Case report - Volume 3 - Issue 3
Cervical transpedicular irrigation and drainage in a patient with cervical spondylodiscitis after hypopharyngeal cancer treatment: A case report
Jae sin Lee1; Kyung-Soo Suk1; Ji-Won Kwon1; Seong-Hwan Moon1; Hun jin Ju1; Byung Ho Lee*1; Mahmoud Abdou2
1Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
2Department of Orthopedic Surgery, Fayoum University College of Medicine, Fayoum, Egypt.
Received Date : April 20, 2023
Accepted Date : May 03, 2023
Published Date: May 10, 2023
Copyright:© Byung Ho Lee 2023
*Corresponding Author : Byung Ho Lee, clinical professor of Orthopedic Surgery, College of Medicine, Yonsei University, Korea.
Email: bhlee96@yuhs.ac
DOI: Doi.org/10.55920/2771-019X/1435
Abstract
Cervical spondylodiscitis is a rare condition, but it is usually associated with rapid neurological deterioration so urgent surgical intervention mostly is indicated. We are presenting a case of cervical spondylodiscitis in a patient with a history of cancer hypopharynx. The patient had lateral pharyngotomy-wide excision followed by radiotherapy, but the presence of an epidural abscess made surgical intervention inevitable. Anterior cervical debridement might lead to esophageal perforation due to the extensive tissue scaring, so transpedicular irrigation and drainage technique was decided. Our emerging MPPP technique allows us to do safe and effective debridement, however, there were some concerns regarding cervical pedicle screw insertion. So, we are reporting the first case of transpedicular curettage and drainage using the freehand cervical pedicle screw insertion technique for the treatment of cervical SD. After surgery, the infection subsided with no need for further intervention. Ultimately, the transpedicular irrigation and drainage technique is effective and less aggressive treatment for cervical SD after hypopharyngeal cancer treatment.
Keywords: cervical spine, spondylodiscitis, transpedicular irrigation drainage, hypopharyngeal cancer
Abbreviations: SD: Spondylodiscitis; MPPP: Medial pedicle pivot point.
Introduction
Cervical spondylodiscitis (SD) is a rare condition, but it has the highest morbidity and mortality among infections of the spine [1]. Its incidence is increasing due to high numbers of aging, immunocompromised patients, and intravenous drug users [2,3]. Cervical SD can be managed conservatively with specific antibiotics, but in cases of epidural abscess, septicemia, kyphosis, and neurologic compromise, surgical intervention is necessary [4]. There is some evidence that cervical SD requires surgical intervention more frequently than SD in other spinal regions[5]. Adequate debridement and reconstruction with stability, sometimes with circumferential fusion, are mandatory procedures, especially if there is evidence of epidural abscess to avoid late collapse and neurological deterioration [2, 6]. In our case, using this approach was not applicable as the patient had a history of cancer of the hypopharynx that was managed by lateral pharyngotomy-wide excision, so an alternative approach, such as transpedicular curettage and drainage for thoracolumbar SD, was investigated [7]. However, as the insertion of a cervical pedicle screw is technically difficult, the use of this technique is limited. Currently, it is more common to employ cervical pedicle screws using the freehand technique in our institute [8]. Therefore, we are reporting the first cervical transpedicular curettage and drainage using the freehand cervical pedicle screw insertion technique for the treatment of cervical SD in a patient who was unable to undergo an anterior procedure due to previous cancer surgery and postoperative adjuvant radiotherapy.
Clinical presentation
A 67-year-old male patient presented with neck pain, limited range of motion, and bilateral arm pain; he had no other neurological manifestations. The patient had undergone wide excision of a cancerous hypopharynx via lateral pharyngotomy, followed by radiotherapy for one year before these most recent issues. The patient has diabetes mellitus and chronic hepatitis C. An X-ray of the cervical spine showed osteolysis and kyphosis of the C6 and C7 vertebral bodies (Figure 1 A). His erythrocyte sedimentation rate (ESR) was initially 120 mm/hr (normal range < 20 mm/hr). C-reactive protein (CRP) levels were 76 mg/L (normal range = 0–8 mg/L), and his total leukocyte count was 6.34×103/µL (normal range = 4–10.8×103/µL) with 75% neutrophils with the shift to left which means a high possibility of bacterial infection.
Magnetic resonance imaging (MRI) with contrast showed SD of both C6 and C7 with vertebral body collapse as well as paravertebral and epidural abscesses with cord compression. There was no recurrence of the primary tumor (Figure 1 B). Computed tomography (CT) showed vertebral body destruction, height loss, and retrolisthesis of C6 and C7 with soft tissue swelling (Figure 1 C).
Surgical intervention was indicated because of the epidural abscess, but the presence of the lateral pharyngotomy scar increased the risk of esophageal injury. Therefore, the patient was admitted immediately, and empirical intravenous antibiotic therapy (ceftazidime and teicoplanin) was started after consultation with the Department of infectious diseases (a CT-guided biopsy and urine, sputum, and blood cultures were analyzed first), and a cervical brace was ordered. An esophagogram was performed to ensure there was no barium leakage from the previous hypopharynx scar.
Surgery was performed after 10 days to prevent the development of neurological deterioration. Transpedicular irrigation and drainage were used to effectively debride C6 and C7 as performed for thoracolumbar SD (Figures 2 and 3) [7].
After pedicle screws were inserted into healthy vertebrae (C5–T1) using the Medial Pedicle Pivot Point (MPPP) method,[8] the pedicle track of the infected vertebrae (C6 and C7) was opened and continuously lavaged with 15 L of sterile fluids mixed with betadine. Posterolateral fusion was performed using an autologous bone graft mixed with vancomycin powder (Figures 2 and 3) [7].
Because arm pain and weakness developed postoperative, the patient underwent micro foraminotomy of C6-7 foramen seven days later. The patient experienced immediate postoperative pain relief and regained 70% of his motor strength one month later.
Blood and tissue cultures were negative for aerobic, anaerobic, fungi, and mycobacteria, so ceftazidime and teicoplanin injections were continued for four weeks [2]. Oral antibiotics were administered until inflammatory markers were negative three successive times (over 3-day intervals) and after consultation with the Department of infectious disease. CRP levels and ESR started to decline after the patient began the intravenous antibiotic therapy, even before surgical debridement, to less than 5 mg/L and 11 mm/hour, respectively, after two months.
Asymptomatic mild kyphosis occurred three months later, but good bone fusion occurred globally after six months. There was no recurrence of infection or implant failure two years after debridement; the patient returned to his daily activities two months postoperatively (Figure 4, 5).

Figure 1: (A) Preoperative X-ray showing osteolysis and vertebral body collapse. (B) MRI Cervical spine showing SD with epidural abscesses in C6 and C7. (C) CT sagittal and axial views showing col- lapse, height loss and retrolisthesis of C6 and C7.
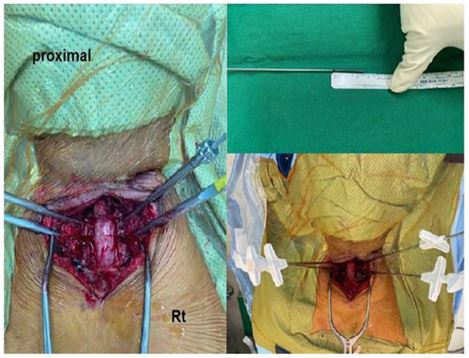
Figure 2: Intraoperative photo showing tapping of the pedicle track prior to insertion of the irrigation and drainage catheters. A mark was made 25 mm from the end of the trocar for the proper in-sertion depth through the pedicle to reach the infected vertebral body.
Discussion
Cervical SD can be a fatal condition. Death is a sequela of cervical infections due to septicemia in 3.7-5 % of cases despite advances in antimicrobial therapy and surgical modalities [4], and is almost always associated with rapid neurological deterioration [6]. Thus, rapid and effective intervention should be considered [6]. Most management strategies are tailored to each patient [1, 2], but early interventions and antibiotic therapy will lead to the best prognosis and earliest recovery [5, 6]. For adequate debridement, stable fixation, and antibiotic therapy are warranted, as insufficient management could lead to the recurrence of infection and/or implant failure [9].
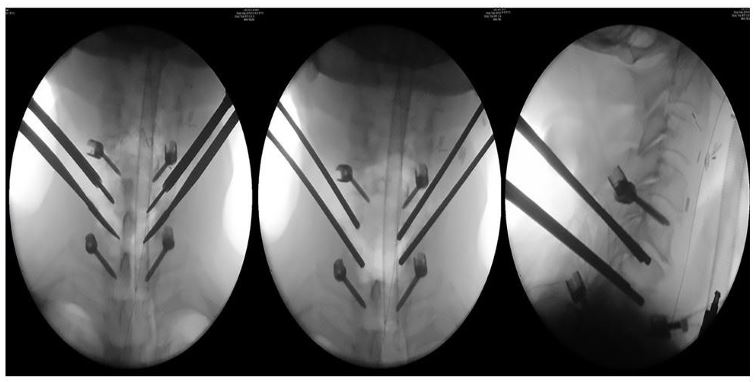
Figure 3: Intraoperative fluoroscopy images showing (A) Ap view showing pedicle screws of C5-T1 and C 6 7 pedicle track opening using pedicle finder. (B,C) AP and lateral view showing pedicle screws and suction and irrigation trocars

Figure 4: (A) Six-month follow-up X-ray showing acceptable kypho-sis with good fusion. (B) One year follow-up X-ray showing com-plete fusion with no recurrence or collapse.
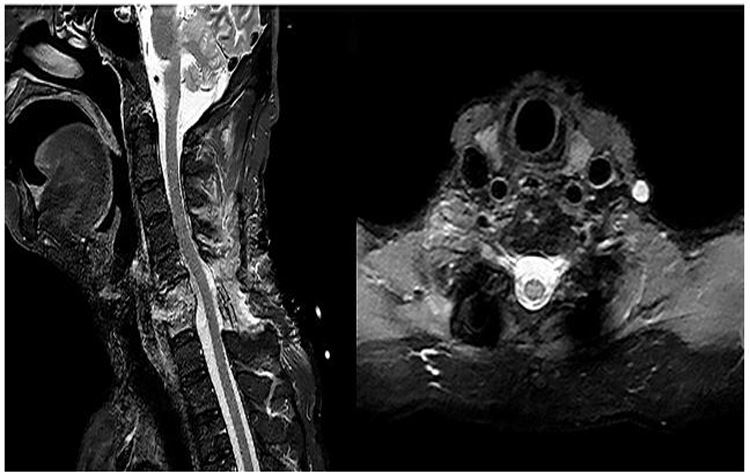
Figure 5: MRI scans one year postoperatively. (A) T2 showing the wide decompression of the thecal sac and both roots with no epi-dural abscess. (B) Post-contrast T1 showing no signs of SD, arach-noiditis, or intraspinal granulation tissue.
According to our literature review, there is a tendency for patients to receive anterior debridement and fusion only in such cases [1, 6, 10]. However, in our case, the risk of esophageal perforation was very high, as the patient had undergone wide excision of his hypopharyngeal cancer via lateral neck dissection followed by radiotherapy with extensive tissue scaring, in addition to the current infection itself, which increased the incidence of esophageal perforation. Moreover, considering the patient's history of diabetes and overall immune system, we have considered the importance of completing the treatment with rapid and less invasive surgery. Therefore, we did not want to further endanger the patient`s health [11].
A posterior laminectomy alone will not address the infected cervical bodies, so recurrence of infection and additional collapse is inevitable sequelae along with a high risk of neurological deterioration; thus, we decided to use the transpedicular irrigation and drainage technique [7, 12].
The pedicle forms a track to the infected body for adequate debridement. The use of the pedicle track in the cervical spine was not as its use in thoracolumbar vertebrae, due to neurovascular risk factors and technical difficulty, but the freehand cervical pedicle screw technique has gained popularity over the last few years in our institute. Additionally, after recent studies confirming its safety and availability even in the absence of a navigation system, we decided to perform the freehand cervical pedicle screw technique using the MPPP method [8].
Transpedicular irrigation was highly effective in the cervical bodies; intervertebral disc access allowed the adequate removal of necrotic tissue [7], and fixation of the pedicle screws provided stability for solid fusion with no recurrence or failure after two years [13].
Conclusion
Transpedicular irrigation and drainage technique is the effective and less aggressive treatment for cervical SD with an epidural abscess in high-risk patients in need of circumferential cervical intervention and in patients in whom anterior cervical debridement is contraindicated.
Consent: The study protocol was approved by the institutional review board of Severance Hospital, Yonsei University Health System, Seoul, Korea (IRB no. 3-2022-0204). The patient authorizes the publication of this manuscript.
Conflict of interest: The authors declare no conflict of interest in preparing this article.
Funding Acknowledgement: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Shousha M, Heyde C, Boehm H. Cervical spondylodiscitis: change in clinical picture and operative management during the last two decades. A series of 50 patients and review of literature. Eur Spine J. 2015; 24: 571-576.
- Tonetti DA, Eichar B, Ares WJ, Kanter AS, Hamilton DK. Should the Presence of Spondylodiscitis Alter the Surgical Treatment of Patients with Symptomatic Ventral Cervical Epidural Abscesses? An Institutional Analysis. World Neurosurg 2020; 138: e282-e288.
- Kothari MK, Shah KC, Tikoo A, Nene AM. Surgical Management in Elderly Patients with Tuberculous Spondylodiscitis: Ten Year Mortality Audit Study. Asian Spine J. 2016; 10: 915-919.
- Sharfman ZT, Gelfand Y, Shah P, Holtzman AJ, Mendelis JR, Kinon MD, et al. Spinal epidural abscess: a review of presentation, management, and medicolegal implications. Asian Spine Journal. 2020; 14: 742.
- Alton TB, Patel AR, Bransford RJ, Bellabarba C, Lee MJ, Chapman JR. Is there a difference in neurologic outcome in medical versus early operative management of cervical epidural abscesses? The Spine Journal 2015, 15: 10-17.
- Ghobrial GM, Franco D, Theofanis T, Margiotta PJ, Andrews E, Wilson JR, et al. Cervical spondylodiscitis: presentation, timing, and surgical management in 59 patients. World Neurosurg 2017; 103: 664-670.
- Lee BH, Park J-O, Kim H-S, Lee H-M, Cho B-W, Moon S-H. Transpedicular curettage and drainage versus combined anterior and posterior surgery in infectious spondylodiscitis. Indian J Orthop. 2014; 48: 74-80.
- Kwon J-W, Arreza EO, Suguitan AA, Lee S-B, Sung S, Park Y, et al. Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series. Journal of Clinical Medicine. 2022; 11: 396.
- Urrutia Escobar JO, Zamora Helo T, Campos Daziano MA. Cervical pyogenic spinal infections: are they more severe diseases than infections in other vertebral locations? 2013.
- Walter J, Kuhn SA, Reichart R, Kalff R, Ewald C. PEEK cages as a potential alternative in the treatment of cervical spondylodiscitis: a preliminary report on a patient series. Eur Spine J. 2010; 19: 1004-1009.
- Ko S-B, Park J-B, Song K-J, Lee D-H, Kim S-W, Kim Y-Y, et al. Esophageal perforation after anterior cervical spine surgery. Asian Spine Journal 2019; 13: 976.
- Lee BH, Lee HM, Kim TH, Kim HS, Moon ES, Park JO, et al. Transpedicular curettage and drainage of infective lumbar spondylodiscitis: technique and clinical results. Clin Orthop Surg. 2012; 4: n 200-208.
- Kim S-H, Kim J-h, Kwon J-W, Kim H-S, Moon S-H, Suk K-S, et al. Assessment of Biomechanical Advantages in Combined Anterior– Posterior Cervical Spine Surgery by Radiological Outcomes: Pedicle Screws over Lateral Mass Screws. Journal of Clinical Medicine. 2023; 12: 3201.

