Review Article - Volume 3 - Issue 2
Bonding in orthodontics and Role of different types of brackets – A Literature review
Harikrishnan B1; Anil Kumar2; Jibin Joy Daniel3; Asjad Nizar4
1Post graduate student, AJ Institute of Dental sciences, Mangalore.
2Reader, Department of Orthodontics, AJIDS, Mangalore.
3Assistant Professor, Department of Orthodontics, PCODS, Kerala.
4Post graduate student, AJ Institute of Dental sciences, Mangalore.
Received Date : Feb 23, 2023
Accepted Date : Mar 29, 2023
Published Date: April 05, 2023
Copyright:© Anil Kumar 2023
*Corresponding Author : Anil Kumar, Reader, Department of Orthodontics, AJIDS, Mangalore.
Email: drharikrishnanb007@gmail.com
DOI: Doi.org/10.55920/2771-019X/1410
Abstract
Bonding is an important development in the field of Orthodontics. From the inception of fixed appliance orthodontic treatment, brackets traditionally have been welded to gold or stainless-steel bands. At present, direct bonding is the method of choice for attaching orthodontic appliances. Bonding is based on the mechanical locking of an adhesive to irregularities in the enamel surface of the tooth, and to mechanical locks formed in the base of the orthodontic attachment.
Key words : Recent advances in bonding; Bonding in orthodontics; Adhesion.
Introduction
The introduction of bonding to orthodontics added a new dimension to fixed appliance therapy. With a considerable reduction in the need for banding teeth, there was an improvement in patient comfort, esthetics and oral hygiene maintenance. The incidence of caries was reduced as well as chair side time and there were no inter proximal spaces left after finishing the treatment.
Bonding of bracket to enamel has been critical issue in orthodontics research. Since the significance of achieving a stable bond between a tooth and its bracket was obvious from the outset. Biomechanical principles required a relatively inelastic interface that would transfer a load applied to the bracket, due to engagement of an activated archwire, to the tooth without exceeding its bond strength.
The introduction of the acid etch bonding technique has led to dramatic changes in the practice of orthodontics. Bonding is a technique sensitive procedure, and moisture is cited as the most common cause for bond failure. Contamination causes plugging of porosities caused by acid etching and a reduction in surface energy. Thus, the penetration of the resin is impaired, and the micro mechanical retention is compromised
History
Buonocore in 1955,11 was the first to demonstrate that bonding of acrylic restorative material was substantially increased by conditioning the enamel surface with 85% H3PO4 for 30 seconds.
In 196512was the first to apply these findings and bonded plastic brackets with an epoxy resin after etching with 40% H3PO4 for 60 seconds.
Mitchell in 196713 described a successful, although limited clinical trial using black copper cement and gold direct attachment.
Smith in 196814 introduced zinc polycarboxylate cement and bracket bonding with this cement was reported.
Miura in 197115 described an acrylic resin Orthomite using a modified trialkyl borane catalyst that proved to be particularly successful for bonding plastic brackets and for enhanced adhesion in the presence of moisture.
Most of the resins used in orthodontics presently are modifications of the Bowen’s resin. The modifications are mainly in the physical properties such as viscosity of the materials to achieve optimal penetration of the resin into the etched enamel spaces which enhanced the bond strength and increased the dimensional stability by cross-linking.
Role of brackets in bonding
Brackets
Three types of attachments are presently available for orthodontic bracket bonding: plastic based, ceramic based and metal based (Stainless Steel, Gold coated and Titanium).
Plastic Brackets
Plastic brackets are made of polycarbonate and are used mainly for esthetic reasons. Pure plastic brackets lack strength to resist distortion and breakage, wire slot wear, uptake of water, discoloration and need for compatible bonding resin. Such plastic brackets may be useful in minimal force situation and for treatment of short duration. New types of reinforced plastic brackets with and without steel slot inserts have presently been introduced.
Ceramic Brackets
Theoretically, porcelain brackets made of aluminium oxide could combine the esthetics of plastic and the reliability of metal brackets. Two forms are currently available7.
- Polycrystalline (GAC Allure, Transcend2000)
- Monocrystalline (‘A’ Company Starfire)
Both polycrystalline and monocrystalline brackets resist staining and discoloration.
Ceramic brackets bond to enamel by two different mechanisms.
- Bonding by means of a silane coupling
- Chemical Mechanical retention via indentations and undercuts in the
Metal Brackets
Although, not as esthetically pleasing as ceramic and plastic brackets, small metal attachments are an improvement over bands.
Metal brackets rely on mechanical retention for bonding and mesh gauge is the conventional method of providing retention. Photo etched recessions on machined undercuts are also available.
The base of the bracket must be small (not smaller than the bracket wings because of strength reasons and danger of demineralization around the periphery) as it avoids gingival irritation and should be designed to follow tissue contour along the gingival margin.
Corrosion of metal brackets is a problem and black & green stains have appeared with bonded stainless steel attachments.
Because of the corrosion susceptibility of stainless steel, interest is growing in the use of more corrosion – resistant and biocompatible bracket metals such as Titanium.
Gold-Coated Brackets (Gold n Braces Inc.)
Recently gold coated steel brackets have been introduced and rapidly gained popularity, particularly for maxillary posterior and mandibular anterior and posterior regions.
In the lack of entirely satisfactory tooth-colored brackets, these brackets may be regarded as an esthetic improvement over stainless steel attachments as they are neater and more hygienic than ceramic alternatives.

these brackets may be regarded as an esthetic improvement over stainless steel attachments as they are neater and more hygienic than ceramic alternatives.
Recent advances in orthodontic bonding system
Decrease in curing time and increase in speed of the procedure
L.E.D Light emitting diode Visible light curing units is an important part of modern dentistry. Bonding with a light activated adhesive system is popular because the extended working time allows for precise bracket placement. Once the bracket is situated at the desired location a rapid command set is accomplished through photo activation.
Barghiet al44 measured the irradiance of 209 visible light curing units for 122 private dental offices and found that 45% had an output less than 200mW/cm2. 65% had an output less than 300 mW/cm2.
Research has demonstrated that irradiance values of at least 300mW/cm2 are necessary to adequately cure resin composite. However even 300mW/cm2 might not always be adequate.
Laser etching of enamel for direct bonding
Orthodontic application of laser treatment was based on the previous hard tissue studies with lasers. Laser irradiation of enamel causes surfaces roughening and irregularity similar to that of acid etching to a depth of 10-20µm. In effect the etching is through a process of continuous vaporization and microexplosion and resulting from vaporization of water trapped in the hydroxyapatite matrix.
Self-etching primer
A unique characteristic of some new bonding agents is that they combine the conditioning and the priming agents into a single acidic primer solution for simultaneous use on both enamel and dentine. This can lead to an improvement in both time and cost effectiveness for the clinician as well as ease of bonding in difficult situations.
Moisture insensitive primer
One of the major disadvantages of direct bonding has been the need for moisture control. The conventional composites are hydrophobic in nature and any moisture contamination prevents the polymerization of the composites. To counteract this problem moisture insensitive primer and hydrophilic resin system have been developed.
GIC light cure
In1972Wilson and Kent58 formulated a new translucent cement for dentistry, i.e. GIC which was a hybrid of silicate and poly carboxylate cement and could bond to both enamel and dentin. The GIC were hydrophilic in nature and had an advantage of fluoride release. In 1995 Silverman introduced light cure GIC for orthodontic bonding. He recommended a no-etch technique for bonding and claimed it to bond satisfactorily in the presence of moisture. But other studies showed relatively poor bond strength compared with composite resin.
Sure smile process
Recent advances in computer management, 3D imaging of dentition, manipulation of complex 3D data and robotics have resulted in new approach totreatment40. A patient centered practice is one that delivers high quality care with minimum amount of patient discomfort, compliance demand and chair time and completes treatment on time, in as short period as possible.
Discussion
Comparative assessment of light- cured resin modified glass ionomer and composite resin adhesives: The ideal adhesive system is one that prevents decalcifications and has sufficient bond strength to withstand untimely impact forces on bonded brackets. The purpose of this investigation was to study and compare the bond strengths and adhesive remnant indexes of light-cured resin-modified glass ionomer and conventional resin adhesives. A new light-cured resin-modified glass ionomer adhesive was compared with the conventional adhesive systems. The effects of the new adhesive, with a system of etching and using adhesive promoters on the tooth enamel, as well as micro etching the brackets, were analyzed
Conclusion
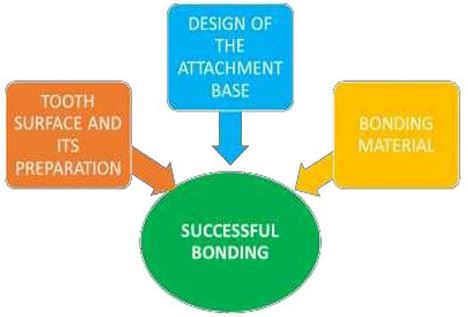
Successful bonding – attention to 3 components of the system:Today, adhesive resins, direct bonding, and light curing unit are a very important part of the modern orthodontist’s armamentarium. Our distinguished profession would not have been popularized without the application of direct bonding and advances in the material science. Similar to any other material, composite resins and bonding have their particular benefits and drawbacks. Beyond a doubt, modern orthodontists need to have a thorough knowledge and comprehension of the materials available so that they can choose the best product available for their particular needs and to make the best use of them.
Case presentation
- Theodore Eliades : Orthodontic materials research and applications: Part 1. Current status and projected future developments in bonding and adhesives. Am J Orthod Dentofacial Orthop. 2006,130;445-451.
- Proffit WRaF, H.W. & Sarver, D.M (2007). Contemporary orthodontic appliances. In: Contemporary orthodontics. J Dolan editor. 4 ed. St. Louis, USA: Mosby Elsevier; pp. 395-430.
- Jenkins TS. Adhesives in Orthodontics: Are We Pushing the Envelope in the Right Direction? Seminars in Orthodontics. 2005 Jun 1;11(2):76–85.
- Centre T. bonding: bonding in orthodontics [Internet]. bonding. 2007 [cited 2019 Jun 19].
- Themes UFO. 10 Orthodontic Adhesive Resins [Internet]. Pocket Dentistry. 2015 [cited 2019 Jun 19].
- Kloukos D, Eliades T. Bisphenol A and orthodontic materials. In: Orthodontic Applications of Biomaterials [Internet]. Elsevier; 2017 [cited 2019 Jun 19]. p. 207–19
- Yadav J, Mehrotra P, Kapoor S, Mehrotra R. Basis of orthodontics-bonding – A review. International Journal of Dental Science and Research. 2013 Jan 1;1(1):28–33.
- Hormati, A. A., J. L. Fuller, and G. E. Denehy. Effect of contamination and mechanical disturbance on the quality of acid etched level. J Am Dent Assoc 1980. 100:34–38.
- Rajagopal R, Padmanabhan S, Gnanamani J. A Comparison of Shear Bond Strength and Debonding Characteristics of Conventional, Moisture-Insensitive, and Self-etching Primers In Vitro. The Angle Orthodontist. 2004 Apr 1;74(2):264–8.
- Grandhi RK, Combe EC, Speidel TM. Shear bond strength of stainless steel orthodontic brackets with a moisture-insensitive primer. American Journal of Orthodontics and Dentofacial Orthopedics. 2001 Mar 1;119(3):251–5.

