Clinical Image - Volume 3 - Issue 3
More than an anal abscess: An atypical pancreatic pseudocyst clinical presentation
Gonçalo Guidi1*; Daniela Martins1; Fernando Próspero1; João Pinto-de-Sousa1,2
1Department of Surgery, Centro Hospitalar Trás-os-Montes e Alto Douro, R. dos Lagoeiros 43, 5000-508 Vila Real, Portugal.
2Clinical Academic Centre Trás-os-Montes e Alto Douro (CACTMAD)
Received Date : Mar 31, 2023
Accepted Date : May 04, 2023
Published Date: May 11, 2023
Copyright:© Gonçalo Guidi 2023
*Corresponding Author : Gonçalo Guidi, Department of Surgery, Centro Hospitalar Trás-os-Montes e Alto Douro, R. dos Lagoeiros 43, 5000-508 Vila Real, Portugal.
Email: gjlima@chtmad.min-saude.pt
DOI: Doi.org/10.55920/2771-019X/1436
Clinical Image
A 50-year-old man presented to the emergency department due to painful perianal swelling. Previous medical history included Sjögren's Syndrome, heart failure with reduced ejection fraction, dilated cardiomyopathy, and alcoholism. He was previously admitted to our hospital six weeks before with mild alcohol-induced pancreatitis. Gallstones were excluded. On physical examination, he presented a right anal abscess (AA) with fluctuation. The abscess was drained, and the patient was discharged, medicated with antibiotics, and referred to a General Surgery outpatient clinic. On revaluation, due to maintenance of purulent drainage, fever, and elevation of analytical inflammatory parameters, a computed tomography (CT) was performed. The image revealed a right retroperitoneal fluid collection, with 15x8x25cm, extending from the cephalopancreatic region to the retrorectal space, with densification of the right perianal and perineal region (Figure 1 and 2). These findings were consistent with a pancreatic pseudocyst (PP).
The patient was proposed to hospitalization. Intravenous antibiotic therapy and supportive measures were started. After an unsuccessful transduodenal endoscopic drainage, he underwent percutaneous drainage via the right retro colic and left transgluteal routes. The patient was unable to undergo surgery by severe cardiomyopathy and ended up dying from heart failure decompensated by sepsis refractory to therapeutic and supportive measures. In asymptomatic patients with a PP, clinical and imaging surveillance is usually sufficient as the spontaneous resolution is not uncommon. Endoscopic or percutaneous drainage is indicated for symptomatic patients, rapidly enlarging / persistent pseudocysts and infection refractory to medical treatment [1]. Surgery is indicated in the failure of conservative treatment [2].
Conflicts of Interest
The Author declares no Conflict of Interest for this article

Figure 1: Sagittal CT image reconstruction. Pancreatic pseudocyst (PP) and densification of the right perianal and perineal region (arrow).
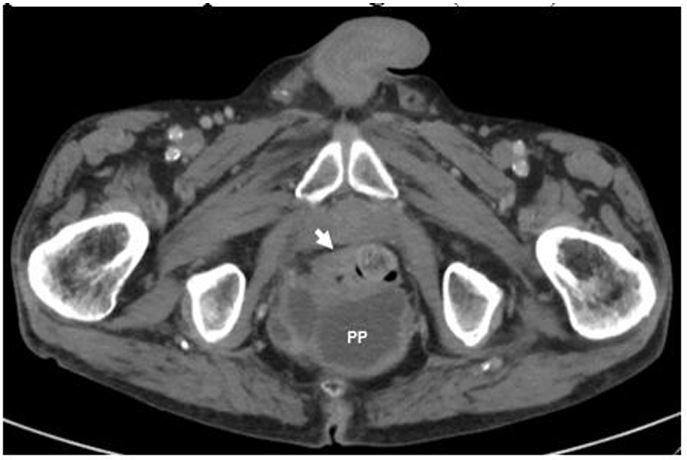
Figure 2: Axial CT image reconstruction. Pancreatic pseudocyst posterior to the rectum (PP) and densification of the right perianal and perineal region (arrow).
References
- Umapathy C, Gajendran M, Mann R, et al. Pancreatic fluid collections: Clinical manifestations, diagnostic evaluation and management. Dis Mon. 2020; 66(11): 100986. doi:10.1016/j.disamonth.2020.100986
- Matsuoka L, Alexopoulos SP. Surgical Management of Pancreatic Pseudocysts. Gastrointest Endosc Clin N Am. 2018; 28(2): 131-141. doi:10.1016/j.giec.2017.11.002

