Review Article - Volume 3 - Issue 2
Acute brain Injury/acute lung injury as life-threatening organ Dysfunction and with outcomes due to sepsis
Dao-Ming T,1*; Guang-Sheng W1; Shao- Dan W2; Yuan-Wei W1; Ying W1
1Department of Neurology, Affiliated Shuyang Hospital of Xuzhou Medical University, Jiangsu, China
2Department of Intensive Care Medicine, Affiliated Shuyang Hospital of Xuzhou Medical University, Jiansu, China.
Received Date : Feb 23, 2023
Accepted Date : Mar 28, 2023
Published Date: April 04, 2023
Copyright:© Dao-Ming T 2023
*Corresponding Author : Dao-Ming T, Department of Neurology, Affiliated Shuyang Hospital of Xuzhou Medical University, Jiangsu, China.
Email: dmtong@xzhmu.edu.cn
DOI: Doi.org/10.55920/2771-019X/1409
Abstract
Background: The early diagnosis of sepsis requires a rapidly screening life-threatening organ dysfunction caused by infection. Sepsis related life-threatening ABI and ALI have not been reported. Objective: To investigate ABI and ALI whether is the leading life-threatening organ dysfunction and its prognosis in sepsis.
Methods: A retrospective study from January 1, 2018 to January 1, 2021 was performed in a general ICU. Those critical ill adult patients who were undergone a brain+ chest + abdominal CT screening before arriving at the ICU were included in this study. Primary outcome was to determine the prevalence of both acute brain and lung injuries and to investigate the hazards of both brain and lung injuries with worse survival in sepsis. The second outcome was the Glasgow Outcome ScaleExtended (GOSE) score at the first 30 days in ICU. Results: Of 1178 ICU admissions, 376 (31.9%) critically ill adults with sepsis were identified by a brain + chest + abdominal CT screening before on ICU. The median age was 66.7 years (IQR 18-91 years) and 246 (65.4%) patients were males. The median time from onset to CT screening before on ICU was 1hour (IQR, 0.5-229 h). The rapid CT screening before on ICU showed that most patients had either sepsis related ABI (94.7%, 356/376) or ALI (93.4%, 351/376), and 335 (89.1%) of 376 patients had evidence of both ABI and ALI due to infection/sepsis. 359 (95.5%) of 376 patients were invasively mechanical ventilated on the day of ICU admission. The risk factors for sepsis with worse outcomes were presentation with both ABI and ALI (OR, 3.8; 95% CI, 2.019- 7.108), systemic inflammatory storm (SIRS≥2, OR, 2.7; 95% CI, 0.999- 7.191), and shorter length of stay in ICU (OR, 0.9; 95% CI, 0.837-0.958). Predictors of 30-day mortality were both ABI and ALI (RR, 2.5. 95% CI, 1.553-2.799), requiring mechanical ventilation ( RR,0.05. 95% CI, 0.005-0.459), and elevated procalcitonin (RR,1.0. 95% CI, 1.001 -1.010). During the 24 days in the ICU, the dynamic profile of inflammatory mediators and organ injury in sepsis with nonsurvivors were significantly higher than those survivors(all p<0.05). A worse outcome (59.4% dead) of sepsis with ABI and ALI at 30 day follow-up was also assessed by GOSE ( Glasgow Outcome Scale-Extended ) scores, and most of them died in the ICU.
Conclusions: This study highlights a previously unreported that the life-threatening ABI / ALI and potential poor outcomes were identified by brain + chest + abdominal CT scans before on ICU. A recognition of this issue facilitate for sepsis patients timely care to improve outcome.
Key words : Sepsis; Coma; Acute brain injury; Acute lung injury; Systemic inflammatory storm syndrome; Organ failure, Mortality.
Introduction
Sepsis related acute brain injury(ABI) and acute lung injury(ALI) is the life-threatening organ dysfunction following critical illness.1-3 The ascending reticulum activation system (ARAS) is located in the bilateral thalamus and midbrain , as a wake-up "switch"(Fig. 1, A and B) , which is very sensitive to ischemia and hypoxia, if simultaneous closed in bilateral will lead to ABL/acute coma. Sepsis related ABI and ALI affects up to the wake-up "switch" of critically ill patients, are strongly associated with worse outcomes and high mortality in critical illness.4-6 Despite the SIRS criteria is still used as a tool to screening infection and inflammatory storm for acute critical ill, 6,7 but it only used to screening suspected infection in the ICU admissions. However, how to rapid screening sepsis related life-threatening ABI and ALI, which is still unrecognized. We hypothesized that the critical ill adults in ICU would be having a high prevalence of infection-induced life-threatening ABI and ALI, which may be identified by a rapid brain + chest + abdominal CT screening before on ICU. The aim of this study was to investigate the sepsis related life-threatening ABI and ALI in critical ill adult patients, including the clinical features of early CT screening, risk factors with worse outcomes, and laboratory findings. We hope that our study results will verity this hypothesis and provide evidence of CT screening before on ICU for sepsis with ABI and ALI, so that to improve early diagnosis and management, and to reduce the mortality of sepsis.
Methods
Procedures and population
We conducted a retrospective cohort study from the critical ill adult patients with sepsis who were admitted to a general ICU in the Affiliated Shuyang Hospital of Xuzhou Medical University, from Jan 1, 2018, to Jan 1, 2021 with a length of stay of more than 24 hours. During this study period, those critical ill adult patients who were performed a brain + chest + abdominal CT screening before on ICU were included in this study. We excluded those critical ill patients who did not have CT data before on ICU, or no medical records due to either death or automatically out of the ICU due to family asked to give up treatment within the first 24 hours. The study was approved by the ethical committee on clinical research of the Affiliated Shuyang Hospital of Xuzhou Medical University, Because the study involved only a review of records obtained as a part of routine medical care, it did not require written information consent from all patients
Screening sepsis
Despite new guideline recommend ' SIRS criteria for screening suspected infection of critical illness in the ICU admissions, but few tools are available to screen for sepsis related ABI and ALI before on ICU. In recent years, in the emergency center of our hospital, many critical ill adult patients have been performed a brain+ chest + abdominal CT screening before on ICU.
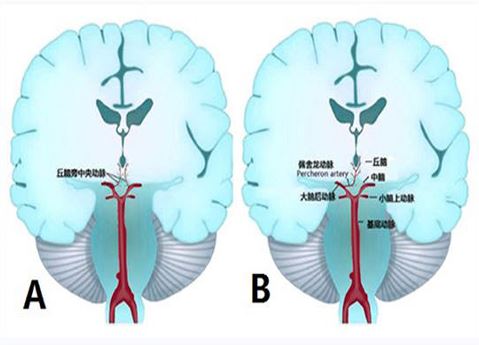
Figure1: The supply blood of a “switch” for the wake-up.
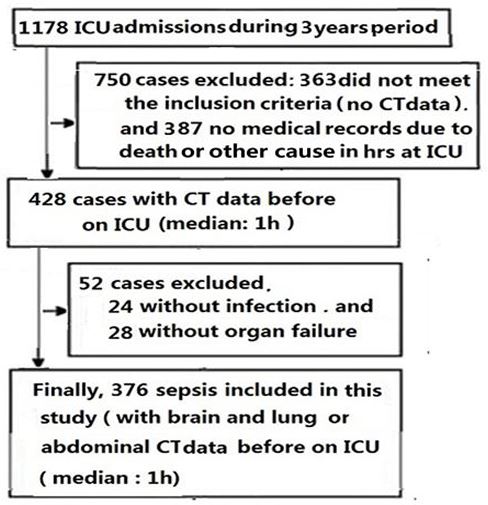
Figure 2: Flow Chart. The patients who were not met the eligibility for this study design were excluded. Finally, 376 patients with sepsis were included in the present study.
In the present study, sepsis related ABI and ALI was based on a large sample of clinical practice in ICU, which was from the electronic medical records of critical ill adult patients who were used a brain+ chest + abdominal CT screening before on ICU. Thus, we studied these patients who had confirmed sepsis related ABI and ALI which identified by CT screening. We defined the features of CT screening for sepsis with ABI as diffuse brain edema or vasogenic brain edema, while sepsis with ALI as infection related pulmonary edema or consolidation, which were showed in the Table 1 in the appendix. We also used the recent update SOFA criteria 7 for sepsis-associated organ dysfunction to verify the CT screening of ABI and ALI before on ICU. The SOFA score ≥2 for the brain may indicate a ABI. Also, the SOFA score ≥2 for the lung may indicate a ALI( in the Table 2 in the appendix).
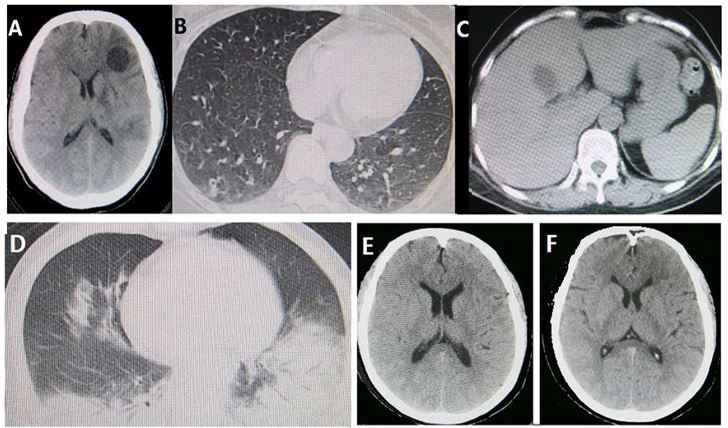
Figure 3: TThe features of brain + chest+abdominal computed tomographic (CT) images. Figure 2 A-C is from a more than 50 yearold female patient with fever 2 days and drowsiness 1day was admitted. Before on admission, brain CT showed the focus of infection and diffuse edema (A), chest CT showed bilateral pneumonia(B), and abdominal CT showed a focus of infection(C). Figure 2 D-F is from a more than 55 year-old female with fever 2 days and coma 2 hours was admitted. Before on admission, chest CT screening showed bilateral pneumonia(D), brain CT showed the brain diffuse swelling (E and F). On ICU, two patient had brain failure and lung failure needing intubation respiratory, suggesting early brain and lung failure from community-required pneumonia.
Table 1: Baseline characteristics of the study population on ICU(n=376).
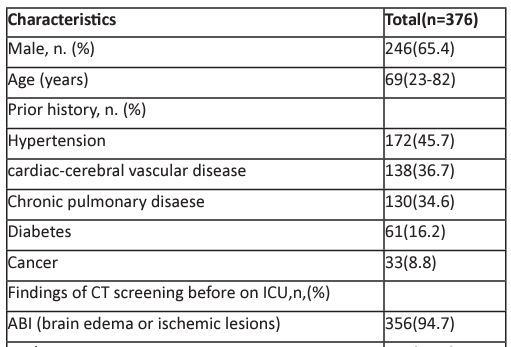
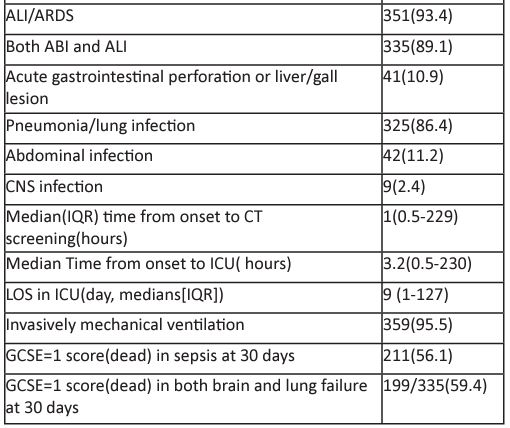
Abbreviation: ICU= intensive care unit; GCS= Glasgow Coma Scale; SOFA= Sequential [sepsis-related] Organ Function Assessment; MODS= multible organ dysfunction;. LOS, length of stay; GCSE= Glasgow Outcome Scale-Extended.
Screening suspected infection:
Systemic inflammatory response syndrome (SIRS) mainly involves to a massive inflammatory cytokine release.8 More recently, it's called a cytokine storm, which is a life-threatening systemic inflammatory storm.9 Moreover, this inflammatory syndrome also involves other inflammatory mediators in the blood (e,g., D-dimer, C-reactive protein, and procalcitonin). The clinical manifestations of SIRS include follow 4 points: (1) temperature> 38o� or < 36o�; (2) heart rate >90 beats per minute; (3) tachypnea> 20 respirations per minute or Pco2 less than 32mmHg ; (4) white blood cell count > 12.0×109/L or < 4.0×109/L, or > 10% band forms. The identified criteria for SIRS must be at least ≥2 points. SIRS only used to screening suspected infection rather than inflammatory mediators. Thus, we also measured the dynamic profile of inflammatory mediators and others laboratory findings during the 24 days in ICU.
Outcomes: Our primary outcome were the high risk factors of both ABI and ALI with worse survival. Our secondary outcomes were the Glasgow Outcome Scale-Extended (GOSE) scores 10 at the initial 30 days in ICU. The outcome events were reviewed by two of the investigators (the first and second author). In order to assessment the GOSE score of patients at the initial 30 days, survival state was confirmed by the medical records. If the patient died after discharge, the information was followed-up to 30 days.
Data collected
All clinical data were gathered from the electronic medical records written by residents or attending physicians of the emergency and ICU. In addition to collect the brain + chest +abdominal CT scans findings, the collected clinical profile for this study in ICU included the patient demographics, time from
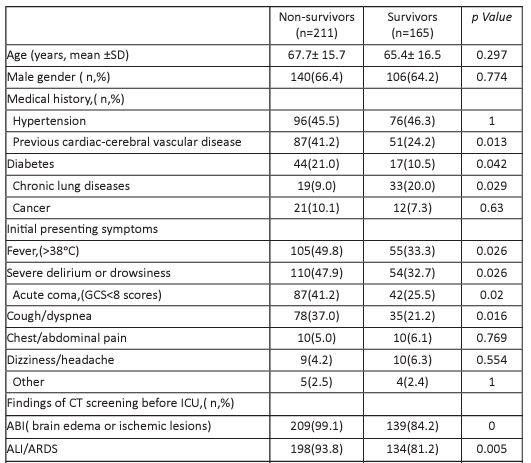
Table 2: Baseline characteristics in patients with sepsis (n=376).
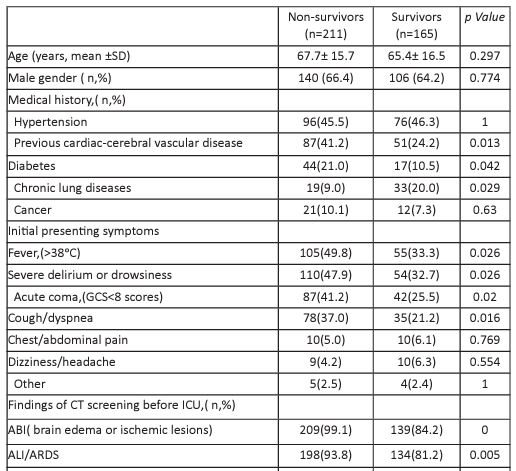
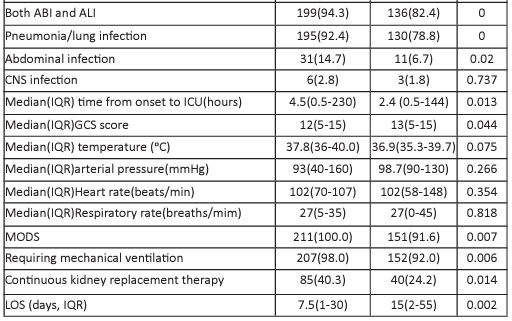
Abbreviations: ICU, intensive care unit; GCS, Glasgow Coma Scale; SOFA, Sequential [sepsis-related] Organ Function Assessment; IMV, invasive mechnical ventilation; LOS, length of stay; IQR;interquartile range; MODS; multiple organ dysfuunction syndrome.
critically ill event to infection, initial SIRS level, initial SOFA score, initial GCS score (or GCS motor score (if the patients were in intubation), vital sign data, experimental / laboratorial data, mechanical ventilation, traditional treatment, length of stay (LOS) in the ICU, and outcomes assessment (GOSE).
Statistical methods
As septic patients were in intubation, we used the GCS motor score (GCS m) to assess acute brain failure , e.g., GCS m<5 indicate a mild/moderate brain failure, GCS m<3 indicate a severe brain failure. The results for each group are expressed as the mean ± standard deviation (SD) or median (IQR), and n (%) indicates qualitative values. Fisher’s exact test and the Mann-Whitney U test were used to examine the relationship between baseline patient variables. Continuous variables were compared using Student’s t test. The area under ROC curve (AUC) were measured by the systemic CT screening for infection/organ failures, and its area of ACU was compared between the systemic CT screening before on ICU and SIRS screening on ICU. Multivariate-adjusted odds ratios (OR) and 95% confidence intervals (CIs) were estimated using a logistic-regression model if they were significant in the univariate analysis, or using Cox proportional hazards model to examine sepsis baseline status and determine whether the variables played a role in the risk of death. Differences between patients was considered significant if the p-value was <0.05. Statistical calculations were performed using a proprietary, computerized statistics package (SPSS 17.0.).
Table 3: Laboratory findings in patients with sepsis who died and survivor (n=376)
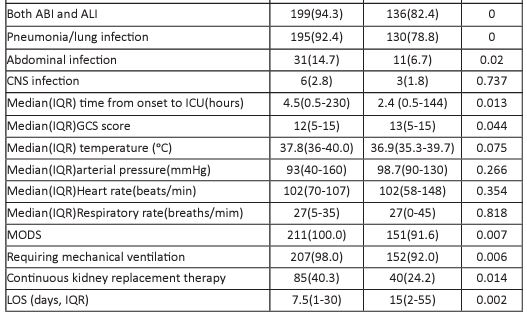
Abbreviations: GCS, Glasgow Coma Scale; SIRS, systemic inflammatory response syndrome; SOFA, Sequential [sepsis-related] Organ Function Assessment; qSOFA, quick SOFA.
Table 4: Logistic regression analysis to identify the death risk factors of sepsis patients in ICU (n=376)
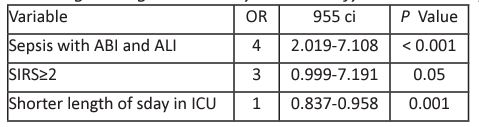
Abbreviations: SIRS, systemic inflammatory response syndrom; ICU, intensive care unit.
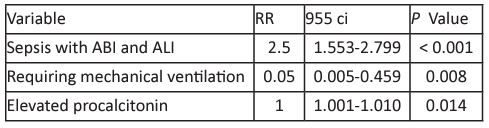
Table 5: The Cox multivariate logistic regression analysis of outcomes for sepsis with worse survival in ICU(n=376)
Results
A total of 1178 critical illness patients were admitted our ICU during the study period. 750 patients were excluded based on our screening criteria, including 363 patients without CT data before on ICU and 387 length of stay less 24 hours or without medical data. Among 428 patients with CT data before on ICU , we excluded those patients without infection (N = 24) and without acute organ failure(n=28). Finally, 376 (31.9%) critically ill adults patients with sepsis were included in the present investigation.(Figure2)
The baseline characteristics of the study population were showed in the Table1. Of 376 sepsis patients, the median age was 66.7 years (IQR 18-91 years) and 246 (65.4%) patients were males. Most patients had chronic diseases. The median time from onset to ICU admission was 3.2 hours (IQR, 0.5230 h). The median time from onset to CT screening before on ICU was 1hour (IQR, 0.5-229 h). By a rapid brain+ chest + abdominal CT screening before on ICU, These patients had various degrees of sepsis related ABI (94.7%,356/376), in most cases were manifested as the sulcus of the brain is shallow( Figure3), severe cases may be manifested as brain displacement. While these patients had also ALI (93.4%,351/376), The rapid CT screening before on ICU showed that most patients (89.1%,335/376) had evidence of both ABI and ALI due to pneumonia (Figure2). The community-acquired pneumonia (86.4%,325/376) was the common infection, followed by the abdominal infection(11.2%) and CNS infection(2.4%). Most ABI and ALI were caused by community-acquired pneumonia. 359 (95.5%) of 376 patients were invasively mechanical ventilated on the day of ICU admission.
By using the update SOFA criteria, we have also validated the accuracy of the brain+ chest + abdomen CT screening for infection-induced organ failure ( in the Table 3 in the appendix). The diagnostic test showed that the AUC of CT screening was 0.95 (95% CI, 0.000-1.000, p=0.000), with the sensitivity was 97.6% and and specificity was 74.6%, which was more than SIRS screening on ICU ( AUC=0.75, 95% CI, 0.525-0.981).
Among 376 sepsis, 211 were nonsurvivors and 165 were survivors. A poor outcome (56.1% dead) of sepsis and a worse outcome of sepsis with both ABI and ALI (59.4% dead) at 30 days of follow-up was confirmed by GOSE score. By the initial data on admission, the multivariate logistic analysis revealed that both ABI and ALI (OR, 3.8; 95% CI, 2.019- 7.108), systemic inflammatory storm(SIRS≥2, OR, 2.7; 95% CI, 0.999- 7.191), and lees length of stay (LOS) in ICU (OR, 0.9; 95% CI, 0.8370.958) were established as early risk factors for sepsis with worse outcomes.
In a multivariate Cox proportional hazards analysis at last step, sepsis with ABI and ALI (RR,2.5; 95% CI, 1.563-2.799), requiring mechanical ventilation (RR,0.049; 95% CI, 0.005-0.459), and elevated procaleitonin (RR,1.0; 95% CI, 1.001-1.010) were significantly associated with death.
In ICU, the dynamic profile of laboratory findings in patients with sepsis with inflammatory findings and organ failures. The data of the surviving or nonsurviving sepsis patients are described in Table 2. The laboratory findings in the survivors were from the worst value during the clinical course in the ICU, but the major critical values in the nonsurvivors were tracked before death. The main dynamic findings during sepsis progression included 6 laboratory parameters, which were from within the initial 1 days to 24 days after ICU admission at 3-day intervals. interleukin-6 (IL-6), procalcitonin , SIRS≥2, SOFA scores, GCS scores, and PaO2/FiO2 levels were higher in the nonsurvivors than in the survivors. In addition, we found that nonsurvivors were more likely to present with elevated C-reactive protein, elevated D-dimer, elevated creatinine, elevated blood glucose, and elevated lactic acid than survivors (all p<0.05).
Discussion
Sepsis-3 criteria defines sepsis as a life-threatening one or more acute organ dysfunction caused by infection. However, the leading life-threatening acute organ dysfunction have not well recognized and have also not been reported. In this large retrospective cohort, a brain+ chest + abdominal CT screening before on ICU for rapid screening infection-induced organ dysfunction was used in critically ill adult patients. We found that the AUC of the CT screening for infection-induced acute organ dysfunction before on ICU was 0.95 (95% CI, 0.0001.000) , which is greater than that the AUC (0.75) of SIRS criteria screening in the ICU, and SIRS criteria screening can only predict the suspected infection rather than organ dysfunction. According to the systemic CT screening results, we found that both ABI and ALI were strongly associated with worse outcomes in sepsis after adjusting for numerous potential confounders. These data are consistent with the hypothesis that ABI and ALI contributes to the worse outcomes in sepsis patients before on ICU.
Importantly, our study found that sepsis with worse outcomes may have complex interactions between the frequency ABI and ALI. Previous studies showed that the interactions between the ABI and ALI were related to the inflammatory storm.11-13 In the present study, severe inflammatory storm were higher in nonsurvivors than in those survivors, suggesting that the inflammation was stronger and more severe in sepsis with worse outcomes.
More importantly, we found that most of sepsis cases were mainly caused by community-acquired pneumonia and most of them with early brain edema and lung edema were confirmed by CT screening. Moreover, the results of the Cox regression analysis were also suggested this high risk of both ABI and ALI as clinically relevant risk factors for worse survival in sepsis.
In addition, our continuous observation found that these dynamic profile of inflammatory mediators and ABI and ALI in sepsis with worse survival during initial 24 days period were related to the worse survival. which is also consistent with the initial analysis from Cox regression forecast .
Several possible interpretations for ABI and ALI becoming a worse survival organ dysfunction are as following. The first, the brain itself is a leading organ of host response to infection, which is believed to be the blood-brain barrier (BBB) leakage due to an overwhelming in the pro-inflammatory cytokines and anti-inflammation factors released and resulted in severe inflammatory storm.14 The severe inflammatory storm is further responsible for these inflammation factors/toxins leak into the brain, and leading to the brain edema and cerebral ischemic injure as well as cell death.15-17 The second, jcmimagescasereports.org Volume 3 | Issue 2 | 2023 7 our data shown that most ABI had ALI /ARDS before onset illness. The brain is the most vulnerable to hypoxia and oxidative stress caused by severe inflammatory storm.18,19 Moreover, an early postmortem brain MRI findings confirmed that ALI/ ARDS play pivotal roles in the development of brain edema.20 The mechanisms of inflammation may be related to the angiotensin conversion enzyme 2 (ACE2) involved inflammatory response, leading to BBB leakage and inflammatory storm.21,22 In addition, massive cytokines ( including interleukin-6 and tumor necrosis factor alpha (TNFα) lead inflammation-derived injurious storm ( i.e; cytokine storm). 9,17,23 Cytokine storm can cause devastating inflammatory conditions, which include MODS.16,20 The previous studies indicated that sepsis with MODS have always existed an ABI and ALI,17,21-23 and that patients who were initial only with septic shock or liver failure or kidney failure can also rapidly be progressed to either ABI or ALI.16,24,25. Thus, our study showed that both ABI and ALI contributed to a high risk of death in patients with sepsis. Notably, our findings confirmed the evidence of a statistical interaction between the ABI and ALI both and mechanical ventilation on the risk for death in sepsis.Previous studies showed that requiring mechanical ventilation was commonly used in the management of the critically ill patients, which can induce an inflammatory response and involved in MODS.11-13 Our study was powered to support an interaction between the effects of ABI and ALI both and mechanical ventilation on worse survival in sepsis. Recent evidence suggests that requiring mechanical ventilation may increased the risk of ALI.12,26,27 Previous studies showed that inflammation factors had been recognized as a marker of infection and related to the severity of the disease.28-30 Especially, elevated procalcitonin was found to be significant predictors of worse prognosis in patients with sepsis.29,30
The strengths of this study include large samples and fully validated screening tools, that is, using brain + chest + abdominal CT scans before ICU to screen sepsis and predict the outcomes. It is clear that the leading life-threatening ABI and ALI is a clinical related risk factor for the worse survival rate of septic patients.
Some limitations of our study have to be addressed due to retrospective analysis. First, we use a well-validated tool for sepsis, but the current sample of sepsis was from a single center and may have selection bias. However, this hospital ICU is a unique regional ICU with an emergency center ( with 10 ambulances) that is responsible for all critically ill referrals in this area. Thus, we believe that this sample does not have a large bias. Second, some patients were excluded because patients who were in ICU length of stay less 1 day or without medical data due to death in initial 24 hours in ICU. Thus, sepsis events may be still underreported. Third, some sepsis patients with severe persistent inflammatory storms may have undetermined infection sites other than in lungs. A diagnosis of CNS infection may be missed because CT screening cannot replace MRI and lumbar puncture examination. In addition, although the prognosis for sepsis is was related to inflammatory storm, requiring mechanical ventilation, and elevated procalcitonin , further prospective studies of some causal links is necessary.
Conclusions
This study highlights a previously unreported the brain + chest + abdominal CT scans before on ICU as a new screening tool for infection/sepsis can early identified the leading life-threatening brain and lung failure and potential worse outcome. A cognition of this issue facilitate for sepsis patients timely care to improve outcome
Abbreviations ICU: intensive care unit; CT: computed tomography; GCS:: Glasgow Coma Scale; SOFA: Sequential [sepsis-related] Organ Function Assessment; ARDS:adult respiratory distress syndrome; IMV: invasive mechnical ventilation; LOS: length of stay; IQR: interquartile range, MODS: multiple organ dysfuunction syndrome.
Funding: This work is supported by a grant from the Medical Research Council and the Affiliated Shuyang Hospital of Xuzhou Medical University (from the National Clinical Key Specialty Construction Project (2019-0019-N -0002), China.
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author' Contributors: TDM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.TDM, WGS, WSD, FZD, WYW, Wy ,and ZJJ were responsible for drafting the manuscript.
Ethical approval and consent to participate: The Ethical committee on Clinical Research of Shuyang Hospitat of Xuzhou Medical University, China, approved the study. The study was in full compliance with the Helsinki declaration and written informed consent was obtained from the patient's nearest relative or a person who had been designated to give consent on admission of the patient.
Consent For publication: Not Applicable
Declaration of Interests: No potential conflicts of interest were reported For all .authors
Acknowledgments: We would like to thank everyone who contributed to the study, namely, the nurses and physicians who recorded the patient data and the related senior experts for reviewing the medical records in the ICU.
References
- Mairi Ziaka,Aristomenis Exadaktylos, et al. Brain-lung interactions and mechanical ventilation in patients with isolated brain injury. Crit Care,2021,25:358:
- Ségolène Mrozek,Jean-Michel Constantin,Thomas Geeraerts, et al. Brain-lung crosstalk: Implications for neurocritical care patients. World J Crit Care Med,2015,4:163-178
- Oddo M, Taccone FS.How to monitor the brain in septic patients? Minerva Anestesiol。2015 Jul;81(7):776-88.
- Tobias Cronberg, David M Greer, Gisela Lilja, et al. Brain injury after cardiac arrest: from prognostication of comatose patients to rehabilitation. Lancet Neurol 2020; 19:611-622
- Westphal GA, Pereira AB, Fachin SM, et al. Characteristics and outcomes of patients with community-acquired and hospital- acquired sepsis. Rev Bras Ter Intensiva. 2019;31(1):71-78.
- Laura Evans, Andrew Rhodes, Waleed Alhazzani, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med, 2021, 47:1181-1247
- Ceccni M, Evans L, Levy M, Rhodes A. Sepsis and septic shock.Lancet.2018; 392:75-87.
- Bone RC. Toward a theory regarding the pathogenesis of the systemic inflammatory response syndrome: what we do and do not know about cytokine regulation. Crit Care Med. 1996; 24: 163-172.
- David C. F, Carl H. J. Cytokine Storm. N Engl J Med 2020; 383:2255-2273.
- Lindsay Wilson,Kim Boase,Lindsay D Nelson, et al. A Manual for the Glasgow Outcome Scale-Extended Interview. J Neuro- trauma, 2021,38:2435-2446.
- Paolo Pelosi and Patricia RM Rocco。The lung and the brain: a dangerous cross-talk. Crit Care .2011 ;15:168
- Mairi Ziaka,Aristomenis Exadaktylos, et al. Brain-lung interactions and mechanical ventilation in patients with isolated brain injury. Crit Care,2021,25:358
- Ségolène Mrozek,Jean-Michel Constantin,Thomas Geeraerts, et al. Brain-lung crosstalk: Implications for neurocritical care patients. World J Crit Care Med,2015,4:163-178
- Shulyatnikova T, Verkhratsky A. Astroglia in sepsis associated encephalopathy. Neurochem Res.2019 Feb 18.
- Shay Brikman, Amir Bieber, Guy Dori..The Hyper- Inflammatory Response in Adults with Severe COVID-19 Pneumonia Differs from the Cytokine Storm of Hemophagocytic Syndrome. Isr Med Assoc J. 2020;22(8):505-513
- Sharshar T, Carlier R, Bernard F, et al., Brain lesions in septic shock: a magnetic resonance imaging study, Intensive Care Medicine,2007; 33:798–806
- Dal-Pizzol F, Tomasi CD, Ritter C. Septic encephalopathy: does inflammation drive the braincrazy? 2014,Rev Bras Psiquiatr 36:251 -258.
- Daniel R Johnson, Christina L Sherry, Jason M York, et al. Acute hypoxia, diabetes, and neuroimmune dysregulation: converging mechanisms in the brain. Neuroscientist,2008,14:235-9.
- Figen Esen, Günseli Orhun,bPerihan Özcan,bet al. Diagnosing acute brain dysfunction due to sepsis. Neurological Sciennces.2019;https://doi.org/10.1107/s10072-019-04069-x
- Coolen Tim, Lolli Valentina, Sadeghi Niloufar, et al. Early postmortem brain MRI findings in 19 non-survivors. Neurology. 2020; 95:e2016-e2027.
- Gaddam RR, Chambers S, Bhatia M. ACE and ACE2 in Inflammation: A Tale of Two Enzymes. Inflamm Allergy Drug Targets. 2014;13(4):224-34.
- Sodhi CP, Nguyen J, Yamaguchi Y, et al. A Dynamic Variation of Pulmonary ACE2 Is Required to Modulate Neutrophilic Inflammation in Response to Pseudomonas aeruginosa Lung Infection in Mice.J Immunol. 2019 1;203(11):3000-3012.
- Masae Iwasaki,Junichi Saito,Hailin Zhao,et al. Inflammation Triggered by SARS-CoV-2 and ACE2 Augment Drives Multiple Organ Failure of Severe COVID-19: Molecular Mechanisms and Implications. Inflammation. 2021;44:13-34。
- Aaron B O, Irene L, Elio A,et al. Altered liver function in patients undergoing veno-arterial extracorporeal membrane oxygenation (ECMO) therapy. Minerva Anestesiol 2017;83:255 - 265
- Edward D Siew, William H Fissell, Christina M Tripp, et al. Acute Kidney Injury as a Risk Factor for Delirium and Coma during Critical Illness. Am J Respir Crit Care Med. 2017; 195:1597-1607.
- Kumar. Toll-like receptors in sepsis-associated cytokine storm and their endogenous negative regulators as future immuno- modulatory targets. Int Immunopharmacol 2020; 89 Pt 107087.
- Purnema Madahar,Jeremy R Beitler, et al. Emerging concepts in ventilation-induced lung injury. F1000Res 2020:9
- Yeon Joo Jeong, Bo Da Nam, Jin Young Yoo, et al. Prognostic Implications of CT Feature Analysis in Patients with COVID-19: a Nationwide Cohort Study.J Korean Med Sci , 2021, 36 :e51.
- Heper Y, Akalin E H, Mistik R, et al.;Evaluation of serum C-reactive protein, procalcitonin, tumor necrosis factor alpha, and interleukin-10 levels as diagnostic and prognostic parameters in patients with community- acquired sepsis, severe sepsis, and septic shock. Eur J Clin Microbiol Infect Dis . 2006;25: 481-91.
- Ian Huang,Raymond Pranata,Michael Anthonius Lim, et al. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis . 2020;14:1753466620937175.

