamous cell carcinoma. Positron emission tomography (PET) scan revealed hypermetabolic right pulmonary hilar foci with hypermetabolic mediastinal nodes. Diagnosis of non-small cell lung carcinoma was made and subsequently, chemotherapy was started.
Atypical presentation and tissue diagnosis of lung cancer via histopathological examination from endovascular thrombectomy are quite unique. Our case highlights the importance of analysis of thrombectomy mass.
Keywords: lung carcinoma, thromboembolic disease, atypical presentation
BACKGROUND
Lung carcinoma is the leading cause of mortality secondary to malignancy in both genders. [1] The presentation of lung carcinoma varies from being asymptomatic, detected incidentally on imaging to overt respiratory symptoms secondary to local invasion by tumor mass or related to metastasic invasion or systemic findings. [2] Usually the tissue diagnosis is obtained by biopsy of the primary lesion or the accessible metastatic site. [1,2] However, we report a unique case of de novo diagnosis of squamous cell carcinoma of lung in a patient presenting with sudden onset bilateral acute limb weakness secondary to thromboembolism. Later after endovascular thrombectomy of abdominal aortic clot, pathology and immunohistochemical analysis of embolus established the diagnosis of carcinoma.
CASE PRESENTATION
A 69-year-old male with history of hypertension, diabetes mellitus type 2 and former smoker (quit 1 year ago, ~60 pack years history) presented with sudden onset bilateral lower extremity weakness and numbness. The symptoms started with difficulty in defecation, followed by dull cramping pain in the legs. The pain was sudden in onset, progressively worsening in intensity and associated with ascending numbness in lower limbs bilaterally. On physical examination, he had bilateral cold feet with profound loss of motor power and sensations. There were no palpable peripheral pulses in the lower extremity along with no doppler signals.
INVESTIGATIONS
An urgent computed tomographic angiographic (CTA) – (Figure 1) scan was done showing large thrombus in the infra-renal aorta and bilateral common iliac arteries with total occlusion. Emergent bilateral endovascular thrombectomy along with fasciotomy was performed. Postoperatively the motor and sensory function recovered, however, he developed rhabdomyolysis with reperfusion. Intravenous fluids were started for
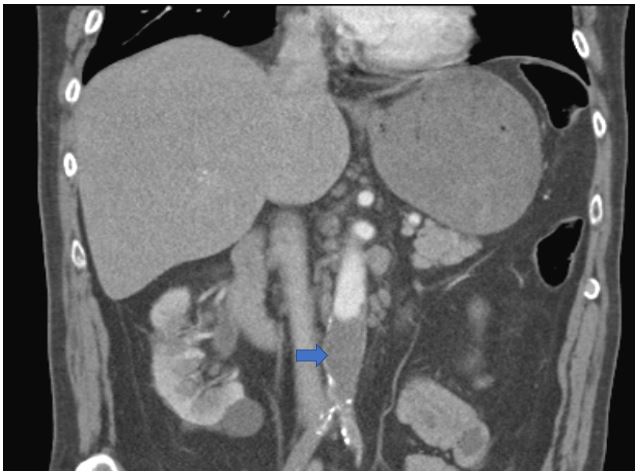
Figure 1: Computerized Tomographic Angiographic (CTA) revealing lower abdominal aorta and bilateral common iliac artery clot (blue arrow indicates the thrombus).
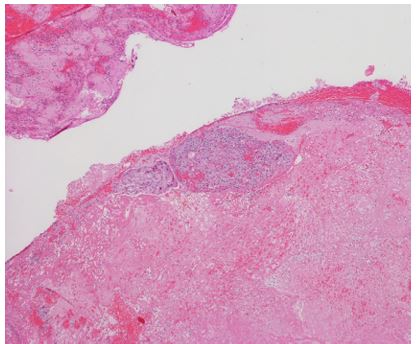
Figure 2 A (4x H&E): shows organized thrombus admixed with squamous cell carcinoma, the round over all shape is compatible with vascular thrombus. (H& E: Hematoxylin and Eosin stained).
optimal diuresis to prevent acute kidney injury. Bilateral doppler scans were negative for deep venous thrombosis. All the coagulation parameters were within normal limits and workup for hypercoagulability was negative. Thoracic echocardiography ruled out any intracardiac thrombus. Post-operatively the ankle brachial index was normal. He was empirically started on the anticoagulants. The CT chest showed right pulmonary hilar mass along with multiple enlarged mediastinal lymph nodes concerning for metastasis and a sub-centimeter right lower lobe pulmonary nodule. The histopathology examination of thrombectomy retrieved thromboembolus revealed organized thrombus admixed with nests of epithelioid cells with cellular pleomorphisms and keratin bridges between cells suggestive of metastatic squamous cell carcinoma (Figure 2 A, B & C). Immuno-histochemical stains revealed tumor cells positive for p40 and cytokeratin 5/6. Napsin, PAX-8 and mucicarmine staining was negative, however, rare cells tested positive for
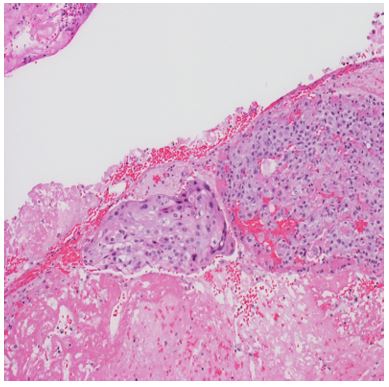
Figure 2 B (10x H&E): Nests of epithelioid cells with cellular pleomorphisms within the clot
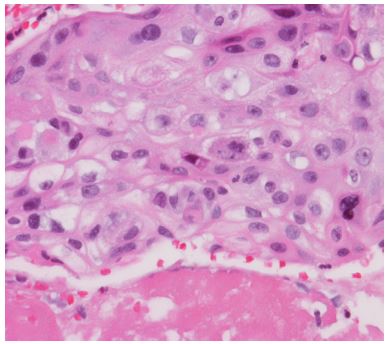
Figure 2 C (10x H&E): Nests of epithelioid cells with cellular pleomorphisms within the clot
thyroid transcription factor -1 (TTF-1) (Figure 3 A & B). Positron emission tomography (PET) scan was done to diagnose occult primary. It showed hypermetabolic right pulmonary hilar foci with standard uptake value (SUV) of 7.0 suspected to be the primary lesion with hypermetabolic mediastinal nodes with SUV of 6.8 concerning for metastasis (Figure 4). Magnetic Resonance Imaging (MRI) brain was concerning for brain metastasis with left thalamic and right lateral ventricle lesions. Diagnosis of non-small cell (squamous) lung carcinoma stage IV was made.
TREATMENT
Patient underwent palliative radiotherapy to brain and was started on chemotherapy regimen with gemcitabine and carboplatin.
OUTCOME AND FOLLOW-UP
He initially tolerated the chemotherapy well for the first cycle. However, during the second cycle, developed adverse reac
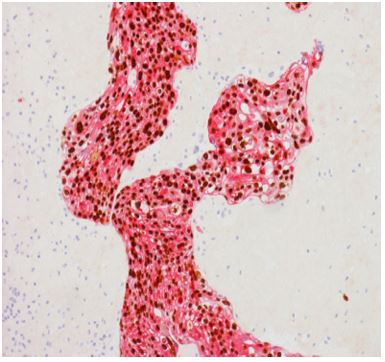
Figure 3A: Immunohistochemistry - p40 and CK5/6: strongly positive. (pink = CK5/6 cytoplasmic stain and brown = p40 nuclear stain).
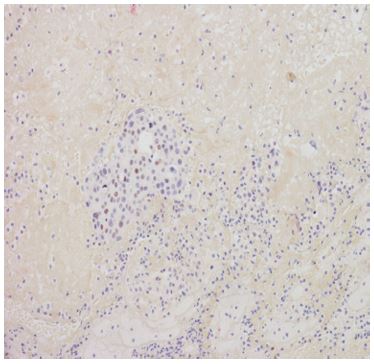
Figure 3B: Immunohistochemistry - TTF-1 and Napsin A: negative. Rare tumor cells are positive for TTF-1. (TTF-1: Thyroid transcription factor -1).
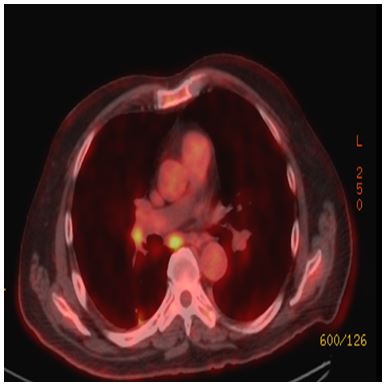
Figure 4: PET Scan with hypermetabolic pulmonary and mediastinal lymph nodes.
tion with worsening stomatitis and intractable vomiting nonresponsive to antiemetics. He was finally hospitalized for neutropenic fever and during the hospital stay decided to opt for comfort care.
Discussion
Lung carcinoma can present in a variety of unusual ways. In elderly chronic smokers, especially male patients with a prolonged history of tobacco abuse the suspicion of lung carcinoma should be high. Therefore, in case of unexplained signs and symptoms, lung malignancy must be kept in differentials. Literature review shows that lung carcinoma can manifest without any overt respiratory and systemic symptoms. For example, there have been case reports of lung carcinoma presenting as: painful subcutaneous nodules of anterior abdominal wall [3]; electrocardiographic changes mimicking as ST segment elevation myocardial infarction without elevation of cardiac enzymes through left atrial involvement [4] ; erectile dysfunction with penile metastasis [5]; knee bursitis through invasion of the bursa [6]; intracranial metastasis involving the soft tissue of the skull [7]; metastasis to soft tissue of the hand [8]; paraneoplastic syndromes with multifarious neurological presentations [9] and soft tissue mass sneezed out.[10]
Acute lower limb weakness is mostly of thromboembolic origin secondary to emboli of cardiac origin or the atherosclerosis of the limb vessels. Rarely acute limb can occur as a complication of abdominal aortic aneurysm or paradoxical emboli of venous origin. Interestingly in our case the sudden onset lower extremity weakness was secondary to a metastatic thromboembolic mass involving abdominal aorta and common iliac arteries. A similar case report with bilateral popliteal artery occlusion with cardiac embolic source secondary to lung carcinoma invasion of the pulmonary vein has been reported. [1] However, in that case the histopathologic examination of the thromboembolic mass did not yield the diagnosis, so median sternotomy was done revealing the tumor mass with cardiac invasion. [1] Interestingly in our case the histopathology of the thrombectomy retrieved mass led to the presumptive lung carcinoma diagnosis without any obvious cardiac emboli. The most plausible explanation in our case was that the pulmonary lesion invaded the pulmonary artery or left atrium and metastasized to lodge into abdominal aorta.
The histopathological exam of the thrombectomy masses can provide important diagnostic information. There have been studies that histopathology of thrombus from endovascular thrombectomy can help in establishing the etiology of cryptogenic stroke. For example, the gram stain of retrieved clot sample yielded the diagnosis of infective endocarditis in a patient with cryptogenic ischemic stroke. [11] Moreover, a retrospective case series of 31 patients, with idiopathic intracranial hemorrhage, showed that examination of thrombus can help establish etiology in some of the cases. [12] Similarly, a retrospective analysis revealed that histopathologic clot examination in serous samples and fine needle aspirates can help improve the diagnostic yield of the sample. The clot samples can test positive for the malignant cells despite the original sample being negative, which adds to the positive predictive value of the test. [13,14]
References
- Fernandez BB, Grove M, Carman TL. An unusual presentation of simultaneous bilateral popliteal artery embolism--a case report. Angiology. 1998;49(7):573-6.
- Tsui P, Lee JH, MacLennan G, Capdeville M. Hemoptysis as an unusual presenting symptom of invasion of a descending thoracic aortic aneurysmal dissection by lung cancer. Tex Heart Inst J. 2002;29(2):136-9.
- Chandanwale SS, Pal SS. Metastatic soft tissue squamous cell carcinoma: unusual presentation of lung cancer. J Cancer Res Ther. 2014;10(1):216-7.
- Guha P, Sardar P, Mookerjee S, Guha S. Left atrial extension of lung carcinoma simulating myocardial infarction, unusual presentation: case report and literature review. Tanaffos. 2011;10(2):69-71.
- Haliloglu AH, Haliloglu N, Akpinar EE, Ataoglu O. Erectile dysfunction: initial symptom of a patient with lung cancer. J Sex Med. 2011;8(12):3511-4.
- Vakili M, Yousefghahari B, Sharbatdaran M. Squamous cell carcinoma of lung with unusual site of metastasis. Caspian J Intern Med. 2012;3(2):440-2.
- Kader I, Strong M, George M. Skull destruction from intracranial metastasis arising from pulmonary squamous cell carcinoma: a case report. J Med Case Rep. 2013;7:28.
- Walton ZJ, Holmes RE, Chapin RW, Lindsey KG, Leddy LR. Bronchogenic squamous cell carcinoma with soft-tissue metastasis to the hand: an unusual case presentation and review of the literature. Am J Orthop (Belle Mead NJ). 2014;43(12):E324-7.
- Verma R, Lalla R, Patil TB, Babu S. "Person in the barrel" syndrome: Unusual heralding presentation of squamous cell carcinoma of the lung. Ann Indian Acad Neurol. 2016;19(1):152-5.
- Hornick PI, Taylor IB, Glover GW, Townsend ER. "Sneeze of a cancer from the lung": sternumentum carcinomae pulmonariae. Ann Thorac Surg. 1997;63(4):1174-5.
- Bhaskar S, Cordato D, Cappelen-Smith C, Cheung A, Ledingham D, Celermajer D, et al. Clarion call for histopathological clot analysis in "cryptogenic" ischemic stroke: implications for diagnosis and treatment. Ann Clin Transl Neurol. 2017;4(12):926-30.
- Abrahams NA, Prayson RA. The role of histopathologic examination of intracranial blood clots removed for hemorrhage of unknown etiology: a clinical pathologic analysis of 31 cases. Ann Diagn Pathol. 2000;4(6):361-6.
- Addey A, Rachel J, Codling BW, Poller DN. Histological examination of clots from cytological specimens: is this a worthwhile procedure? Cytopathology. 1996;7(2):120-4.
- Jalal R, Aftab K, Hasan SH, Pervez S. Diagnostic value of clot examination for malignant cells in serous effusions. Cytopathology. 2009;20(4):231-4.

