Research Article - Volume 3 - Issue 3
Psoriasis in children: Study of 463 patients
Fouzia Hali; Rkia Ajaaouani*; Fatima zehra El Fatoiki; Soumya Chiheb
Dermatology-Venerology Department, Ibn Rochd hospital university, Casablanca, Morocco.
Received Date : Mar 31, 2023
Accepted Date : May 01, 2023
Published Date: May 08, 2023
Copyright:© Rkia Ajaaouani 2023
*Corresponding Author : Rkia Ajaaouani, Dermatology-Venerology Department, Ibn Rochd hospital university, Casablanca, Morocco.
Email: ajaaouani.rkia@gmail.com
DOI: Doi.org/10.55920/2771-019X/1433
Abstract
Objective: To illustrate the epidemiological and clinical features of psoriasis in children.
Methods: Retrospective study of patients, aged less than 18 years with a clinical and histopathological diagnosis of psoriasis, over a period of 11 years (2009-2020).
Results: Four hundred and sixty-three patients with psoriasis were enrolled, representing 5, 6 % of the paediatric dermatology outpatients. The mean age of onset was 6 years, with a predominance of the 7-12 year age group. The initial lesions were erythemato-squamous plaques in 79% of cases. The predominant topography was the scalp (215 cases: 46.4%). Classical plaque psoriasis was the most frequent type of psoriasis at the time of presentation (n=206; 44.5%). According to the psoriasis activity and severity index (PASI), a mild form (PASI 0-10) was reported in 363 patients and moderate to severe form (PASI> 10) in 100 cases. Topical treatment with dermocorticoids was indicated in all patients, calcipotriol in 10 cases, topical calcineurin inhibitor in 3 patients and balneo-phototherapy in 23 patients. In 29 children (6.3%), systemic therapy was required, 24 patients received retinoid, 12 patients methotrexate, 3 patients cyclosporine and four patients Secukinumab.
Conclusions. Our findings differ from those of previous studies in that they show a later onset, less frequent involvement of the face, infrequent guttate lesions, more frequent involvement of the soles of the feet, less frequent family history and more frequent severe forms.
Keywords: Psoriasis, children, plaque psoriasis, paediatric psoriasis
Introduction
Psoriasis is a common skin disease in children and adults; it is an immune-mediated inflammatory skin disease, clinically characterized by erythematous papules and plaques covered with silvery scale. It is associated especially in children with physical and psychological burden [1]. Both genetic and environmental factors interact to precipitate the development of psoriasis [2]. Estimates of the total prevalence of psoriasis in various parts of the world range from 0.1 to 3% [3]. Although its true incidence in children is unknown, psoriasis commences by the age of 15 years in 30% of patients and, therefore, is an important disorder in the paediatric age group [4]. The aim of this study was to illustrate the epidemiological and clinical features of psoriasis in children through a retrospective study.
Materials and Methods
We conducted a retrospective study of patients, aged less than 18 years with a clinical and histopathological diagnosis of psoriasis, over a period of 11 years (2009-2020). Recorded data included age, gender, disease duration, clinical variant, nail involvement, type of treatment, and family history of psoriasis. Microsoft® excel program was used for analysis.
Results
Of twelve thousand five hundred patients having consulted, four hundred and sixty-three patients with psoriasis were enrolled, representing 5, 6 % of the paediatric dermatology outpatients. The mean age of onset was 6 years (range 1 month to 17 years), with a predominance of the 7-12 year age group, and the sex ratio H/F was 0.75:1. Familial psoriasis was present in 12.5% of children and 13 patients had a history of atopic dermatitis (2,8%). Seventy-nine patients had triggering factors, including streptococcal infection (9.2%), stress (2.1%), and trauma (1.4%). The initial lesions were erythemato-squamous plaques in 79% of cases. The predominant topography was the scalp (215 cases: 46.4%). Classical plaque psoriasis (Fig.1) was the most frequent type of psoriasis at the time of presentation (n=206; 44.5%), and the overall frequency of the different types of psoriasis is shown in ( Table 1). Palmoplantar keratoderma was noted in 35 patients, and nail involvement in 23 cases. According to the psoriasis activity and severity index (PASI), a mild form (PASI 0-10) was reported in 363 patients and moderate to severe form (PASI> 10) in 100 cases. Topical treatment with dermocorticoids was indicated in all patients, calcipotriol in 10 cases, topical calcineurin inhibitor in 3 patients and balneo-phototherapy in 23 patients. In 29 children (6.3%), systemic therapy was required, 24 patients received retinoid, 12 patients methotrexate, 3 patients cyclosporine and four patients Secukinumab.
Table 1: Types of psoriatic lesions at the time of presentation.
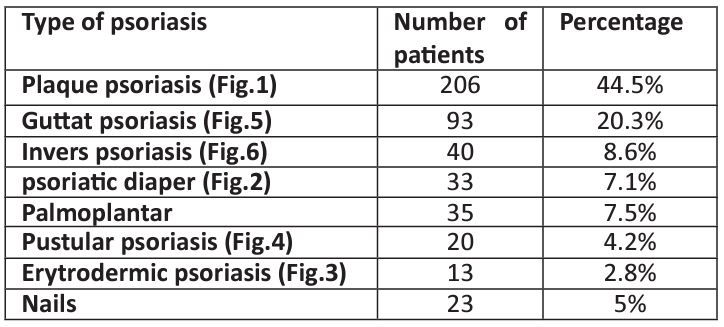
Table 2: Comparison of present study with previous studies.
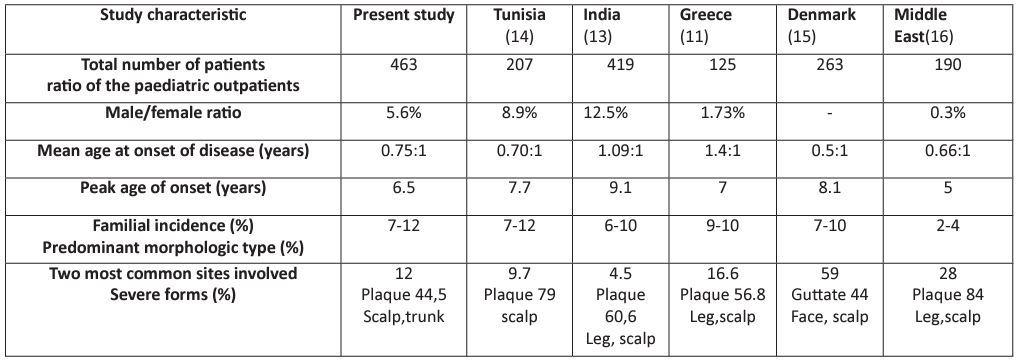

Figure 1: Extended plaque psoriasis.

Figure 2: Psoriatic diaper with plaque psoriasis.

Figue 3: Erytrodermic psoriasis.

Figure 4: Pustular psoriasis.

Figure 5: Guttat psoriasis.

Figure 6: Invers psoriasis.
Discussion
Psoriasis is a multifactorial papulosquamous disorder common in paediatrics, the prevalence of childhood psoriasis varied depending on the population. Estimates reported from literature range from 0% to 2.1%, the highest values were from European studies, Italy (2.1%), Germany (1.3%) and UK (1.3%) compared to low prevalence in Taiwan (0%) and Egypt (0.05%)[5–9]. However, the proportion of psoriatic children in outpatient paediatric dermatology varies between countries, in our series it is 5.6%, lower than in India and Tunisia and higher than in Greece and the Middle East (table 2). Positive family history was recorded in 12% of our patients however; there is a difference between the different countries. A high incidence was found in Denmark and the Middle East while a low incidence was found in India, Tunisia and Greece (table 2). The large variation reported in family history of psoriasis may in part be due to genetic differences between ethnic populations [10]. In line with what has been reported in the literature, we also found a slight predominance of females, with a male: female ratio of 0.75:1. In contrast, the Greece [11] study showed a male predominance. This female predominance seen in the prevalence of childhood psoriasis is the opposite of what is commonly observed in adults [12]. There is a large discrepancy between studies regarding the age of onset of psoriasis. In our study, the mean age was 6 ±5 years with a predominance of the 7-12 year age group. Our results are broadly in line with studies from Tunisia, Denmark and India, in which most children had an onset of disease between the ages of 8 and 12 years [13-15] . In contrast, reports from the Middle East demonstrate onset of the disease in the majority of the children before 5 years of age [16]. Despite the fact that stress and infections are the most common triggers, their incidence in our patients was much lower than that reported by other [17]. Plaque-type lesions are the most prevalent variety in this study, as has been observed in almost all previous studies, but the percentage varies (table 2). However, guttate psoriasis was the most common type of psoriasis in Denmark [15] and infection was reported as the most frequent precipitating factor. We speculate that, in poor or developing countries such as ours, repeated episodes of subclinical infection do not allow for the accumulation of the critical levels of streptococcal antigens [18] required to trigger guttate psoriasis. In addition, genetic and environmental factors may also play an important role, such that Moroccan children tend to have the enduring plaque form of the disease rather than the transient guttate form.
The scalp is the most frequently affected site of involvement in our patients 46, 4%, which is in agreement with the results of the other series [14,16]. Facial involvement was less frequent in our patients (2.1%). Children in our country are practically exposed to ultraviolet rays of the sun, and hence involvement of sun-exposed sites like the face is less frequent. Similarly, facial involvement was less frequent in the series of patients from India [13], Tunisia [4] and the Middle East [16], where sun exposure is more important. However, facial lesions were much more frequent in patients from Denmark [15], probably due to the lower number of sunny days. Nail changes were seen in 32% of children in the study of Nanda et al. nail pitting alone was the first sign of the disease. The most common nail change was pitting (5%) in our patients. A psoriatic diaper rash and flexural psoriasis are very frequent in Morocco as well as in Tunisia, Greece and Denmark [11,14,15]. This is explained by the fact that this area is the seat of trauma and friction and the use of western-type diapers (which are thick and of an occlusive nature because they are meant to soak and retain urine and secretions), as well as the development of a western lifestyle. The increased bacterial and fungal growth levels due to occlusion may initiate the psoriatic lesions in predisposed individual. On the other hand in India which does not use this type of western-type diapers , involvement of the diaper area was seen in only two patients [13]. The palms and soles have been reported as uncommon sites of psoriasis involvement in children. However, in our study, the palms and soles were the most common site (7, 5%) of onset after the scalp and trunk, of which some children had only plantar lesions; the results are similar to those from India where they found palmoplantar involvement in 12.8% of cases. This contrast sharply with a study in Australia, where plantar involvement was reported in only 4% of cases [19]. In India as in morocco, the habit of walking barefoot or wearing open-toed sandals is common, which leads to some degree of keberisation at these friction points [20]. This could explain the higher percentage of palms and soles involvement in both studies. Most children in our study (78.4%) had a mild form of the disease, and 21,5% of children had >20% of their skin affected by psoriasis. Comparing our results with those of other series we find that the severe forms which represent 7% is higher than that of Greece (0,8%), India (2,1%), Denmark (2,1%) and Middle East (1,57%) (Table 2).
A specific guideline for the diagnosis, management, and treatment of psoriasis are of extreme importance. However, these guidelines are still lacking in this age group. Most of the psoriasis treatments used in adults are not officially approved, for the paediatric age and require off-label prescription. Moreover, efficacy and safety studies are lacking in this population, especially with long-term follow-up and outcomes. Many biologic agents have been recently approved for the treatment of psoriasis in children, while others are currently being studied. Topical corticosteroids are the most commonly prescribed topical therapy for paediatric psoriasis. However, prescribing should be performed with prudence, taking into account the duration of the treatment and the extent of the lesions, because of the undesirable effects. Such that systemic absorption may follow extensive application of potent dermocoticoids with consequent suppression of the hypothalamus-pituitary-adrenal axis [21]. Calcipotriol is a vitamin D3 analogue, which has been shown to be beneficial in childhood psoriasis [22] ; it was used as steroid sparing in 10 children in our series. Topical calcineurin inhibitors are used as steroid-sparing options for psoriasis at high-risk sites for adverse effects in case of long-term topical steroid use (face, eyelids, flexures, fingertips/nails, anogenital region)[23]. Phototherapy was used in our series only in palmoplantar keratoderma in the form of balneophototherapy in 23 patients. Ultraviolet rays inhibit DNA synthesis and keratinocyte proliferation and induce T cell apoptosis and the production of anti-inflammatory mediators [24]. Acitretin is the second-line drug of choice suitable for children with generalized flares pustular psoriasis as intermittent rescue therapy and in case of pustular, erythrodermic or severe plaque psoriasis of older children as long-term therapy. This drug can also be associated with topical and NB-UVB phototherapy [25]. Because of the risk of premature epiphyseal closure, we used the lowest doses (0.25 – 0.6 mg/kg) in treatment of our 24 patients. Methotrexate (MTX) is an antimetabolite that modulates the immune system and inflammatory processes. Jager et al. highlighted that this drug represents an effective alternative treatment for moderate to severe paediatric psoriasis, with minor short-term side effects usually detected [26]. A good clinical response and therapeutic tolerance was noted in 12 children treated with MTX. Cyclosporine is an immunosuppressant drug approved for treatment of psoriasis in adults. As the evidence in children is limited, the lowest possible dose and the shortest treatment period were used in our 3 patients [27]. Biologics are relatively new pharmacological agents that target specific mediators of the inflammatory cascade in psoriasis, including TNF-a and IL-12/23[22]. Those molecules are theoretically lack many of the toxicities of the traditional agents, are convenient to use, requiring less frequent dosing and laboratory monitoring. All these factors should make them an attractive option for treating paediatric psoriasis. Still, concerns remain regarding their long-term safety. Hence despite the obvious advantages, these are often indicated as second-or third-line agents for refractory psoriasis in children [28]. We illustrate our experience with the use of biologics in four patients, three children who received Secukinumab and one patient with etanercept with excellent tolerance.
Conclusion:
Our findings differ from those of previous studies in that they show a later onset, less frequent involvement of the face, infrequent guttate lesions, more frequent involvement of the soles of the feet, less frequent family history and more frequent severe forms. The management of psoriasis in children differs from adults in several important respects including the emphasis on educating the family, dealing with the emotional aspects of the disease and eliminating triggering factors.
Conclusion
Our findings differ from those of previous studies in that they show a later onset, less frequent involvement of the face, infrequent guttate lesions, more frequent involvement of the soles of the feet, less frequent family history and more frequent severe forms. The management of psoriasis in children differs from adults in several important respects including the emphasis on educating the family, dealing with the emotional aspects of the disease and eliminating triggering factors.
References
- Mahé E. Childhood psoriasis. European Journal of Dermatology. 2016; 26(6): 537‑48.
- Raychaudhuri SP, Gross J. A Comparative Study of Pediatric Onset Psoriasis with Adult Onset Psoriasis. Pediatr Dermatol. mai 2000; 17(3): 174‑8.
- Relvas M, Torres T. Pediatric Psoriasis. Am J Clin Dermatol. 2017; 18(6): 797‑811.
- Rogers M. Childhood psoriasis: Current Opinion in Pediatrics. Août. 2002; 14(4): 404‑9.
- Gallus’ S. Prevalence of Atopic Dermatitis in Italian Schoolchildren: Factors Affecting its Variation.
- Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schäfer I. Epidemiology and comorbidity of psoriasis in children: Epidemiology and comorbidity of psoriasis in children. British Journal of Dermatology. 2010; 162(3): 633‑6.
- Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and Treatment of Psoriasis in the United Kingdom: A Population-Based Study. Arch Dermatol. 2005; 141(12).
- Yang YC, Cheng YW, Lai CS, Chen W. Prevalence of childhood acne, ephelides, warts, atopic dermatitis, psoriasis, alopecia areata and keloid in Kaohsiung County, Taiwan: a community-based clinical survey. J Eur Acad Dermatol Venerol. 2007.
- El-Khateeb EA, Lotfi RA, Abdel-Aziz KM, El-Shiekh SE. Prevalences of skin diseases among primary schoolchildren in Damietta, Egypt. Int J Dermatol. mai 2014; 53(5): 609‑16.
- Burden-Teh E, Thomas KS, Ratib S, Grindlay D, Adaji E, Murphy R. The epidemiology of childhood psoriasis: a scoping review. Br J Dermatol. juin 2016; 174(6): 1242‑57.
- Stefanaki C, Lagogianni E, Kontochristopoulos G, Verra P, Barkas G, Katsambas A, et al. Psoriasis in children: a retrospective analysis: Psoriasis in children. Journal of the European Academy of Dermatology and Venereology. 2011; 25(4): 417‑21.
- Hägg D, Eriksson M, Sundström A, Schmitt-Egenolf M. The Higher Proportion of Men with Psoriasis Treated with Biologics May Be Explained by More Severe Disease in Men. Bobé P, éditeur. PLoS ONE. 2013; 8(5): e63619.
- Kumar B, Jain R, Sandhu K, Kaur I, Handa S. Epidemiology of childhood psoriasis: a study of 419 patients from northern India. Int J Dermatol. 2004; 43(9): 654‑8.
- Frikha F, Mseddi M, Chaabane H, Sellami K, Bahloul E, Masmoudi A, et al. Psoriasis de l’enfant : étude rétrospective de 207 cas. Annales de Dermatologie et de Vénéréologie. 2015; 142(12): S543‑4.
- Nyfors A, Lemholt K. Psoriasis in children: A short review and a survey of 245 cases. Br J Dermatol.1975; 92(4): 437‑42.
- Al-Fouzan AS, Nanda A. A Survey of Childhood Psoriasis in Kuwait. Pediatr Dermatol. 1994; 11(2): 116‑9.
- Özden MG, Tekin NS, Gürer MA, Akdemir D, Doğramacı Ç, Utaş S, et al. Environmental Risk Factors in Pediatric Psoriasis: A Multicenter Case-Control Study: Özden et al. Pediatric Dermatology. 2011; 28(3): 306‑12.
- Valdimarsson H, Baker BS, Jónsdóttir I, Powles A, Fry L. Psoriasis: a T-cell-mediated autoimmune disease induced by streptococcal superantigens? Immunology Today. 1995; 16(3): 145‑9.
- Morris A, Rogers M, Fischer G, Williams K. Childhood Psoriasis: A Clinical Review of 1262 Cases. Pediatric Dermatology. mai 2001; 18(3): 188‑98.
- Kumar B, Saraswat A, Kaur I. Palmoplantar Lesions in Psoriasis: A Study of 3065 Patients. Acta Dermato-Venereologica. 2002; 82(3): 192‑5.
- Maibach HI, Wester RC. Issues in measuring percutaneous absorption of topical corticosteroids. Int J Dermatol. 1992; 31(s1): 21‑5.
- Megna M, Napolitano M, Balato A, Scalvenzi M, Cirillo T, Gallo L, et al. Psoriasis in Children: A Review. CPR. 2015; 11(1): 10‑26.
- Brune A, Miller DW, Lin P, Cotrim-Russi D, Paller AS. Tacrolimus Ointment is Effective for Psoriasis on the Face and Intertriginous Areas in Pediatric Patients: Tacrolimus Ointment for Facial and Inverse Psoriasis. Pediatric Dermatology. 2007; 24(1): 76‑80.
- Holme SA, Anstey AV. Phototherapy and PUVA photochemotherapy in children. Photoderm Photoimm Photomed. 2004; 20(2): 69‑75.
- Sue Lee C, Koo J. A review of acitretin, a systemic retinoid for the treatment of psoriasis. Expert Opinion on Pharmacotherapy. 2005; 6(10): 1725‑34.
- de Jager MEA, de Jong EMGJ, van de Kerkhof PCM, Seyger MMB. Efficacy and safety of treatments for childhood psoriasis: A systematic literature review. Journal of the American Academy of Dermatology. 2010; 62(6): 1013‑30.
- Bronckers IMGJ, Paller AS, van Geel MJ, van de Kerkhof PCM, Seyger MMB. Psoriasis in Children and Adolescents: Diagnosis, Management and Comorbidities. Paediatr Drugs. 2015; 17(5): 373‑84.
- Dogra S, Mahajan R. Biologics in pediatric psoriasis - efficacy and safety. Expert Opin Drug Saf. 2018; 17(1): 9‑16.

