Clinical Image - Volume 3 - Issue 3
Pneumothorax in pulmonary histiocytosis X syndrome
Rebeca Tenajas1*; David Miraut2
1Family Medicine Department, Arroyomolinos Community Health Centre, Spain.
2Advanced Healthcare Technologies. GMV, Tres Cantos, Spain.
Received Date : Mar 29, 2023
Accepted Date : April 28, 2023
Published Date: May 05, 2023
Copyright:© David Miraut 2023
*Corresponding Author : David Miraut, Advanced Healthcare Technologies. GMV, Tres Cantos, Spain.
Email: dmiraut@gmv.com
DOI: Doi.org/10.55920/2771-019X/1432
Abstract
Pulmonary Langerhans' cell histiocytosis (PLCH) represents an uncommon interstitial lung clinical disorder with unpredictable clinical presentation and outcome. The precise incidence of pulmonary LCH is unknown, although it has been estimated as about two cases per million yearly in adults. Some patients take a long time to be correctly diagnosed because of its rarity. In the present clinical image report, we describe a rather unusual case of a smoker man with PLCH presented with pneumothorax.
Keywords: Langerhans cell histiocytosis (LCH), Histiocytosis X, Neumothorax
Discussion
A previously healthy 21-year-old man was admitted to the emergency department due to severe respiratory distress. A chest X-ray was requested, it showed a tension pneumothorax of the left hemithorax, which required surgery for treatment. As a personal history, this patient was a smoker of 5 cigarettes a day for 3 years. In the contralateral hemithorax, a diffuse nodular interstitial pattern was found, leading to the decision to request an additional chest Computed Tomography (CT). An extensive analytical study was carried out with negative results for sputum culture, negative Mantoux, complete blood count (CBC), biochemistry and urine without alterations. Negative HIV serology, positive IgG mycoplasma pneumoniae antibodies, negative antinuclear antibodies, negative antineutrophil cytoplasm antibodies (ANCA). The image in the CT-thorax raised the clinically suspicion for the presence of a pulmonary histiocytosis.
Langerhans cell histiocytosis (LCH) or Histiocytosis X is a rare condition resulting from the abnormal histiocytic proliferation. These cells infiltrate the tissues forming multinucleated giant cells that constitute granulomas with eosinophils, which manifest as lesions in multiple or single organs, such as the lungs, lymph nodes, pituitary gland, liver, thyroid, bones and skin [1]. Pulmonary Langerhans cell histiocytosis (PLCH) is a unique variant of LCH in that it occurs almost exclusively in cigarette smokers, that results in the development of nodular and cystic lung lesions, making individuals susceptible to pneumothorax [2]. The progression of LCH is unpredictable and can range from continuous progression, despite the use of aggressive chemotherapy, to stabilization with or without relapses, and even spontaneous and asymptomatic remission.
The CT image was the key to perform a differential diagnosis with other processes such as lymphangioliomyomatosis, sarcoidosis, silicosis, farmer's lung. The CT scan image (figures 1 and 2) demonstrates the presence of multiple thin-walled pulmonary cystic lesions predominantly distributed throughout both upper lobes, accompanied by small isolated nodular opacities, also predominantly observed in the upper lobes. The cystic involvement is diffuse, yet spares the costophrenic and cardiophrenic sinuses. Due to the location of the lesions and the presence or absence of nodules in these processes, it was identified as a histiocytosis X case. Later, diagnosis was confirmed histologically by tissue biopsy.
Given the rapid diagnostic based on the image, the patient could be treated immediately and his respiratory function tests were not altered. However, this condition is usually related to a marked reduction in oxygen diffusion, airflow limitation, and reduced physical performance. It is a persistent and progressive disease, the possibility of death due to respiratory failure affects 10% of patients and it is increased in the case of recurrent pneumothorax. Treatment includes smoking cessation and corticosteroids in case of disease progression.
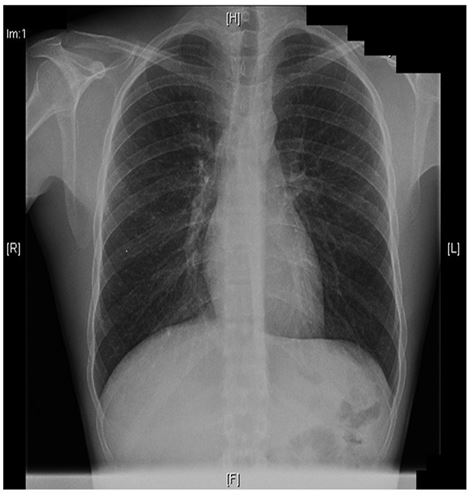
Figure 1: Thoracic CT Frontal view.
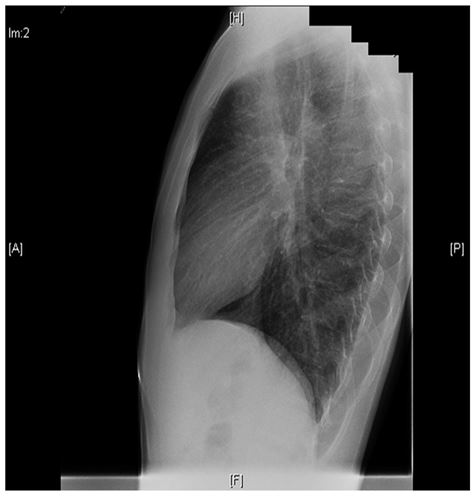
Figure 2: Thoracic CT Lateral view.
Author’s Contributions
All authors contributed to this work. All authors have read and approved the final version of the manuscript.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Funding sources
The authors are independent researchers, and they have no funding sources.
References
- Girschikofsky M, Arico M, Castillo D et al. Management of adult patients witch Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013; 8: 1-11.
- Juvet, Stephan. Rare lung diseases III: Pulmonary Langerhans' cell histiocytosis. Canadian Respiratory Journal. 2010; 17 (3): 55-62.

